Purpose: The purpose of this study is to establish the psychometric properties and diagnostic accuracy of the Teen Hurt-Insult-Threaten-Scream-Sex (TeenHITSS), a 5-item measure used to screen adolescents for family violence in clinical settings.
Methods: Study participants included 251 adolescent participants (n=197 not at-risk subsample; n=56 at-risk subsample), recruited from ambulatory care clinics, a medical center at-risk referral clinic, and area shelters. Participants completed a cross-sectional survey, including the TeenHITSS and Parent-Child Conflict Tactics Scales (CTSPC) questionnaires. We calculated internal reliability, validity, and sensitivity and specificity for the full sample and both subsamples for each screening instrument.
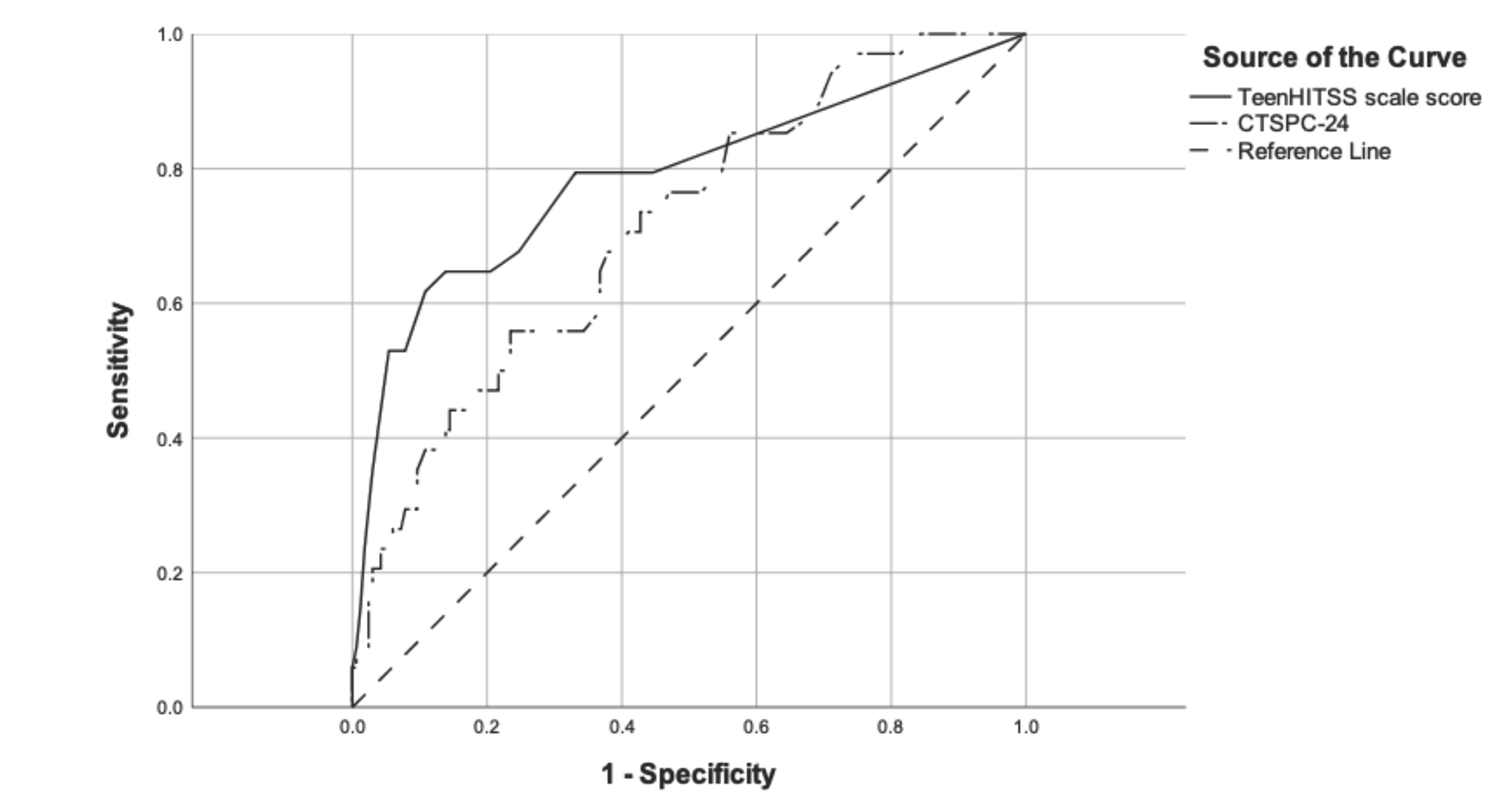
Results: Concurrent validity between the TeenHITSS and CTSPC was strong (r=.71, P<.000). We determined an optimal cutpoint based on sensitivity and specificity for correctly identifying abuse victims as a score of one or greater on the TeenHITSS. The TeenHITSS also proved slightly superior to the CTSPC in differentiating between victims and nonvictims of adolescent abuse (AUC=.79 vs .73, respectively).
Conclusions: The TeenHITSS screening tool performed as well as the CTSPC in correctly classifying at-risk and not-at-risk teenagers and offers much greater utility to providers by supplying an actionable cut score. The findings of this study suggest that TeenHITSS is a valid and reliable tool to screen for physical and sexual abuse in children ages 13 years and older in clinical settings and can help health care providers detect adolescent abuse and initiate intervention and prevention of future abuse.
In 2018, the United States reported a national rounded number of child maltreatment victims totaling 678,000, of whom 123,066 were adolescents 13-17 years of age.1 Over 50% of adolescents will experience some form of violence during their lifetime, while approximately one-quarter will experience physical or sexual maltreatment by a caretaker2, 3 ; around 15% of adolescents experience multiple forms of maltreatment.1 Childhood maltreatment is associated with increased risk of diabetes, cardiac events, brain damage, hypertension, arthritis, and impaired brain development and functioning.4-7 Physical abuse during adolescent years increases the likelihood of developing posttraumatic stress disorder, depression, anxiety, conduct disorders, and certain health-compromising behaviors, such as cigarette smoking.8 Abuse during adolescence is associated with increased incidence of criminality and victims of abuse are twice as likely as nonvictims to commit intimate partner violence.9
While definitions of abuse and neglect vary, all states require the reporting of suspected or confirmed maltreatment to a child protective services (CPS) agency.6 Despite the prevalence and severity of health outcomes, screening for abuse in primary care settings is not routine.10, 11 While there are myriad barriers to screening for child abuse,12 the most-reported barrier is a lack of education and adequate training.13, 14 Continuing education and training efforts have proven successful in increasing screening and reporting,15, 16 but no standard measure for clinical screening for adolescent abuse currently exists. The most-used measure, the Parent-Child Conflict Tactics Scales (CTSPC), has been widely used in epidemiological and clinical studies,17 but its length and complexity introduce significant barriers to routine usage. Given the long-term ramifications of adolescent abuse, it is vital that effective screening measures are developed, validated, and deployed in clinical settings. The use of such screening assessments can assist clinicians in identifying abuse victims and in the development of targeted interventions.
Present Study
The purpose of this study was to determine the psychometric efficacy and diagnostic accuracy of the Teen Hurt-Insult-Threaten-Scream-Sex (TeenHITSS) as a brief screening method for adolescent abuse. TeenHITSS is a 5-item, self-reported tool used to provide medical professionals with awareness of physical and sexual abuse. TeenHITSS is a variation of the HITS screening tool, a consistent, valid, and reliable measure used to assess family and intimate partner violence and abuse. The HITS has been previously validated in pediatric and adult populations.18, 19, 20, 21 This study explores the psychometric properties of the TeenHITSS among adolescents who are at-risk versus adolescents who are not at-risk.
Setting and Participants
Data were collected over 5 years (2014-2019) and include two subsamples of English- or Spanish-speaking adolescent patients residing in a large southern US city (n=253). The primary care subsample included patients (n=197) recruited while being seen in five ambulatory care settings for routine care. An at-risk subsample included confirmed adolescent victims of abuse (n=56) either receiving treatment at a medical center’s at-risk referral clinic or residing in four area shelters for victims of domestic abuse and violence. Though adolescents in the primary care subsample were not necessarily at zero risk, we differentiate between this group of general patients and the at-risk group with confirmed abuse histories (described below). Indeed, two participants from the primary care subsample reported sexual abuse via the TeenHITSS; we removed these participants from analyses in order to utilize a true negative comparison sample for psychometric analyses, resulting in a final sample size of 251 adolescent participants (n=195 primary care adolescents). Though we removed these participants, we replicated our sensitivity and specificity analyses (described below), post hoc, with the full primary care sample (n=197) and report those results below.
Data Collection
This study and all research procedures were reviewed and approved by our Institutional Review Board (IRB). The IRB mandated that only verbal consent be collected; written consent was not documented due to the possibility that an abusive family member or caretaker with access to the patient’s medical record could discover the abuse disclosure.
Specific to the primary care subsample, physicians and staff confirmed participant eligibility and participants were then recruited during a primary care visit. Participants were informed that participation was confidential and would not affect their care. No identifying information was collected. Specific to the at-risk subsample, shelter staff confirmed and verified at-risk status by (1) reviewing parental admission of abuse, participant medical history, or CPS reports for victims recruited at shelter sites and the referral clinic, and (2) confirming abuse using shelter intake procedures for adolescents residing at a shelter who did not have a CPS report on file. In order to protect the safety and privacy of potential participants residing at family violence shelter recruitment sites, all participant recruitment was conducted on site by shelter staff. Each adolescent participant was provided two measures: TeenHITSS and Conflict Tactics Scale: Parent-Child Version (CTSPC), for paper-and-pencil self-administration. The sequencing of the questionnaires was counterbalanced to avoid presentation effects. Participants completed the assessments privately during a medical visit or, specific to the at-risk subsample, after a counseling appointment. Participation was voluntary; no incentive was provided.
Instruments
TeenHITSS
TeenHITSS is a self-reported modified version of the Pediatric HITSS completed by adolescent participants.21 TeenHITSS contains five items, including, “During the last year, how often would you estimate that an adult in your home did each of the following: (1) Physically hurt you; (2) Insult you or talk down to you; (3) Threaten you with physical harm; (4) Scream or curse at you; (5) Forced you to have sex.” Participants responded to each item using a 5-point Likert scale (0=Never; 1=Rarely; 2=Sometimes; 3=Fairly Often; 4=Frequently). Scale scores were calculated by summing responses, with scores ranging from 0-20; higher scores indicate more frequent abusive behavior.
CTSPC
We used the CTSPC to evaluate concurrent and discriminant validity. CTSPC was designed to measure childhood maltreatment using parent/guardian self-report. In our study, the adolescent participants completed the “child version” which is designed to obtain reports of parental behaviors.22 CTSPC contains 22 items and has been validated to measure child maltreatment in children from infancy to 17 years of age using the following subscales: Nonviolent discipline (four items), psychological aggression (five items), and physical assault (13 items). We included two sexual abuse items that are adjunctive to the CTSPC. Items are prompted with, “During the last year, how often would you estimate that an immediate family member has done each of the following?” The frequency of each example of maltreatment was rated using a 7-point Likert scale ranging from 0 (never) to 6 (>20 times). Responses were recoded such that responses range from 0-25.22 The two sexual abuse items utilize a unique 3-point Likert scale ranging from 0 (never) to 2 (>1). Following recoding, we summed responses within subscales.22 We also calculated a total scale score for the full CTSPC (0-550), and the full CTSPC with the addition of the two sexual abuse items (0-554).
Analyses
Reliability
We calculated internal reliability (Cronbach’s α) of both scales for the full sample and both subsamples. The study was adequately powered to estimate, for a 5-item measure, Cronbach’s α ranging from .50 to .95, with an α error of .05, power of .80, and smallest subsample size of 56 participants (in the at-risk subsample), assuming a null hypothesis Cronbach’s α=0.00. Assuming a null hypothesis Cronbach’s α=0.50, the study is adequately powered to estimate a Cronbach’s α ranging from .75 to .95 (for the at-risk subsample) and ranging from .65 to .95 (for the full study sample).32,33 In addition, we report the average interitem correlation (AIC) as an additional measure of internal reliability for TeenHITSS responses, for each subsample. AIC should ideally total between .15 and .50 to indicate a measure captures a specific construct while minimizing redundant items.34
Validity
We assessed convergent and discriminant validity using Pearson’s correlation to calculate alignment of TeenHITSS total scores and CTSPC total score, as well as agreement between TeenHITSS individual items and CTSPC subscales. Convergent validity is determined by strong, positive, significant correlations) between concordant subscales across measures, while discriminant validity is determined by weak, nonsignificant correlations between discordant subscales across measures.23 Similar to analyses supporting the PedHITSS,21 we hypothesize strong, positive, significant correlations between the total scale scores, as well as between the following TeenHITSS items and CTSPC subscales: (1) Hurt-Physical Assault; (2) Insult-Psychological Aggression; (3) Threaten-Physical Assault; (4) Scream-Psychological Aggression; and (5) Sex-Sexual Abuse. We also hypothesize weak, nonsignificant correlations between the following TeenHITSS items and CTSPC subscales: (1) Insult-Sexual Abuse; (2) each TeenHITSS item and Nonviolent Discipline. Though there is disagreement in the literature regarding specific correlation coefficient thresholds,24, 25, 26 we set benchmarks for convergent and divergent validity a priori, based on conservative estimates of each which are substantiated in the literature23 : namely, r>.60 (P<.05) between concordant subscales to indicate convergent validity, and r<.40 (P>.05) between discordant subscales to indicate divergent validity.
In addition, the construct validity of TeenHITSS is tested using factor analysis. The Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy, Bartlett’s test of sphericity (a test of the correlation matrix, with results indicated by χ2), and shared variance across scale items (h2) are each reported. First, the KMO statistic should be closer to 1, while the Bartlett’s sphericity statistic should be significant, to indicate a factor analysis of the TeenHITSS items is possible. Though the PedHITSS factor structure provides guidance with regard to possible factor structure of the TeenHITSS (ie, the PedHITSS has been substantiated as having a two-factor structure, with insult, threaten, and scream items forming one factor, and hurt and sexual abuse forming a second factor21), the current study represents the first test of the TeenHITSS. Thus, we proceed first using exploratory factor analysis (EFA), using maximum likelihood estimation, to examine the number of potential factors as determined by eigenvalue (percent of the variance captured). Second, we employed confirmatory factor analysis (CFA) with varimax rotation to specify the number of factors present in the measure. As is standard, model fit for the EFA and CFA is reported using χ2.
Sensitivity and Specificity
We analyze the ability of the TeenHITSS (as well as the CTSPC) to detect whether a participant was located in the primary care or at-risk subsample via receiver operating characteristic (ROC) curves. Using the sensitivity and specificity statistics, we describe optimal cutpoints for each measure (each including, and excluding, their respective items assessing sexual abuse). We also present each measure’s area under the ROC curve (AUC), a measure of diagnostic accuracy; comparisons between the two measures’ diagnostic accuracies are discussed. The TeenHITSS was designed to identify adolescent primary care patients who are experiencing or are at-risk of abuse; as such, we prioritize sensitivity of the measure (ie, the ability to detect children experiencing abuse) over specificity.
Sample Demographics
Participants in the sample included 251 adolescents (n=195 primary care; n=56 at-risk) with a mean age of 15.22 years (1.58 SD); the majority (60.6%) identified as female. The majority of participants self-identified as Hispanic (37.8%), while almost one-third of participants (31.5%) identified as White; 2% of participants completed the survey in Spanish. The two subsamples did not significantly differ by age (F=.11, P=.74), though female adolescents were overrepresented in the at-risk subsample (n=42; χ2=6.30, P=.02). The two subsamples differed in regard to participant race/ethnicity as well; participants who self-identified as Black/African American were particularly overrepresented in the at-risk subsample (n=13; χ2=9.98, P=.04). Complete demographic data can be found in Table 1.
Specific to TeenHITSS scores, the full sample scored an average of 2.68 on the full TeenHITSS (SD=3.89; range 0 to 19; 47% scored 0; kurtosis=2.81, skewness=1.74), while the abused subsample scored an average of 6.56 (SD=5.21; range 0 to 19; 17.9% scored 0), and the primary care subsample scored an average 1.63 (SD=2.60; range 0 to 15; 55% scored 0). These samples significantly differed in regard to TeenHITSS scores, as expected (F=89.79, P<.001). Among the primary care subsample, participants endorsed hurt (n=19), insult (n=50), threaten (n=20), and scream (n=76) items, specifically.
|
Characteristics
|
n (%) or Mean (SD) (N=251)
|
n (%) or Mean (SD) At-Risk (N=56)
|
n (%) or Mean (SD) Primary Care (N=195)
|
Tests of Between-Group Differences
|
|
Adolescent/Teen Participant
|
|
|
|
|
|
Age*
|
15.22 (1.58)
|
15.29 (1.55)
|
15.21 (1.59)
|
F=.11, P=.74
|
|
Language of survey administered
|
|
|
|
|
|
English
|
246 (98.0)
|
53 (94.6)
|
193 (99.0)
|
|
|
Spanish
|
5 (2.0)
|
3 (5.4)
|
2 (1.0)
|
|
|
Sex
|
|
|
|
χ2=6.30, P=.02
|
|
Female
|
152 (60.6)
|
42 (75.0)
|
110 (56.4)
|
|
|
Male
|
99 (39.4)
|
14 (25.0)
|
85 (43.6)
|
|
|
Race/Ethnicity (N=268)**
|
|
|
|
χ2=9.98, P=.04
|
|
Hispanic
|
95 (37.8)
|
27 (48.2)
|
68 (34.9)
|
|
|
White
|
79 (31.5)
|
12 (21.4)
|
67 (34.4)
|
|
|
Black
|
44 (17.5)
|
13 (23.2)
|
31 (15.9)
|
|
|
Asian
|
15 (6.0)
|
0 (0.0)
|
15 (7.7)
|
|
|
Other/mixed
|
17 (6.8)
|
4 (7.1)
|
13 (6.7)
|
|
Reliability
The TeenHITSS demonstrated good internal reliability with the full study sample (α=.80, n=251), with the sample of at-risk adolescents (α=.75; AIC=.40; n=56), and with the primary care subsample (α=.74; AIC=.49; n=195). The latter analysis contains solely four items, as zero participants in the primary care adolescent subsample answered positively to the fifth TeenHITSS item assessing sexual abuse. Similarly assessing the reliability of the TeenHITSS using solely the first four items with the at-risk subsample resulted in an improved Cronbach’s α of .88 (AIC=.49); the improvement is likely due to few positive responses on the sexual abuse item of the measure.
The CTSPC was similarly found to have good internal reliability, both in the 22-item form (α=.88, n=251) and 24-item form (ie, including the two sexual abuse items; α=.88). The 24-item CTSPC performed similarly within the at-risk (α=.92, n=56) and primary care subsamples (α=.80, n=195), as did the 22-item CTSPC (α=.92, at-risk; α=80, primary care). However, the CTSPC subscales demonstrated mixed internal reliability. Whereas the Psychological Aggression (α=.82) and Physical Assault (α=.93) subscales demonstrated good reliability, the Nonviolent Discipline subscale did not perform as strongly (α=.57). A post hoc test of the reliability of this subscale with solely the primary care subsample minimally improved consistency (α=.60).
Overall, both the TeenHITSS and CTSPC (full-scale scores) demonstrated good internal reliability when administered to either participant subsample, and when including or excluding their respective items assessing sexual abuse.
Convergent and Discriminant Validity
The TeenHITSS and CTSPC (24-item) scale totals were strongly correlated (r=.71, P<.000). Convergent validity was also demonstrated via strong, positive, and significant correlations between most concordant TeenHITSS item-CTSPC subscales, as hypothesized (Table 2). Specifically, the TeenHITSS hurt item was strongly, positively correlated with the CTSPC Physical Assault subscale; the TeenHITSS insult item was similarly correlated with the CTSPC Psychological Aggression subscale; the TeenHITSS threaten item was strongly, positively correlated with the CTSPC Physical Assault scale; and the TeenHITSS sex item was strongly, positively correlated with the CTSPC Sexual Abuse subscale. Each of these concordant TeenHITSS item-CTSPC subscale correlation coefficients was significantly different from zero, and each was as hypothesized. Only the TeenHITSS scream item failed to demonstrate convergent validity as predicted: responses to this item were positively and significantly correlated with the CTSPC Psychological Aggression subscale, but failed to reach the minimum correlation coefficient set a priori to indicate convergent validity (r=.562, P<.001).
Discordant TeenHITSS-CTSPC domains (eg, TeenHITSS insult item and CTSPC Sexual Abuse subscale; TeenHITSS hurt item and CTSPC Nonviolent Discipline subscale, etc) were weakly correlated, as hypothesized, providing support for the discriminant validity of the TeenHITSS items, and their ability to distinguish from areas of child abuse they were developed to assess, and other areas of abuse and neglect the items were not developed to assess.
|
Item/Subscale
|
1
|
2
|
3
|
4
|
5
|
6
|
7
|
8
|
9
|
|
1. Hurt item
|
--
|
|
|
|
|
|
|
|
|
|
2. Insult item
|
.601***
|
--
|
|
|
|
|
|
|
|
|
3. Threaten item
|
.707***
|
.592***
|
--
|
|
|
|
|
|
|
|
4. Scream item
|
.540***
|
.684***
|
.568***
|
--
|
|
|
|
|
|
|
5. Sex item
|
.277**
|
.116
|
.229***
|
.182**
|
--
|
|
|
|
|
|
6. CTSPC Nonviolent Discipline
|
.307***
|
.283***
|
.292***
|
.270***
|
-.002
|
--
|
|
|
|
|
7. CTSPC Psychological Aggression
|
.633***
|
.663***
|
.562***
|
.562***
|
.177**
|
.489***
|
--
|
|
|
|
8. CTSPC Physical Assault
|
.738***
|
.506***
|
.647***
|
.647***
|
.208**
|
.315***
|
.569***
|
--
|
|
|
9. CTSPC Sex
|
.356***
|
.209**
|
.310***
|
.310***
|
.908***
|
.024
|
.270***
|
.303***
|
--
|
We next utilized exploratory factor analysis (EFA) to test the structure of the TeenHITSS. The results of the KMO measure of sampling adequacy (.79) and Bartlett’s test of sphericity (χ2=491.71, P<.000) suggested a factor analysis was possible. The EFA determined the number of factors, specified by eigenvalue, to be 1. Specifically, the one-factor model accounted for 58.72% of the variance (h2) in the five items, with an eigenvalue of 2.94 (model fit: χ2 [1]=36.19, P<.000). The two-factor model h2 equaled 77.52%, and the second factor had an eigenvalue of .94. The retained factors and each item’s factor loadings are reported in Table 3. Though four of the five TeenHITSS items loaded similarly to the initial factor, the fifth item assessing sexual abuse did not. Thus, we proceeded with a CFA to intentionally test a two-factor structure of the measure.
The results of the CFA testing a two-factor structure of the TeenHITSS demonstrated poor model fit (χ2=2.23, P=.136) with two clusters of items: (1) insult and scream, and (2) hurt, threaten, and to a lesser extent, sex. However, results were mixed: responses to the hurt and threaten items did not distinctly load onto one factor versus the other, and the sex abuse item continued to load poorly on either factor (Table 3). The nonsignificant model, and factor loadings, provide evidence the one-factor solution is preferable. This outcome is similar to prior results examining the factor structure of PedHITSS, with younger samples, and provides support for the construct validity of TeenHITSS, a measure we purport to assess child abuse.
|
|
EFA
|
CFA
|
|
Item
|
1
|
1
|
2
|
|
Hurt
|
.812
|
.494
|
.682
|
|
Insult
|
.784
|
.981
|
.192
|
|
Threaten
|
.804
|
.469
|
.690
|
|
Scream
|
.735
|
.619
|
.371
|
|
Sex
|
.271
|
.054
|
.350
|
|
Eigenvalue
|
2.936
|
--
|
3.876
|
|
Percent of variance
|
58.72%
|
--
|
77.52%
|
Specificity and Sensitivity
Results of our ROC curve analyses provide support for the TeenHITSS performing superiorly to the CTSPC in accurately determining participant group membership (ie, primary care subsample versus at-risk subsample). Specifically, the TeenHITSS AUC equaled .79 (SE=.04, P<.000, 95% CI=0.71-0.87); the AUC for the CTSPC 24-item and 22-item versions were .73 (SE=.04, P<.000, 95% CI=0.64-0.82) and .72 (SE=.05, P<.000, 95% CI=0.63-0.80), respectively. Figure 1 shows the HITSS and CTSPC 24-item ROC curves, for comparison. These results were replicated for our post hoc ROC curve analyses completed with the full primary care subsample (n=197): the TeenHITSS AUC equaled .79 (SE=.04, P<.000), CTSPC 24-item AUC equaled .73 (SE=.04, P<.000), and CTSPC 22-item AUC equaled .72 (SE=.05, P<.000). In other words, replicating sensitivity and specificity analyses with the two primary care participants who were otherwise removed from the sample to test TeenHITSS psychometrics did not change our results.
Sensitivity and specificity estimates indicate that any positive answer on the TeenHITSS (a score of 1) maximizes sensitivity while also demonstrating good specificity (Table 4). Thus, we recommend a TeenHITSS cutpoint of 1, indicating a positive answer on any item should prompt clinician follow-up. In addition, 99.5% of the sample is correctly classified (ie, false positives are eliminated, and specificity is maximized) at a TeenHITSS score of 12.0 (out of 20). Comparatively, the CTSPC (24-item) ROC results do not demonstrate a meaningful difference in sensitivity between any positive item and a score of 7, though the specificity of scores in this range remains so low so as to trigger many false positives. A specificity similar to the HITSS is not found with the CTSPC until a score of 20.5 (out of 554). Thus, the CTSPC is burdened not solely by its cumbersome administration (ie, with a total of 24 items) and scoring methods (with response recoding and multiple subscales capturing individual domains), but the scoring methodology and structure of the measure do not appear to have adequately distinguished between our subsamples.
Though considered a gold standard measure of child maltreatment, the TeenHITSS is at a minimum performing similarly as demonstrated in the present results, if not outperforming the CTSPC, with the current sample.
|
Positive if Greater Than or Equal To
|
Sensitivity
|
1-Specificity
|
|
.50
|
.808
|
.438
|
|
1.50
|
.788
|
.328
|
|
2.50
|
.692
|
.250
|
|
3.50
|
.654
|
.203
|
|
4.50
|
.615
|
.125
|
|
5.50
|
.577
|
.099
|
|
6.50
|
.500
|
.068
|
|
7.50
|
.462
|
.047
|
|
8.50
|
.327
|
.026
|
|
9.50
|
.250
|
.016
|
|
10.50
|
.192
|
.010
|
|
12.00
|
.154
|
.005
|
|
13.50
|
.135
|
.005
|
|
14.50
|
.115
|
.005
|
|
15.50
|
.077
|
.000
|
|
17.50
|
.019
|
.000
|
|
20.00
|
.000
|
.000
|
This study utilized data from 251 adolescents to establish the accuracy and psychometric properties of the TeenHITSS, a 5-item tool for detecting physical, psychological, and sexual abuse of adolescents in clinical settings. As with other versions,18, 19, 20, 21 the TeenHITSS was found to be a reliable, valid, and accurate tool for identifying abuse.
Study results demonstrate TeenHITSS is more accurate at distinguishing at-risk from the primary care adolescents than the CTSPC, while both measures exhibit good internal reliability. Though the CTSPC includes subscales to assess specific abuse types, previous research finds that the 5-item HITSS maps onto these subscales without the additional questions.21 Other measures for screening for adolescent abuse have similar weaknesses. For example, the Childhood Trauma Questionnaire is a 70-item, self-report questionnaire for evaluating experiences of physical, emotional, and sexual abuse.27 The length of the questionnaire, however, poses an impracticality for use in clinical settings. Similarly, the Childhood Exposure to Domestic Violence Scale, the Behavioral Health Screen-Primary Care, and the Trauma History Checklist and Interview, are either too lengthy or not targeted enough for abuse screening.28, 29 Unlike these measures, the TeenHITSS is brief, targeted, and has a simple scoring scheme with valid cutpoints.
The United States Preventive Services Task Force currently finds inadequate evidence to establish the benefits and harms of preventive intervention for child maltreatment, though they do recognize that primary care clinicians are uniquely suited to identify child maltreatment.30 Primary care prevention efforts to address child abuse have shown success, especially where they intervene to increase parental nurturing, improve the parent-child relationship, and educate parents in the use of positive discipline strategies.31 Given that the TeenHITSS can quickly establish both frequency and type of adolescent maltreatment, it is uniquely situated to provide information to primary care clinicians to take such preventive measures, work with families, and execute targeted referrals to behavioral and family therapists. TeenHITSS can also confirm suspected abuse via patient self-report, an important mechanism for detecting abuse and providing specific information to CPS, should a referral be necessary.32
Limitations
Our study demonstrated the psychometric properties of TeenHITSS, including its ability to identify and differentiate teens at-risk of having experienced physical or sexual abuse. However, our study is not without limitations. First, TeenHITSS is a self-reported measure, which can potentially introduce reporting bias, an especially important consideration when assessing a sensitive topic. Though participants were assured of confidentiality, it is possible that respondents experienced sufficient anxiety regarding disclosure of abuse experiences that prevented them from reporting honestly. Second, sample size for preidentified victims of abuse was smaller than expected. Though our goal was to recruit 150 adolescents per subsample, our multisite, several-year recruitment strategy resulting in a lower-than-expected sample size may mirror low abuse report rates among youth found elsewhere in the literature.1, 31 Finally, TeenHITSS is intended to capture abuse experiences occurring in close relationships. It was not designed to identify bullying or dating violence, which limits its application. This may be especially significant given the growing rates of both bullying and intimate partner violence among adolescents over the past several years, which are strongly associated with multiple physical and mental health risks.33, 34 Future adaptations of HITSS will focus on identifying these specific types of abuse.
The TeenHITSS screening tool performed as well as the CTSPC in correctly classifying at-risk teenagers and offers much greater utility to clinicians by supplying an actionable cut score. The findings of this study suggest that TeenHITSS is a valid and reliable tool to screen for physical and sexual abuse in adolescent children in clinical settings and can help clinicians detect abuse and initiate intervention and prevention of future abuse.
Acknowledgments
The authors would like to acknowledge Katie Bridges, MS, Alexandra DeCrescenzo, MPH, and Jessica Chu, MPH, for their work coordinating this project over the years. We would also like to thank the Department of Family and Community Medicine for their ongoing support and dedication to this project.
Funding Statement
This study was supported by Texas Academy of Family Physicians Foundation Research Grant #2013009.
Disclosure
None of the authors have any conflicts of interest to disclose. However, the senior author, Amer Shakil, MD, MBA, was elected President of the Texas Academy of Family Physicians in 2020. His election to President occurred after the above grant was awarded in 2014, but in the interest of transparency the authors disclose this apparent conflict.
Presentations
Findings from this study have been previously presented as lecture presentations at the Society of Teachers of Family Medicine Annual Conference (virtual, April, 2020) and the North American Primary Care Group Annual Conference (Toronto, Ontario, Canada, November, 2019).
References
1. Adams J, Mrug S, Knight DC. Characteristics of child physical and sexual abuse as predictors of psychopathology. Child Abuse Negl. 2018;86:167-177. doi:10.1016/j.chiabu.2018.09.019
3. Finkelhor D, Turner HA, Shattuck A, Hamby SL. Violence, crime, and abuse exposure in a national sample of children and youth: an update. JAMA Pediatr. 2013;167(7):614-621. doi:10.1001/jamapediatrics.2013.42
4. Goodrum NM, Smith DW, Hanson RF, Moreland AD, Saunders BE, Kilpatrick DG. Longitudinal relations among adolescent risk behavior, family cohesion, violence exposure, and mental health in a national sample. J Abnorm Child Psychol. 2020;48(11):1455-1469. doi:10.1007/s10802-020-00691-y
5. Fagan AA. The short- and long-term effects of adolescent violent victimization experienced within the family and community. Violence Vict. 2003;18(4):445-459. doi:10.1891/vivi.2003.18.4.445
7. Bick J, Nelson CA. Early Adverse experiences and the developing brain. Neuropsychopharmacology. 2016;41(1):177-196. doi:10.1038/npp.2015.252
8. Keyes KM, Eaton NR, Krueger RF, et al. Childhood maltreatment and the structure of common psychiatric disorders. Br J Psychiatry. 2012;200(2):107-115. doi:10.1192/bjp.bp.111.093062
9. Fagan AA. The relationship between adolescent physical abuse and criminal offending: support for an enduring and generalized cycle of violence. J Fam Violence. 2005;20(5):279-290. doi:10.1007/s10896-005-6604-7
10. Lapidus G, Cooke MB, Gelven E, Sherman K, Duncan M, Banco L. A statewide survey of domestic violence screening behaviors among pediatricians and family physicians. Arch Pediatr Adolesc Med. 2002;156(4):332-336. doi:10.1001/archpedi.156.4.332
11. Moyer VA; U.S. Preventive Services Task Force. Primary care interventions to prevent child maltreatment: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2013;159(4):289-295. doi:10.7326/0003-4819-159-4-201308200-00667
12. Azizi M, Shahhosseini Z. Challenges of reporting child abuse by healthcare professionals: a narrative review. J Nursing and Midwifery Sciences. 2017;4(3):110-116. doi:10.4103/JNMS.JNMS_3_17
14. Herendeen PA, Blevins R, Anson E, Smith J. Barriers to and consequences of mandated reporting of child abuse by nurse practitioners. J Pediatr Health Care. 2014;28(1):e1-e7. doi:10.1016/j.pedhc.2013.06.004
16. Dudas L, Petrohoy G, Esernio-Jenssen D, et al. Every child, every time: hospital-wide child abuse screening increases awareness and state reporting. Pediatr Surg Int. 2019;35(7):773-778. doi:10.1007/s00383-019-04485-2
17. Sierau S, White LO, Klein AM, Manly JT, von Klitzing K, Herzberg PY. Assessing psychological and physical abuse from children’s perspective: factor structure and psychometric properties of the picture-based, modularized child-report version of the Parent-Child Conflict Tactics Scale - Revised (CTSPC-R). PLoS One. 2018;13(10):e0205401. doi:10.1371/journal.pone.0205401
18. Sherin KM, Sinacore JM, Li XQ, Zitter RE, Shakil A. HITS: a short domestic violence screening tool for use in a family practice setting. Fam Med. 1998;30(7):508-512.
19. Shakil A, Donald S, Sinacore JM, Krepcho M. Validation of the HITS domestic violence screening tool with males. Fam Med. 2005;37(3):193-198.
20. Shakil A, Bardwell J, Sherin K, Sinacore JM, Zitter R, Kindratt TB. Development of Verbal HITS for intimate partner violence screening in family medicine. Fam Med. 2014;46(3):180-185.
21. Shakil A, Day PG, Chu J, Woods SB, Bridges K. PedHITSS: a screening tool to detect childhood abuse in clinical settings. Fam Med. 2018;50(10):763-769. doi:10.22454/FamMed.2018.778329
22. Straus MA, Hamby SL, Warren WL. Conflict Tactic Scales Handbook and Revised Forms. Western Psychological Services; 2003.
23. Evans JD. Straightforward Statistics for the Behavioral Sciences. Brooks/Cole Publishing; 1996.
24. Chan YH. Biostatistics 104: correlational analysis. Singapore Med J. 2003;44(12):614-619.
27. Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. J Am Acad Child Adolesc Psychiatry. 1997;36(3):340-348. doi:10.1097/00004583-199703000-00012
28. Habib M, Labruna V. The Sdolescent Trauma History Checklist and Interview. North Shore University Hospital; 2006.
29. Edleson JL, Shin N, Johnson Armendariz KK. Measuring children’s exposure to domestic violence: The development and testing of the Child Exposure to Domestic Violence (CEDV) Scale. Child Youth Serv Rev. 2008;30(5):502-521. doi:10.1016/j.childyouth.2007.11.006
30. Curry SJ, Krist AH, Owens DK, et al; US Preventive Services Task Force. Interventions to Prevent Child Maltreatment: US Preventive Services Task Force Recommendation Statement. JAMA. 2018;320(20):2122-2128. doi:10.1001/jama.2018.17772
31. Viswanathan M, Fraser JG, Pan H. AHRQ. 2018. Primary Care Interventions to Prevent Child Maltreatment: An Evidence Review for the US Preventive Services Task Force: Evidence Synthesis No. 170. Rockville, MD: Agency for Healthcare Research and Quality
32. Kolko DJ, Kazdin AE, Day BT. Children’s perspectives in the assessment of family violence: psychometric characteristics and comparison to parent reports. Child Maltreat. 1996;1(2):156-167. doi:10.1177/1077559596001002007
33. Niolon PH, Vivolo-Kantor AM, Tracy AJ, et al. An RCT of dating matters: effects on teen dating violence and relationship behaviors. Am J Prev Med. 2019;57(1):13-23. doi:10.1016/j.amepre.2019.02.022



There are no comments for this article.