Background and Objectives: Physician location is an important element of health care access. However, physician shortages and disparities in geographic distribution exist. This study examines physician locations, relocation patterns, and factors associated with relocating.
Methods: We used Arizona licensure data and rural-urban commuting area (RUCA) codes to identify Arizona physicians and their office or mailing address locations. Our sample included Arizona physicians estimated to be younger than 70 years of age who had an active license between in 2014 and 2019. We used multivariable logistic regression to assess physicians’ adjusted odds of relocating in Arizona by RUCA code, primary care status, age, gender, and medical education location.
Results: We identified 11,202 Arizona physicians in our sample, 33% of whom changed practice addresses within Arizona between 2014 and 2019. Primary care physicians (PCPs) in large rural areas had lower odds of relocating in Arizona (0.62, 95% CI 0.43-0.90) than PCPs in urban areas. Compared to 64–69-year-old physicians, those less than 34 and 34-43 years old had statistically higher odds of relocating within Arizona.
Conclusions: Primary care status and rurality are important factors consider to understand physician relocation patterns. We found that a substantial number of Arizona physicians relocated within Arizona between 2014 and 2019, and few of those who relocated (2%) moved to a more rural area.
Access to health care services is an important aspect of population health and well-being. For services to be accessible, they need to be affordable, proximal, timely, and delivered by usual, trusted, and capable providers. 1 Access to health care providers is limited by a variety of factors, including physician shortages. Within the health care provider workforce, physicians play a central role in health care delivery, including in many rural areas. While the role of the physician in the United States has changed as the health care system adapts to team-based care, advanced-practice health professionals, and telehealth services, ensuring a well-trained physician workforce remains an important element of access to health care services for all communities.2
Physician shortages can result from too few total physicians, an imbalance among specialties relative to health care needs and geographic maldistribution.3 Driven by an aging population, population growth, and more individuals with health insurance coverage, 4 it is estimated that by 2032, the United States will need between 21,100 and 55,200 additional primary care physicians (PCPs) and 46,900 to 121,900 total physicians.5 Since the 1970s, the number of physicians training in primary care has declined while the proportion of specialist physicians has increased.6 This imbalance has accelerated in the last 2 decades; between 2005 and 2015, specialist physicians growth was six times that of PCPs, and the share of the physician workforce represented by primary care decreased from 44% to 37%.7
Workforce distribution also varies by location. For example, in 2019, Arizona had 243 physicians per 100,000 persons, while the US median is 263.8 Within states, there are more PCPs per population in metropolitan areas—53.3 per 100,000 persons—compared to 39.8 in nonmetropolitan areas. 9 Although physicians are concentrated in population centers, PCPs are more likely than specialty physicians to work in nonmetropolitan areas.10 In Arizona, although a larger proportion of the rural workforce are PCPs, the ratio of PCPs per population remains lower in rural compared to urban areas.11 Arizona’s distribution fits with US physician workforce patterns; rural shortages are not improving, for primary care or specialist physicians. In 1991, 12.6% of physician graduates were practicing in a rural area, by 2005, only 11.4% were.12 In 2017, in metropolitan areas there were 333 physicians per 100,000 persons compared to nonmetropolitan areas with 127.13
Rural physician shortages result from multiple factors at the individual, community, and system level. Individual factors that influence the decision to enter and remain in rural practice include background, gender, and age. Historically, those with a rural background are twice as likely to work in rural practice,14 and female physicians, physicians younger than 45 years old, and those raised in metropolitan areas are more likely to leave rural practice.15 Community factors include proximity to other physicians, peer and administrative support, and community connection.16, 17 Medical education in rural areas18 and family medicine residency programs also support rural retention.19 A study of primary care physicians found that few migrated between counties over a 5-year period.20
Physician shortages and disparities in geographic distribution in Arizona make it necessary to recruit and retain physicians in rural and underserved areas. To appropriately develop and target recruitment and retention policies and programs, it is important to understand physician movement patterns within the state. We assessed Arizona physician relocation patterns in a sample that included all allopathic (MD) and osteopathic (DO) physicians with active state licenses in a 5-year period, between 2014 and 2019. Using rural-urban commuting area (RUCA) codes, we describe physician relocation patterns and report their odds of relocating within Arizona by location type.21 RUCA codes provide subcounty distinctions that allow important nuance in classifying rurality. This approach complements and expands efforts to analyze trends in physician mobility that used county-level coding of rurality.15 This is especially important in western states like Arizona where there are fewer and larger counties, some of which are geographically larger than Northeastern states.
Study Population and Data Sources
This study used Arizona Medical Board and the Arizona Board of Osteopathic Examiners physician licensure data. These boards (referred to collectively as the AMB) provide single-point-in-time data snapshots of physician licensee information in Arizona. Physicians in Arizona are required to renew their license every 2 years based on licensee birth date or by December 31. Physicians were included if they had a doctor of medicine (MD) or doctor of osteopathic medicine (DO) degree and had a registered medical license in Arizona in 2014 and 2019. This research was reviewed and approved by the University of Arizona Institutional Review Board.
Measures
Outcome Variables. Licensure data are publicly available by request to the state licensing boards and include limited information on physician location (office or mailing address), demographics, and educational background. The primary outcome for this study is physician relocation (Y/N). Physicians with different address zip codes in 2014 and 2019 were coded as having relocated. To understand relocation patterns within Arizona, we associated the physician address zip code with a RUCA code using the United States Department of Agriculture, Economic Research Service (USDA) zip to RUCA crosswalk file.22 Once we identified RUCA codes for the physician address, we generated relocation patterns by comparing RUCA code types (did not relocate, relocated to a more urban area category, relocated within same RUCA category, relocated to a more rural area category).
Independent Variables. Independent variables included age, physician specialty, undergraduate medical education (UME) location, gender, and rurality. Physician birthdate is not included in the public record licensure data sets. Age was estimated using licensee reported graduation year from their undergraduate medical education program (or license date if the graduation year was missing) as of 2014. Given an average age of medical school matriculation in the United States of 24 years,23 physicians were assumed to be age 28 years at the time of graduation. We grouped age into five categories <34 years, 34-43 years, 44-53 years, 54-63 years, and 64-69 years. To account for retirement, this analysis restricts active licensed physician data to physicians with an estimated age younger than 70 years. Physicians retire, on average, between 60 and 69 years of age.24, 25, 26 The first age category of <34 years is an attempt to capture likely ages of residency training, which lasts an average of 4.5 years.27
Physician specialty was categorized using the “area of interest” field in the licensure data set. We coded PCPs as physicians who self-reported primary specialties in family medicine, general internal medicine, general pediatrics, or preventive medicine. Preventive medicine was defined as PCP for physicians who also self-reported family, internal, or pediatric medicine as a secondary area of interest. We coded all other physicians as nonprimary care physicians (NPCPs). Undergraduate medical education (UME) location was categorized as (1) in Arizona, (2) out of Arizona within the United States, and (3) international medical graduate (IMG). We identified gender by matching the physician information available in the licensure data to data in the National Plan and Provider Enumeration System (NPPES), dichotomized as male/female.
We used RUCA codes to assess the number and ratio of physicians by urban-rural geography. RUCA codes use US Census tract data and provide a standardized, national rurality classification system that accounts for population density, proximity to urban areas and commuting patterns.21, 28 The University of Washington’s WWAMI Program provides guidance on grouping the 33 individual RUCA codes into categories or groups, including the WWAMI Rural Health Research Center RUCA “categorization B” of Urban, Large Rural City or Town, Small Rural Town and Isolated Small Rural Town group nomenclature.29 In this analysis, we refer to these groups as (1) urban, (2) large rural, and (3) small rural. Physician practice location zip codes were mapped to RUCA codes using the above-mentioned USDA RUCA zip-code approximation file.22 In descriptive analysis, we also assessed physician density and scored this as the number of physicians per 100,000 Arizona residents. Physician density counts are reported for 2014 and 2019. Population data are from the US Census American Community Survey (ACS) 5-year estimates for 2014 and 2019. Recognizing that population change may be a contributing factor to physician relocation, we also explored population change in the primary analysis. We created a percent population change variable using the US Census population data (<0 [reference], % change between 0-10, and % change >10).
Primary Analysis
This was a retrospective cohort study. We described physician counts for 2014, 2019, and the characteristics for those with an Arizona practice location address at both time points. These counts provide context for the population of physicians in Arizona. The primary analysis was based on physicians who reported practice addresses at both time points. For these, we describe changes in physician density within RUCA groups between 2014 and 2019 and used χ2 and Fisher exact tests to examine differences between physicians practicing in urban, large rural, and small rural locations. Finally, we used a multivariable logistic regression model to examine the adjusted odds and 95% confidence interval (95% CI) for relocating between 2014 and 2019. Based on literature that highlights the association between physician specialty and location,10 we explored potential moderation from PCP/NPCP on relocation. We used a likelihood ratio test to assess this interaction. The multivariable logistic regression model included 2014 RUCA location, UME location, age, and gender. We performed statistical tests using Stata 16 (StataCorp LLC, College Station, TX).
In 2014, there were 15,453 MD and DO physicians with an active Arizona license practice address. By 2019, this number grew to 17,141 Arizona licensed physicians (Table 1). This represents an increase of 11%, a rate that outpaced Arizona’s population growth of 6% over the same period. The increase favored urban centers; the proportion of all Arizona physicians practicing in urban areas increased from 94.0 to 94.7%. In contrast, large and small rural areas experienced a net decrease of physicians. By 2019, urban areas gained 1,709 physicians while large rural and small rural areas lost 9 and 12 physicians, respectively. Where the physician workforce grew by 12% in urban areas, it declined by 1% and 5% in large rural and small rural areas. In 2014, in urban areas there were 241 physicians for every 100,000 residents. This increased to 255 by 2019. In large rural areas, the number of physicians per 100,000 persons declined from 177.6 to 175.8, and from 106.2 to 102.6 in small rural areas.
Between 2014 and 2019, there were 11,202 physicians under the estimated age of 70 years who reported an Arizona practice location at both time points. Within this group, 33% changed practice locations within the state, the vast majority of whom (95%) relocated to a location with the same RUCA group code. However, relocation patterns varied based on physicians’ 2014 RUCA location. Compared to other RUCA groups, a larger proportion of urban physicians relocated within the same RUCA group in Arizona, whereas relocating physicians in large rural and small rural areas tended to relocate to more urban Arizona areas (Table 2).
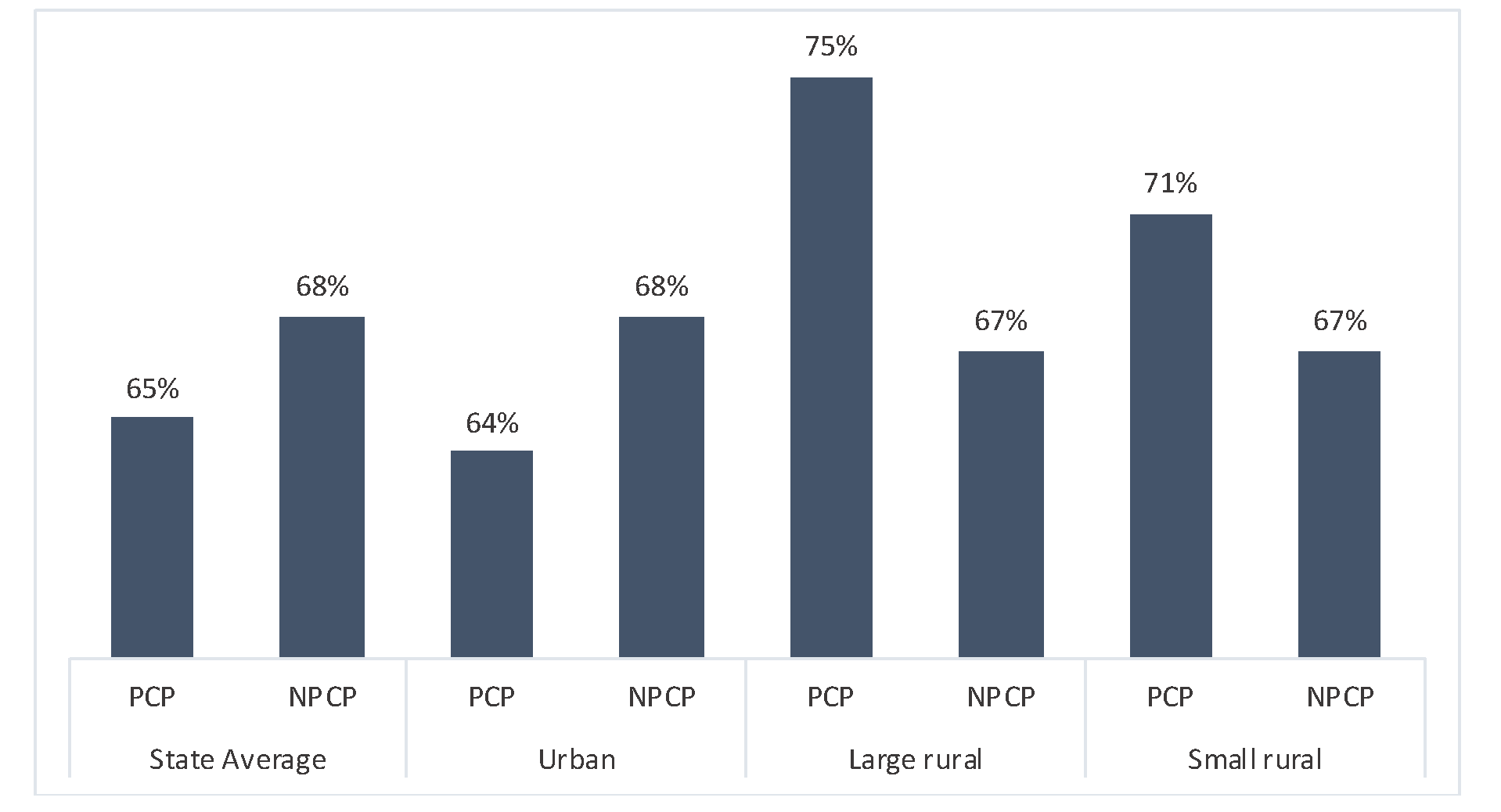
Physician type also differed by RUCA code. In 2014, 32% percent of Arizona urban physicians were PCPs, compared to 40% of large rural and 60% of small rural physicians. A lower percentage of female physicians practiced in large rural areas. These differences were all statistically significant. Further examining relocation patterns by primary care status and RUCA (Figure 1) shows that while most physicians across all RUCA groups and specialty type who remained in Arizona did not relocate between 2014 and 2019, among PCPs, 75% of large rural and 71% of small rural Arizona physicians remained at their same practice location compared to only 64% of urban PCP physicians. The percentage of NPCPs who did not relocate was virtually the same across all RUCA groups (67%-68%).
To examine the odds of relocating in Arizona, we fit logistic regression models stratified by physician type (Table 3). The likelihood ratio test comparing models with and without a physician type/RUCA interaction term was statistically significant (P=.045), indicating a moderating effect. In an unadjusted model, PCPs practicing in large rural areas in 2014 had lower odds of relocating in Arizona (OR 0.61, 95% CI 0.42-0.88) than urban-located PCPs. Adjusting for age, gender, and UME, compared to urban PCPs, PCPs in large rural areas maintained lower odds of relocating in Arizona (aOR 0.62, 95% CI 0.43-0.90). Compared to male NPCPs, female NPCPs were 20% more likely to relocate (aOR 1.20, 95% CI 1.08-1.33). Compared to physicians 64-69 years old, those younger than 34 years had higher odds of relocating in Arizona. This was true for PCPs (aOR 3.23 95% CI 2.33-4.60) and NPCPs (aOR 2.71 95% CI 1.77-4.15). Physicians who were 34-43 years old also had higher odds of relocating in Arizona (PCP [aOR 1.80 95% CI 1.32-2.43], NPCP [aOR 1.49 95% CI 1.24-1.80]). When we examined percent population change in the adjusted model, we did not observe a substantive change to the results. It was not included in the final model.
| |
Licensed Arizona Physicians—2014
(N=15,453), n (%)
|
Licensed Arizona Physicians—2019
(N=17,141), n (%)
|
|
Urban focused
|
14,531 (94.0)
|
16,240 (94.7)
|
|
Large rural city/town
|
657 (4.3)
|
648 (3.8)
|
|
Small and isolated rural city/town
|
265 (1.7)
|
253 (1.5)
|
|
Primary care physician
|
5,193 (33.6)
|
5,908 (34.5)
|
|
Medical education in Arizona
|
1,822 (11.8)
|
2,301 (13.4)
|
|
Female
|
4,696 (30.4)
|
5,964 (34.8)
|
|
|
Arizona N=11,202, n (%)
|
Urban N=10,661 (95.2), n (%)
|
Large R ural N=380 (3.4), n (%)
|
Small Rural N=161 (1.4), n (%)
|
P Value
|
|
Relocation Patterns (2014 - 2019)
|
|
|
|
|
|
|
Did not relocate
|
7,493 (66.9)
|
7,115 (66.7)
|
266 (70.0)
|
112 (69.6)
|
<.001
|
|
Relocated more urban
|
102 (0.9)
|
0 (0.0)
|
61 (16.1)
|
41 (25.5)
|
|
|
Relocated within same RUCA code
|
3,515 (31.4)
|
3,466 (32.5)
|
41 (10.8)
|
8 (5.0)
|
|
|
Relocated more rural
|
92 (0.8)
|
80 (0.8)
|
12 (3.2)
|
0 (0.0)
|
|
|
Physician Type (2014)
|
|
|
|
|
<.001
|
|
Primary care
|
3,605 (32.2)
|
3,355 (31.5)
|
153 (40.3)
|
97 (60.2)
|
|
|
Nonprimary care
|
7,597 (67.8)
|
7,306 (68.5)
|
227 (59.7)
|
64 (39.8)
|
|
|
Undergaduate Medical Education
|
|
|
|
|
.002
|
|
Arizona
|
1,563 (14.0)
|
1,490 (14.0)
|
49 (12.9)
|
24 (14.9)
|
|
|
Out of Arizona
|
6,872 (61.4)
|
6,534 (61.3)
|
219 (57.6)
|
119 (73.9)
|
|
|
Out of United States
|
2,765 (24.7)
|
2,635 (24.7)
|
112 (29.5)
|
18 (11.2)
|
|
|
Gender
|
|
|
|
|
.002
|
|
Female
|
3,445 (30.9)
|
3,305 (31.1)
|
83 (21.9)
|
57 (35.4)
|
|
|
Male
|
7,712 (69.1)
|
7,312 (68.9)
|
296 (78.1)
|
104 (64.6)
|
|
|
Age in Years (2014)
|
|
|
|
|
.02
|
|
<34
|
339 (3.0)
|
315 (3.0)
|
16 (4.2)
|
8 (5.0)
|
|
|
34-43
|
3,309 (29.5)
|
3,170 (29.7)
|
98 (25.8)
|
41 (25.5)
|
|
|
44-53
|
3,681 (32.9)
|
3,521 (33.0)
|
110 (28.9)
|
50 (31.1)
|
|
|
54-63
|
2,933 (26.2)
|
2,762 (25.9)
|
118 (31.1)
|
53 (32.9)
|
|
|
64-69
|
940 (8.4)
|
893 (8.4)
|
38 (10.0)
|
9 (5.6)
|
|
|
Unadjusted Model NPCP, N=7,597
|
Unadjusted M odel PCP, N=3,605
|
|
|
OR (95% CI)
|
P Value
|
OR (95% CI)
|
P Value
|
|
2014 RUCA Location
|
|
|
|
|
|
Urban focused
|
ref
|
|
ref
|
|
|
Large rural city/town
|
1.05 (0.79-1.39)
|
0.74
|
0.61 (0.42-0.88)
|
<.01
|
|
Small and isolated small rural town
|
1.04 (0.61-1.75)
|
0.89
|
0.72 (0.46-1.13)
|
.15
|
|
|
Adjusted Model NPCP N=7,597
|
Adjusted Model PCP N=3,605
|
|
|
aOR (95% CI)
|
P Value
|
aOR (95% CI)
|
P Value
|
|
2014 RUCA Location
|
|
|
|
|
|
Urban focused
|
ref
|
|
ref
|
|
|
Large rural city/town
|
1.04 (0.78-1.38)
|
.78
|
0.62 (0.43-0.90)
|
.01
|
|
Small and isolated small rural town
|
1.13 (0.67-1.92)
|
.65
|
0.73 (.46-1.15)
|
.18
|
|
Medical Education (UME)
|
|
|
|
|
|
Arizona
|
ref
|
|
ref
|
|
|
Out of Arizona
|
1.01 (0.87-1.18)
|
.86
|
0.97 (0.80-1.19)
|
.79
|
|
Out of United States
|
1.24 (1.08-1.33)
|
.02
|
1.20 (0.97-1.48)
|
.09
|
|
Gender
|
|
|
|
|
|
Male
|
ref
|
|
ref
|
|
|
Female
|
1.20 (1.08-1.33)
|
<.01
|
1.01 (0.88-1.18)
|
.80
|
|
2014 Age in Years
|
|
|
|
|
|
<34
|
3.23 (2.33-4.60)
|
<.01
|
2.71 (1.77-4.15)
|
<.01
|
|
34-43
|
1.49 (1.24-1.80)
|
<.01
|
1.80 (1.32-2.43)
|
<.01
|
|
44-53
|
0.92 (.077-1.11)
|
.34
|
1.13 (0.83-1.53)
|
.43
|
|
54-63
|
0.95 (0.78-1.15)
|
.59
|
0.86 (0.63-1.18)
|
.35
|
|
64-69
|
ref
|
|
ref
|
|
This study adds to previous findings that rural areas have fewer physicians compared to urban areas. In Arizona, though physician growth outpaced population growth between 2014 and 2019, the growth occurred predominately in urban areas. In 2019, the state had an overall physician density of 246 physicians per 100,000 residents. In its urban, large rural, and small rural areas, there were 255, 176, and 103 physicians for every 100,000 residents, respectively. Regardless of rurality, all areas in Arizona fell below the US median density of 263 physicians per 100,000 persons.8
We found that most Arizona physicians did not relocate within the state between 2014 and 2019. Those who did were mainly urban physicians moving within the same RUCA group and rural physicians who relocated to more urban areas of Arizona. Of the 33% of physicians in our study who relocated within Arizona, 95% moved within the same RUCA code, 3% relocated more urban, and 2% more rural. This relates to McGrail et al’s 2000-2014 relocation study that found that ≤45-year-old PCP physicians’ mobility rate was almost double (17%) that of 46-65 year-old PCPs (9%).15 These appear to align with our 33% overall rate; McGrail et al measured mobility within 2-year windows compared to our 5-year period. We similarly found higher odds of relocation among younger physicians. However, where our findings showed that PCPs in large rural areas had lower odds of relocating, McGrail et al found worse retention rates in rural counties.
Another national study that examined US PCP migration found that between 2008 and 2013, only 6% of physicians moved to a new practice site, and only 1% moved across county lines.20 These authors used US, office-based provider data that are updated every 6 months (SK&K database). They suggested that their relocation findings were lower than what prior studies found, including ours, because other data sets may include systematic errors related to practice location. This includes studies using American Medical Association Masterfile data where a portion of physicians may report residential rather than practice addresses, leading to an overestimate of supply in high-income areas.20 This may also occur in licensure data like we used. This is likely more common among physicians who maintain an active license but no longer practice. Limiting our analysis to physicians estimated to be younger than the average retirement age may have limited some of this error in our study, but the larger issue relates to improving the quality of physician location and activity data. One promising option involves collecting a standard set of workforce data by state medical boards. The Federation for State Medical Boards recommends collecting a minimal set of data that include birthdates, UME graduation dates, specialty and subspecialty certifications, and employment status including weekly hours worked and hours worked by location.30 These data would provide a more accurate census of the physician workforce,31 including the distribution located in rural and underserved areas. We suggest that including information related to graduate medical training (residency) and J-1 visa status should also be considered as essential datapoints. Monitoring workforce supply and predicting future need requires a clearer understanding of physicians’ training, employment, and activity status.
Limitations and Future Research
In this study, we explored physician relocation patterns and odds of relocating in Arizona within a 5-year period. It is possible that with a longer observation period, and additional data points, other trends could be identified. Likewise, we only used Arizona practice location licensure data; our study does not account for patterns among physicians who retired or relocated outside of Arizona. The AMB licensure data did not contain information on practice setting, practice hours, physician age, GME location, or if the physician is in a residency program. Additionally, we cannot account for the role of J-1 visa waiver physicians in Arizona. The small number of small rural (RUCA 3) physicians in our analysis (n=161) also made it difficult to draw statistical inferences for this group.
In addition to tracking relocation trends longitudinally, future research should use qualitative methodologies. Interviews with physicians across RUCA groups, particularly in large and small rural areas, would clarify the motivations of physicians who change RUCA group locations, particularly those who moved from or into rural areas. This should extend to capturing rural residency experiences. These data may inform program or policy initiatives to address physician retention in more rural areas.
Between 2014 and 2019, we found that two-thirds of Arizona physicians did not relocate to a new practice location. Among those who did, few physicians moved outside of their RUCA groups; only 2% of relocators moved to a more rural RUCA. In Arizona, we identified an intersection between rural location, primary care physician status, and physician’s odds of relocating in Arizona. PCPs who lived in large rural areas were 38% less likely to relocate within Arizona compared to urban PCPs. Regularly monitoring the physician workforce is necessary to address physician supply shortages and monitor changes in its distribution. More detailed data on physician’s demographics and professional activity will assist this effort.
Acknowledgments
The Arizona Area Health Education Center supported this work. It was completed as part of the Workforce Data & Analysis project at the Arizona Center for Rural Health. We thank Susan Coates for her assistance in cleaning and organizing the licensure data and Patrick Wightman for helping with the analysis.
References
3. Salsberg ES. Is the Physician Shortage Real? Implications for the Recommendations of the Institute of Medicine Committee on the Governance and Financing of Graduate Medical Education. Acad Med. 2015;90(9):1210-1214. doi:10.1097/ACM.0000000000000837
4. Petterson SM, Liaw WR, Phillips RL Jr, Rabin DL, Meyers DS, Bazemore AW. Projecting US primary care physician workforce needs: 2010-2025. Ann Fam Med. 2012;10(6):503-509. doi:10.1370/afm.1431
6. Dalen JE, Ryan KJ, Alpert JS. Where have the generalists gone? They became specialists, then subspecialists. Am J Med. 2017;130(7):766-768. doi:10.1016/j.amjmed.2017.01.026
11. Koch B, Coates S, Carter H, Derksen D. Arizona Primary Care Physician Workforce Report. Arizona Center for Rural Health; 2019:1-25.
12. Rosenblatt RA. Commentary: do medical schools have a responsibility to train physicians to meet the needs of the public? The case of persistent rural physician shortages. Acad Med. 2010;85(4):572-574. doi:10.1097/ACM.0b013e3181d306b8
14. Laven G, Wilkinson D. Rural doctors and rural backgrounds: how strong is the evidence? A systematic review. Aust J Rural Health. 2003;11(6):277-284. doi:10.1111/j.1440-1584.2003.00534.x
15. McGrail MR, Wingrove PM, Petterson SM, Bazemore AW. Mobility of US rural primary care physicians during 2000-2014. Ann Fam Med. 2017;15(4):322-328. doi:10.1370/afm.2096
16. Ono, T, Schoenstein, M & Buchan, J . 2014. Geographic Imbalances in Doctor Supply and Policy Responses. OECD iLibrary. doi:10.1787/18152015
17. Cameron PJ, Este DC, Worthington CA. Professional, personal and community: 3 domains of physician retention in rural communities. Can J Rural Med. 2012;17(2):47-55.
18. Farmer J, Kenny A, McKinstry C, Huysmans RD. A scoping review of the association between rural medical education and rural practice location. Hum Resour Health. 2015;13(1):27. doi:10.1186/s12960-015-0017-3
19. Goodfellow A, Ulloa JG, Dowling PT, et al. Predictors of primary care physician practice location in underserved urban or rural areas in the United States: a systematic literature review. Acad Med. 2016;91(9):1313-1321. doi:10.1097/ACM.0000000000001203
20. Kandrack R, Martsolf GR, Reid RO, Friedberg MW. Primary care physician migration patterns and their implications for workforce distribution. J Gen Intern Med. 2019;34(7):1108-1109. doi:10.1007/s11606-019-04872-4
21. Morrill R, Cromartie J, Hart G. Metropolitan, urban, and rural commuting areas: toward a better depiction of the United States Settlement System. Urban Geogr. 1999;20(8):727-748. doi:10.2747/0272-3638.20.8.727
24. Petterson SM, Rayburn WF, Liaw WR. When do primary care physicians retire? Implications for workforce projections. Ann Fam Med. 2016;14(4):344-349. doi:10.1370/afm.1936
26. Silver MP, Hamilton AD, Biswas A, Warrick NI. A systematic review of physician retirement planning. Hum Resour Health. 2016;14(1):67. doi:10.1186/s12960-016-0166-z
28. National Academies of Sciences Engineering and Medicine. Rationalizing Rural Area Classifications for the Economic Research Service: A Workshop Summary. The National Academies Press;2016.
31. Young A, Chaudhry HJ, Thomas JV, Dugan M. A census of actively licensed physicians in the United States. J Med Regul. 2012;99(2):11-12. doi:10.30770/2572-1852-99.2.11



There are no comments for this article.