Background and Objectives: Office-based minor surgery (OBMS) refers to all surgical procedures performed under local anesthetic in the office setting. It is cost effective for the health economy, safe, and appreciated by patients. It is not yet fully understood why some general practitioners (GPs) perform OBMS and others do not, while there is a growing demand for OBMS. Therefore, we explored factors that influence the performance of OBMS by GPs. The aim of this study is to explore the facilitators and barriers that influence GPs in deciding whether to perform OBMS.
Methods: We performed a qualitative study using focus groups consisting of GPs and GP trainers. Two researchers analyzed the data independently.
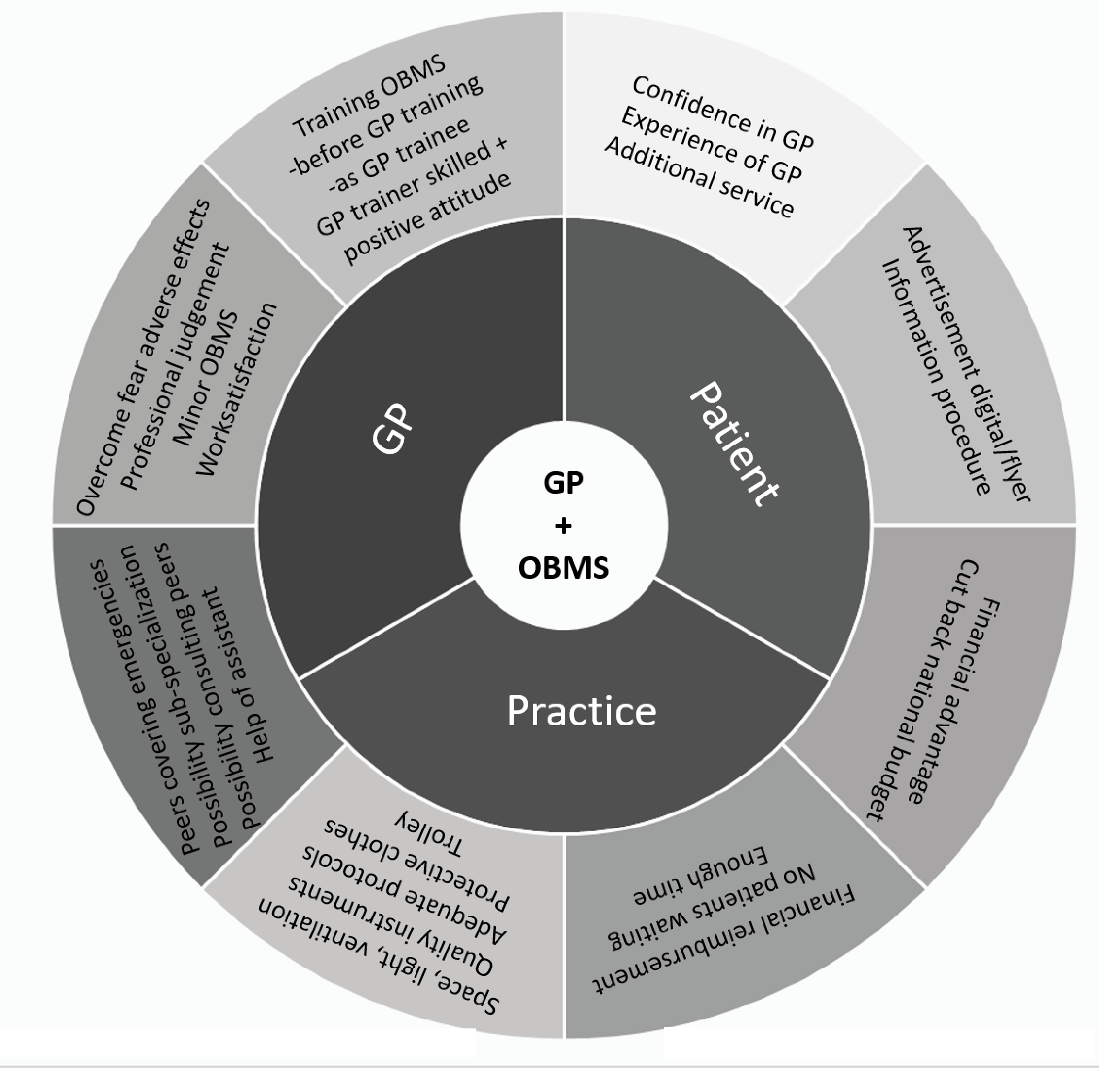
Results: The analysis resulted in a comprehensive list of facilitators and barriers. Besides already known factors such as financial consequences and geographic location, the most important factors influencing the decision to perform OBMS were training and the role of the GP trainer; fear of having to work alone and having to solve unexpected complications; and the influence of collaboration, organization, and facilities in the GP’s own practice.
Conclusions: The increasing demand for OBMS in primary care centers requires more attention to training aspects, the existing fear, adequate reimbursement for special accreditation, and collaboration and organization. We expect that addressing these factors will result in the strengthening of primary care, improving patient safety, lower referral rates, and a reduction in health care costs.
Office-based minor surgery (OBMS) has traditionally been a feature of general practice.1-11 OBMS refers to all surgical procedures performed under local anesthetic, typically in the office setting. This includes a wide variety of procedures, ranging from minor excisions of dermatological imperfections and tumors, incision of abscesses, suturing wounds, and removing foreign objects, to more therapeutic procedures such as elective partial matrixectomy and thrombosed hemorrhoid treatment. In the Dutch setting, about 70% of these OBMS are performed by general practitioners while about 30% are still performed by surgeons in hospitals.12, 13 When performed by GPs as a service to their patients, OBMS is cost effective and appreciated by patients, as they do not have to be referred for hospital-based care.3, 4, 7, 9, 14, 15 Also in the United States, a recent study showed a positive effect of minor surgical procedures performed in primary care on the costs of care.15 In the Netherlands, for example, the insurance reimbursement for OBMS performed by GPs is about 20% of the reimbursement for hospital-based procedures. Additionally, these costs are fully paid for by the insurance companies. All Dutch patients have a GP for primary care. These GPs can choose to perform OBMS themselves or refer their patients to hospital-based care. Although all Dutch inhabitants are insured for medical expenses, they must pay the obligatory deductible for hospital-based care. There is no deductible for GP care.
Regular performance of OBMS was shown to result in increased satisfaction among GPs. 16 Despite the advantages of performing OBMS in primary care, research in different countries showed great variation in the numbers of GPs performing OBMS and in GP referral rates.4, 7, 8, 9, 11
This variation may be partly due to safety concerns associated with OBMS in general practice.5, 10, 11, 14, 17-22 Previous studies have reported that safety depends on the skills and training of the GP.5,21,22 Some therefore suggest that, to enhance safety, specific skills are required in order to perform OBMS.5, 20, 21, 23 Dutch GPs are expected to have the basic skills required to perform minor surgery after completing their GP training. Therefore, in the Netherlands, as in some other countries, there is no official accreditation for GPs performing OBMS.6, 13
The improvement of primary care is a key issue in international comparative research. Due to the cutbacks in developed countries’ health care budgets, an increase in skin disorders, and the shift in care from hospitals to general practice, there is an increasing demand for OBMS. 2 An Irish study described the importance of an accreditation system to ensure high quality for OBMS in primary care. 6 No literature is available on the attitude of GPs towards OBMS, or on the factors influencing the performance of OBMS by GPs. More knowledge about these factors is essential to determine the conditions under which GPs are willing to perform OBMS.
In this study we aim to identify the facilitators and barriers influencing GPs in deciding whether to perform OBMS.
We performed a qualitative study using focus groups.24 The Ethical Review Board of the NVMO Dutch Association for Medical Education (NVMO, file number 2018-1024) ruled this study did not fall within the remit of the Medical Research Involving Human Subject Acts (WMO) because of its noninvasive character. In 2015 we organized a pilot meeting moderated by an experienced moderator. We used the data from this pilot meeting to draw up the initial and follow-up questions.
Context
In the Netherlands, GP training after basic medical training lasts 3 years. In the first and third years, GP trainees work in GP practices, supervised by GP trainers. One day per week GP trainees take courses at one of the eight institutes for GP specialty training, where they are taught by GP teachers. In the second year of the training program, GP trainees work in a variety of clinical settings, supervised by clinical trainers. Because not all GP trainers perform OBMS and not all trainees work in surgical settings in their second year, not all GP graduates will learn how to perform OBMS.
Sampling Methods
Participants for the pilot meeting were recruited during a monthly national meeting for GPs and GP trainers. In addition, we used purposive sampling and approached GPs and GP trainers working in different settings by invitation. We selected potential participants based on practice circumstances (GP trainers/GPs; rural area with hospitals further away/big cities with hospitals nearby; working alone/with colleagues). We obtained written informed consent from each participant prior to the focus group.
Data Collection
We arranged four 60-minute focus group meetings throughout the Netherlands in the period between 2015 and 2018. We used the data from the pilot meeting in 2015 to draw up the initial and follow-up questions. Initially, it proved difficult to organize focus groups of busy GPs, delaying the process. Therefore, we scheduled the focus group sessions in combination with other meetings and postgraduate training.
Each focus group meeting began with the question, “Why do some GPs perform OBMS while others do not?”
The starting question was formulated in such a way that the participating GPs would think beyond their own reasons for performing or not performing OBMS. We deliberately did not provide detailed examples to ensure an open discussion. We made audio recordings and verbatim transcriptions of the focus group sessions.
The study was performed by three researchers: a physician/head of research department (N.v.D.), a GP instructor/researcher with a focus on practical skills (H.G.A.J.L.), and a GP trainer/researcher (H.v.d.D.). The focus group meetings were moderated by F.D. and H.G.A.J.L. All four groups were observed, and field notes were taken by H.v.d.D.
Data Analysis
All four verbatim transcriptions were analyzed independently by two researchers (H.G.A.J.L., H.v.d.D.) according to the principles of content analysis. Following thematic open coding of all transcripts, results were compared, and categories defined. A check to ensure all statements were categorized in the same agreed categories was performed during successive meetings.
A total of 31 GPs participated in four focus groups (Table 1). Each focus group consisted of participants unfamiliar with the other members of their group. After three of these four focus groups, no new themes were identified. Only subtle differences between the GP trainers and GPs were observed, so we concluded that data saturation was reached.
Analysis resulted in a comprehensive list of facilitators and barriers, divided into three categories (Figure 1).
|
Focus Groups
|
Number of Participants
|
Male
|
Female
|
Age in Years
|
Feature of General Practice
|
Location of General Practice
|
|
1
|
7
|
5
|
2
|
40-59
|
Center* GP: 4
Employed§ GP: 1
Solo# GP: 2
|
City: 3
Suburb: 1
Rural: 3
|
|
2
|
8
|
6
|
2
|
39-62
|
Center GP: 5
Employed GP: 2
Solo GP: 1
|
City: 2
Suburb: 2
Rural: 4
|
|
3
|
7
|
5
|
2
|
52-62
|
Center GP: 4
Employed GP: 1
Solo GP: 2
|
City: 3
Suburb: 2
Rural: 2
|
|
4
|
9
|
3
|
6
|
42-67
|
Center GP: 6
Employed GP: 1
Solo GP: 2
|
Suburb: 9
|
Patient-Related Factors
GPs stated patients preferred OBMS by their GP because it is less time consuming, closer to home, more comfortable, and felt like an additional service.
Other patients preferred to be referred to a specialist, expecting more experienced doctors:
The opposite happened to me: I was hesitant about a procedure, where the patient indicated that she really wanted me to do it.
Some patients were not aware their GP performed OBMS; GPs had to mention this on their website or in their pamphlet.
We have written extensively in our leaflet and on our website that if someone has a wound or requires first aid, they can come to the practice without an appointment.
Referring a patient to a colleague GP or establishing a special clinic managed by GPs for OBMS raised the number of OBMS even more, including more complex procedures (eg, vasectomies or upper eyelid lifts).
Practice Organization and Finance-Related Factors
Adequate planning could have a positive effect on performing OBMS. For example, scheduling OBMS at the end of the working day could reduce stress factors eg, the presence of other patients. Assistants play an important role in scheduling enough time and taking over tasks. It appeared beneficial to invest in training and skills of practice assistants. Due to time constraints, GPs were often forced to perform OBMS alone. Therefore, GPs were more likely to refer their patients elsewhere in case of a full schedule. Due to strongly varying incidence of OBMS, doctors can lose experience. On the other hand, practical circumstances such as the availability of good instruments, materials, maintenance protocols, assistance, and an optimal working environment were stimulating factors.
By performing OBMS, GPs wanted to protect their patients from financial consequences and help reduce the national health care budget:
Because of the deductible patients are motivated to go their GP for OBMS.
Also, appropriate financial compensation encouraged GPs to perform OBMS themselves.
GP-Related Factors
Education or Work Experience Before and During GP Traineeship. GPs mentioned performing surgical procedures before entering GP traineeship gave them a head start in performing OBMS as a GP:
I learned the most when I worked in the emergency room.
Therefore, some trainees are already better trained than their GP trainers and can even train GP trainers and the practice assistants, causing GP trainers to feel insecure and afraid of not being able to act in the event of complications due to the the OBMS performed by the GP trainee.
GP trainees with sufficient training in OBMS during their GP traineeships frequently performed OBMS as a GP after graduation, while low incidence of OBMS, competition from peers, and GP trainer with lack of enthusiasm or skills in OBMS all had a negative influence on performing OBMS. However, teaching trainees could also have a stimulating effect on the GP trainer. Moreover, many GP trainers were convinced that all GPs should learn how to perform OBMS and discover their own limits in this respect:
We use the method of “see one, do one, teach one.” First, I show the procedure to the trainee, then I supervise the trainee when he/she performs the procedure, and when the trainee shows to be adequate in performing the procedure, the trainee can perform it without direct supervision.
GP trainers felt responsible for both trainees and the safety of their patients.
GPs’ Fear of Performing OBMS. Complications related to OBMS led to fear of failure, poor results, and complaints from patients. Fear could also arise due to poor planning, lack of available assistance, lack of time due to emergencies coming in, or due to impatient patients:
One of them had a bad experience once, and never did it again.
Usually, these fears did not materialize; results were better than expected. It was reassuring that even referred patients were often treated by trainees, less experienced than the GPs themselves, and that OBMS performed by hospital doctors could also show poor results.
Work Satisfaction. Some GPs took pleasure in performing OBMS, by seeing the results immediately, and by enjoying the variety in their daily activities. During OBMS, GPs had time for a social conversation with the patient, enhancing the relationship:
I think it’s fantastic. Really tangible. Finally getting to do something. Finally having a visible result. Fantastic. Better than someone who’s tired.
Collaboration, Consultation, and Support in Daily Practice. The benefit of collaboration was the opportunity to ask for practical help and mental support. When GPs worked as a team, colleagues were able to provide emergency cover, offer assistance, or take over the procedure. Furthermore, subspecializing and therefore a better division of tasks automatically emerged when GPs worked together in a single medical center:
I really noticed that if I had to work with a colleague who didn’t perform OBMS himself or had no affinity with it, it was passed on to me.
The type of surgery and the person in need of the procedure could force GPs to define professional limits. Therefore, cases of suspected melanoma, difficult localization of lipomas, surgery involving children or the face, especially in female patients, were more likely to be referred to a hospital. Another reason for referral was not experiencing patient’s trust, although patients could be thankful afterwards. By contrast, liability for risk when something went wrong could damage the doctor-patient trust relationship.
Most GPs reported that performing OBMS had to be preserved for the GP practice to protect the diversity of their profession. By achieving good results, they felt proud and respected:
Because I have a lot of experience, I notice I also project this onto my patients.
To preserve OBMS for the future and protect professionalism, a recurring wish was better postgraduate education with more focus on practical implementation of new skills.
However, courses could be counterproductive (eg, too much information at once):
But that’s something I didn’t learn properly in yet another course we took on that subject.
Main Findings
Our study showed three different groups of facilitators and barriers influencing GPs in deciding whether to perform OBMS in their general practices in the Netherlands: one concerning practical arguments, one explaining the role of the patient and, and one category concerning the GP and GP training perspectives.
Newly identified and prominent factors were prior experience in surgical interventions of the GP trainee, and therefore the role of the GP trainer,25 fear, and the influence of collaboration, organization, and facilities in the GP’s own practice.
Limitations
This study was performed in the Netherlands, with its specific position and financing of health care. Therefore, the results may only be partially applicable to other countries. On the other hand, due to the observed trends in a high variety of settings, these factors should be similar (or the results should be applicable) in other countries.
Comparison With Existing Literature
An important barrier for performing OBMS is fear. However, Murchie et al demonstrated that patients who received an initial excision for melanoma in primary care did not have poorer survival or increased morbidity compared to those initially treated in hospital care.22 Czarnowski et al emphasized the importance of proper technique, documentation, and knowing one’s limits to achieve a good result.26 So, existing fear may be reduced through optimal practice organization and good education.
Our participants also believed that good training in OBMS will likely increase patient safety. However, the QUALICOPC study concluded that logistical factors, such as consistently more equipment, appeared to have a positive effect on services offered,8 our research added the importance of cooperation with colleagues, practice assistants, and optimal practice and time management. As described by Riain et al, the development of accreditation for OBMS may provide a useful model and minimize risks for patients.6 Perhaps an official accreditation could convince health insurers and government authorities to provide adequate reimbursement.6 A general consensus of which procedures should be always taught, as in US family medicine residencies, could also be helpful in family medicine education in other countries.27
Young et al suggested that additional training appears to benefit learners by better preparing them for settings where a broader scope of practice is needed.28
To cut back referrals and reduce national health care costs, GPs in our cohort emphasized the importance of OBMS in primary care centers, a view supported by Ramdas19 et al and Eide et al.8 To achieve this, adequate reimbursement is key. Without appropriate reimbursement, time-consuming surgical procedures may be deprioritized, as shown by both Eide8 et al and our study.
Reimbursements for GPs are always less than hospital rates.3, 4, 14, 15 Therefore, if GPs perform more OBMS, this can contribute to reduction in health care costs. This is confirmed by the cost-effective effect on the health economy observed by Koelink and Lakasing.2, 3
Recently, more countries have struggled with similar questions: is OBMS a task for primary care? What is necessary to make this possible? Is it safe, and will it reduce national health costs? 1, 5, 6, 7, 9, 10, 11, 14, 18, 20, 21, 23, 27, 29 Nelligan et al demonstrated that OBMS driven entirely by family physicians significantly lowered health spending at their AMC. Perhaps more equitable payment for OBMS (greater than 20% of hospital rates) could still contribute to lower national health care costs, and also better support the GP practices to provide the proper equipment and staffing to provide OBMS in safe and timely manner.
The increasing demand for OBMS in primary care centers requires more attention to training aspects, the existing fear, adequate reimbursement for special accreditation, and collaboration and organization. By addressing these factors, strengthening of primary care, improving patient safety, lower referral rates, and a reduction in health care costs, can all be expected.
Future Research
Future research is needed for designing targeted interventions for education and improving practice organization. Measurable outcomes like improvements in training facilities for family medicine, fewer referrals to hospitals, increased patient safety and quality of care, and reduction in health care costs are needed to encourage governments and health insurers to develop special reimbursements for performing OBMS, and perhaps, to establish an accreditation that is recognizable to patients.
Acknowledgments
The authors thank all the GPs who participated in the focus groups. The authors also thank Dr Frans Dekker for moderating the pilot session and Dr Rinse Barendsen for critically reviewing our manuscript.
References
1. George S, Pockney P, Primrose J, et al. A prospective randomised comparison of minor surgery in primary and secondary care. The MiSTIC trial. Health Technol Assess. 2008;12(23):iii-iv, ix-38. doi:10.3310/hta12230
2. Koelink CJ, Kollen BJ, Groenhof F, van der Meer K, van der Heide WK. Skin lesions suspected of malignancy: an increasing burden on general practice. BMC Fam Pract. 2014;15(1):29. doi:10.1186/1471-2296-15-29
3. Lakasing E. Restricting minor surgery in general practice: another example of financial short-termism. Br J Gen Pract. 2010;60(574):385-386. doi:10.3399/bjgp10X502029
4. van Dijk CE, Verheij RA, Spreeuwenberg P, Groenewegen PP, de Bakker DH. Minor surgery in general practice and effects on referrals to hospital care: observational study. BMC Health Serv Res. 2011;11(2):2. doi:10.1186/1472-6963-11-2
5. Botting J, Correa A, Duffy J, Jones S, de Lusignan S. Safety of community-based minor surgery performed by GPs: an audit in different settings. Br J Gen Pract. 2016;66(646):e323-e328. doi:10.3399/bjgp16X684397
6. Ní Riain A, Collins C, O’Sullivan T. Developing accreditation for community based surgery: the Irish experience. Leadersh Health Serv (Bradf Engl). 2018;31(1):33-46. doi:10.1108/LHS-01-2017-0001
7. Menahem S, Nazarenko A, Shvartzman P. Minor surgical procedures and musculoskeletal injections by primary care physicians - an Israeli experience. Isr J Health Policy Res. 2014;3(1):12. doi:10.1186/2045-4015-3-12
8. Eide TB, Straand J, Björkelund C, et al. Differences in medical services in Nordic general practice: a comparative survey from the QUALICOPC study. Scand J Prim Health Care. 2017;35(2):153-161. doi:10.1080/02813432.2017.1333323
9. van Dijk CE, Korevaar JC, Koopmans B, de Jong JD, de Bakker DH. The primary-secondary care interface: does provision of more services in primary care reduce referrals to medical specialists? Health Policy. 2014;118(1):48-55. doi:10.1016/j.healthpol.2014.04.001
10. Ferguson HJ, Fitzgerald JE, Reilly J, Beamish AJ, Gokani VJ; Council of the Association of Surgeons in Training. A cross sectional study of surgical training among United Kingdom general practitioners with specialist interests in surgery. BMJ Open. 2015;5(4):e007677. doi:10.1136/bmjopen-2015-007677
11. Ní Riain A, Maguire N, Collins C. Minor surgery in general practice in Ireland- a report of workload and safety. BMC Fam Pract. 2020;21(1):115. doi:10.1186/s12875-020-01186-x
14. Taib A, Hammill C, Abraham A, et al. Provision of a local anaesthetic minor procedures service by surgical advanced clinical practitioners: 5-year study. BJS Open. 2021;5(5):73. doi:10.1093/bjsopen/zrab073
15. Nelligan I, Montacute T, Browne MA, Lin S. Impact of a family medicine minor procedure service on cost of care for a health plan. Fam Med. 2020;52(6):417-421. doi:10.22454/FamMed.2020.334308
16. Rivet C, Ryan B, Stewart M. Hands on: is there an association between doing procedures and job satisfaction? Can Fam Physician. 2007;53(1):93, 93, 1-5, 92.
17. Smith AL, Watts CG, Robinson S, et al; Australian Melanoma Centre of Research Excellence Study Group. GPs’ involvement in diagnosing, treating, and referring patients with suspected or confirmed primary cutaneous melanoma: a qualitative study. BJGP Open. 2020;4(2):bjgpopen20X101028. doi:10.3399/bjgpopen20X101028
18. Korgul R, Holme SA. Factors influencing skin cancer excision rates in Scottish primary care. Clin Exp Dermatol. 2018;43(4):441-444. doi:10.1111/ced.13360
19. Ramdas K, van Lee C, Beck S, et al. Differences in rate of complete excision of basal cell carcinoma by dermatologists, plastic surgeons and general practitioners: a large cross-sectional study. Dermatology. 2018;234(3-4):86-91. doi:10.1159/000490344
20. van Rijsingen MC, Vossen R, van Huystee BE, Gorgels WJ, Gerritsen MJ. Skin tumour surgery in primary care: do general practitioners need to improve their surgical skills? Dermatology. 2015;230(4):318-323. doi:10.1159/000371812
21. van Rijsingen MC, van Bon B, van der Wilt GJ, Lagro-Janssen AL, Gerritsen MJ. The current and future role of general practitioners in skin cancer care: an assessment of 268 general practitioners. Br J Dermatol. 2014;170(6):1366-1368. doi:10.1111/bjd.12935
22. Murchie P, Amalraj Raja E, Brewster DH, Iversen L, Lee AJ. Is initial excision of cutaneous melanoma by General Practitioners (GPs) dangerous? Comparing patient outcomes following excision of melanoma by GPs or in hospital using national datasets and meta-analysis. Eur J Cancer. 2017;86:373-384. doi:10.1016/j.ejca.2017.09.034
23. Collins AM, Ridgway PF, Hassan MS, Chou CW, Hill AD, Kneafsey B. Surgical instruction for general practitioners: how, who and how often? J Plast Reconstr Aesthet Surg. 2010;63(7):1156-1162. doi:10.1016/j.bjps.2009.05.023
24. Stalmeijer RE, Mcnaughton N, Van Mook WN. Using focus groups in medical education research: AMEE Guide No. 91. Med Teach. 2014;36(11):923-939. doi:10.3109/0142159X.2014.917165
25. Jochemsen-van der Leeuw HG, van Dijk N, Wieringa-de Waard M. Assessment of the clinical trainer as a role model: a Role Model Apperception Tool (RoMAT). Acad Med. 2014;89(4):671-677. doi:10.1097/ACM.0000000000000169
26. Czarnowski C, Ponka D, Rughani R, Geoffrion P. See one. Do one. Teach one.: office-based minor surgical procedures. Can Fam Physician. 2008;54(6):893.
27. Nothnagle M, Sicilia JM, Forman S, et al; STFM Group on Hospital Medicine and Procedural Training. Required procedural training in family medicine residency: a consensus statement. Fam Med. 2008;40(4):248-252.
28. Young RA, Casey D, Singer D, Waller E, Carney PA. Early career outcomes of family medicine residency graduates exposed to innovative flexible longitudinal tracks. Fam Med. 2017;49(5):353-360.
29. White B. The state of family medicine. Fam Pract Manag. 2012;19(1):20-26.



There are no comments for this article.