Background and Objectives: Visual learning equity is a health justice effort in response to the lack of representation of brown and black skin images in medical education. This paucity creates a knowledge gap and decreases providers’ competence in managing skin disease in minoritized populations. Herein, we aimed to create a standardized course auditing system to assess the use of brown and black skin images in medical education.
Methods: We performed a cross-sectional analysis of the 2020-2021 preclinical curriculum at one US medical school. All human images in the learning material were analyzed. Skin color was categorized as light/white, medium/brown, and dark/black using the Massey-Martin New Immigrant Survey Skin Color Scale.
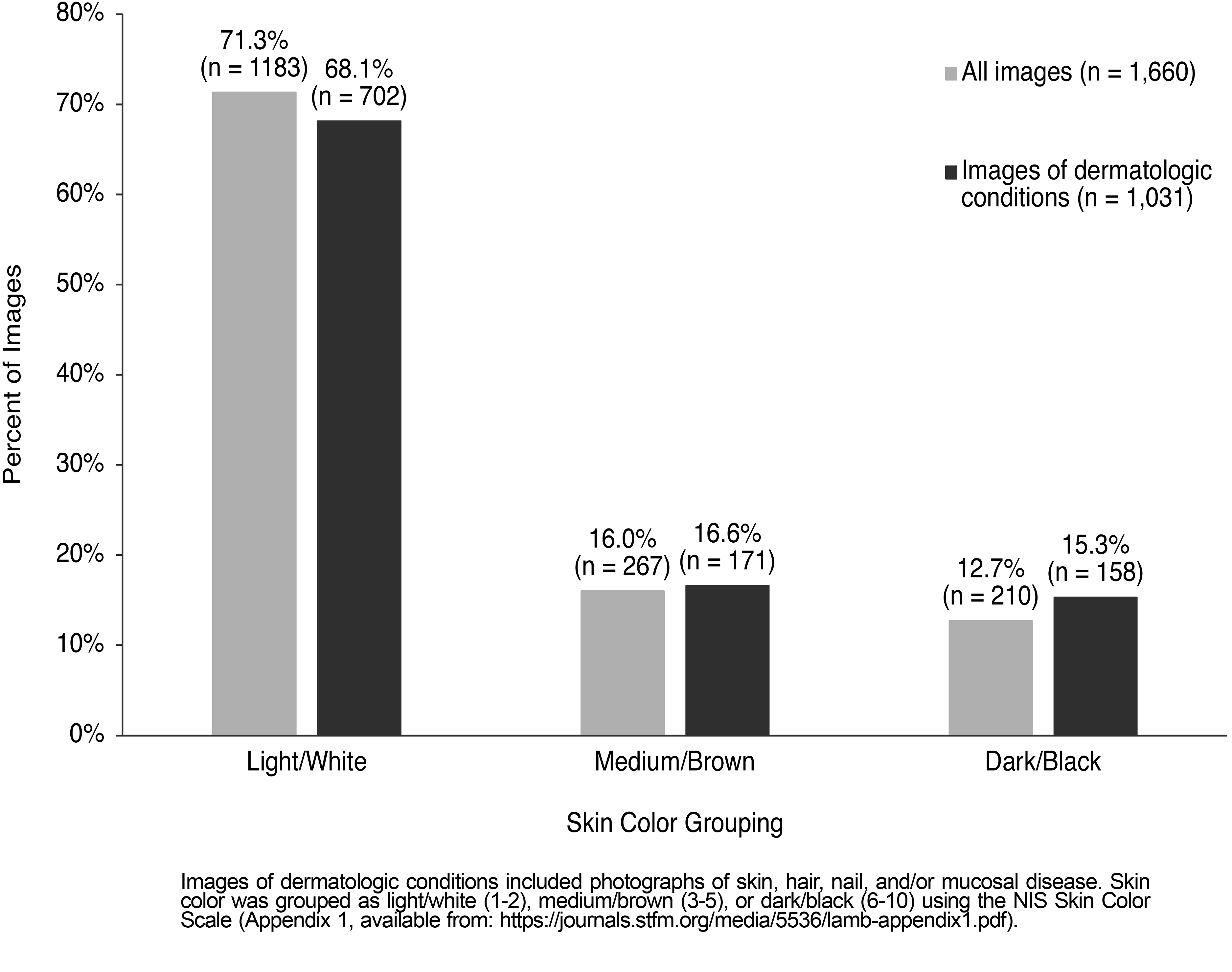
Results: We included 1,660 unique images in our analysis; 71.3%, (n=1,183) were light/white, 16.1% (n=267) were medium/brown and 12.7% (n=210) were dark/black. Dermatologic images of skin, hair, nails, or mucosal disease made up 62.1% (n=1,031) of the images and 68.1% (n=702) were light/white. The pulmonary course presented the highest proportion of light/white skin (88.0%, n=44/50) and the dermatology course presented the lowest proportion of light/white skin (59.0%, n=301/510). Images of infectious diseases were more frequently presented in darker skin colors (χ2 [2]=15.46, P<.001).
Conclusions: Light/white skin was the standard used for visual learning images in the medical school curriculum at this institution. The authors outline steps to perform a curriculum audit and diversify medical curricula to ensure the next generation of physicians are educated to care for all patients.
Visual learning equity is a term coined to represent the health justice effort to increase the representation of brown and black skin color images in medical education. Previous studies have demonstrated that in dermatology textbooks targeted to both dermatologists and internists, approximately 80% of the images are of white skin. 1 Additionally, there is a documented paucity of brown and black skin images in internal medicine and dermatology residency didactic material, 2, 3 medical school textbooks, 4 and popular United States Medical Licensing Examination (USMLE) preparatory resources. 5
This lack of diverse skin images in medical training creates a knowledge gap that affects dermatologists as well as primary care providers (PCPs). 6, 7 PCPs commonly manage dermatologic conditions and typically serve as the front line for evaluating and treating skin disease. More than half of all outpatient skin-related visits are seen by family medicine, internal medicine, pediatric, and emergency medicine providers. 8 However, these health professionals frequently report feeling poorly trained in managing dermatologic concerns, and report low confidence in their ability to identify and treat basic skin conditions in people with brown and black skin. 7 Due to health professionals’ lack of competency in treating skin conditions in all populations, people with brown and black skin may experience delayed or missed diagnoses, which contributes to known skin health disparities. 9- 11
As the medical school curriculum is the major source of learning for medical students, we aim to determine if similar gaps in brown and black skin color representation exist within preclinical course material. Previous studies of medical school curricula have focused broadly on the representation of race and race portrayal in case examples. 12, 13 It is important to note that race is distinct from skin color. Skin color is a biologic feature determined by the amount, type, and epidermal distribution of the cutaneous pigment melanin and the skin’s reaction to environmental factors such as sunlight. The visible color of the skin contributes to the appearance of skin disease. Race, however, is a societal construct that classifies people based on skin color, hair texture, and other physical and social traits. Skin color and race are often conflated; however, skin color does not directly translate to race, and race does not directly translate to skin color.
Herein, we focus on the inclusion of diverse skin color images in the preclinical curriculum at the University of Pittsburgh School of Medicine (UPSOM). We assess the associations of skin color with medical and dermatologic diagnoses, stigmatized diseases, and depiction of health care professionals. With a focus on health justice, we present a standardized course auditing system and outline actions steps for curriculum reform with the goal of equitable representation of a spectrum of skin colors. We also recommend resources with brown and black skin images in the hopes that other institutions will take similar actions to achieve visual learning equity.
Data Collection
We evaluated all course material for the 2020-2021 preclinical curriculum at UPSOM including lecture PowerPoint slides, course syllabi, group workshop material, and exam items posted on the course websites of all 34 first- and second-year medical school courses. We reviewed all human images of subjects representing a person with a medical condition or exam finding, undergoing a treatment or procedure, as well as images of patient-physician interactions. For each image, we recorded the corresponding diagnosis/representation along with the respective course. Images of skin, hair, nail, or mucosal disease were coded as dermatologic conditions. We also recorded if the image portrayed an infectious disease. Duplicate images, drawings and cartoons, and images in which background skin color could not be determined due to poor image quality or closeup of mucosa, nails, palms, or soles, were excluded. This study was considered exempt under educational settings by the University of Pittsburgh Institutional Review Board.
Measurements
To score the skin color of the images, we used the Massey-Martin New Immigrant Survey (NIS) Skin Color Scale. 14 While most studies have used Fitzpatrick Skin Types as a proxy for skin color, 15 this is a phototyping measurement that categorizes a person’s response to ultraviolet light, which cannot be determined from images. Instead, the NIS Skin Color Scale is a tool developed to assess the skin color of research participants. This scale has a wide range of skin colors, from zero representing absolute white to 10 representing the darkest black skin color. The scale depicts 10 identical hands in increasingly darker skin colors corresponding to points 1 through 10 on the scale (Appendix 1). Prior to data collection, both image reviewers (J.L. and A.S.) received training on use of the NIS Skin Color Scale under the guidance of the senior author (A.J.), a board-certified dermatologist experienced in using the scale in prior research. 1 We matched the skin color of the subjects in the images to a numbered hand on the scale and coded skin colors 1-2 as light/white, 3-5 as medium/brown, and 6-10 as dark/black. Previous studies using the NIS Skin Color Scale to categorize skin color of images in medical textbooks also reported these skin color groupings. 1, 4, 16
Statistical Analysis
We used descriptive statistics to summarize the data. We used χ2 tests to examine associations of proportion of skin color (light/white, medium/brown, and dark/black) with specific diagnoses, including whether the diagnosis was an infectious disease. We performed statistical analyses using SPSS Statistics for Windows, Version 27.0.
Interrater Reliability
One reviewer scored the skin color of all the images included in the analysis. Using a random number generator, we selected 10% of the total images for the second reviewer to score, resulting in a percent agreement of 83% and Cohen’s κ of 0.64.
We examined 1,775 pieces of learning material (PowerPoint documents, course syllabi, workshop handouts, and exams) over the course of 2 months. In total, 1,660 unique images were included in this study; 71.3%, (n=1,183) of these images were scored as light/white skin. Medium/brown and dark/black skin images made up a smaller proportion of the total, 16.1% (n=267) and 12.7% (n=210), respectively. Of the total images, 62.1% (n=1,031) were dermatologic images of skin, hair, nail, or mucosal disease. The proportion of dermatologic images across the three skin color groupings was similar to the overall distribution, with 68.1% (n=702) of these images being light/white (Figure 1).
Table 1 shows the proportion of images across the three skin color groupings for each course in the preclinical curriculum. The dermatology course presents the greatest number of images (n=510), followed by the microbiology (n=157) and immunology courses (n=118). Of the courses with more than 15 total images, the pulmonary course presents the highest proportion of light/white skin (88.0%, n=44/50) and the dermatology course presents the lowest proportion of light/white skin images (59.0%, n=301/510). Five courses presented no images of dark/black skin (pulmonary course 0/50 images, neuroscience course 0/45 images, hematology course 0/9 images, evidence-based medicine course 0/1 images, and introduction to being a physician course 0/1 images). Of the total 158 dermatologic images of dark/black skin presented throughout all the learning material, 72% (n=114) are from the dermatology course, with less than 50 dermatologic images of dark/black skin displayed in all other preclinical courses.
|
Course Title a
|
Total Number of Images, n
|
Images of Light/White Skin Color, n (%)
|
Images of Medium/Brown Skin Color, n (%)
|
Images of Dark/Black Skin Color, n (%)
|
|
All images
|
1,660
|
1,183 (71.3)
|
267 (16.1)
|
210 (12.7)
|
|
Dermatology
|
510
|
301 (59.0)
|
95 (18.6)
|
114 (22.4)
|
|
Medical Microbiology
|
157
|
107 (68.2)
|
29 (18.5)
|
21 (13.4)
|
|
Immunology in Health & Disease
|
118
|
95 (80.5)
|
15 (12.7)
|
8 (6.8)
|
|
Musculoskeletal
|
95
|
83 (87.4)
|
10 (10.5)
|
2 (2.1)
|
|
Advanced Physical Exam
|
89
|
57 (64.0)
|
16 (18.0)
|
16 (18.0)
|
|
Introduction to Physical Exam
|
82
|
68 (82.9)
|
11 (13.4)
|
3 (3.7)
|
|
Tissues in Health & Disease
|
71
|
54 (76.1)
|
14 (19.7)
|
3 (4.2)
|
|
Endocrinology
|
64
|
52 (81.3)
|
7 (10.9)
|
5 (7.8)
|
|
Digestion & Nutrition
|
58
|
45 (77.6)
|
9 (15.5)
|
4 (6.9)
|
|
Medical Anatomy
|
51
|
37 (72.5)
|
10 (19.6)
|
4 (7.8)
|
|
Reproductive & Developmental Biology
|
51
|
42 (82.4)
|
3 (5.9)
|
6 (11.8)
|
|
Pulmonary
|
50
|
44 (88.0)
|
6 (12.0)
|
0 (0.0)
|
|
Neuroscience
|
45
|
39 (86.7)
|
6 (13.3)
|
0 (0.0)
|
|
Human Genetics
|
39
|
31 (79.5)
|
4 (10.3)
|
4 (10.3)
|
|
Renal
|
29
|
22 (75.9)
|
4 (13.8)
|
3 (10.3)
|
|
Cardiology
|
28
|
19 (67.9)
|
8 (28.6)
|
1 (3.6)
|
|
Psychiatry
|
24
|
17 (70.8)
|
6 (25.0)
|
1 (4.2)
|
|
Fuel Metabolism
|
20
|
15 (75.0)
|
2 (10.0)
|
3 (15.0)
|
|
Clinical Experiences
|
17
|
12 (70.6)
|
3 (17.6)
|
2 (11.8)
|
|
Behavioral Medicine
|
16
|
12 (75.0)
|
2 (12.5)
|
2 (12.5)
|
|
Pharmacology
|
14
|
9 (64.3)
|
0 (0.0)
|
5 (35.7)
|
|
Ethics, Law and Professionalism
|
11
|
7 (63.6)
|
2 (18.2)
|
2 (18.2)
|
|
Population Health
|
10
|
5 (50.0)
|
4 (40.0)
|
1 (10.0)
|
|
Hematology
|
9
|
8 (88.9)
|
1 (11.1)
|
0 (0.0)
|
|
Evidence Based Medicine
|
1
|
1 (100.0)
|
0 (0.0)
|
0 (0.0)
|
|
Introduction to Being a Physician
|
1
|
1 (100.0)
|
0 (0.0)
|
0 (0.0)
|
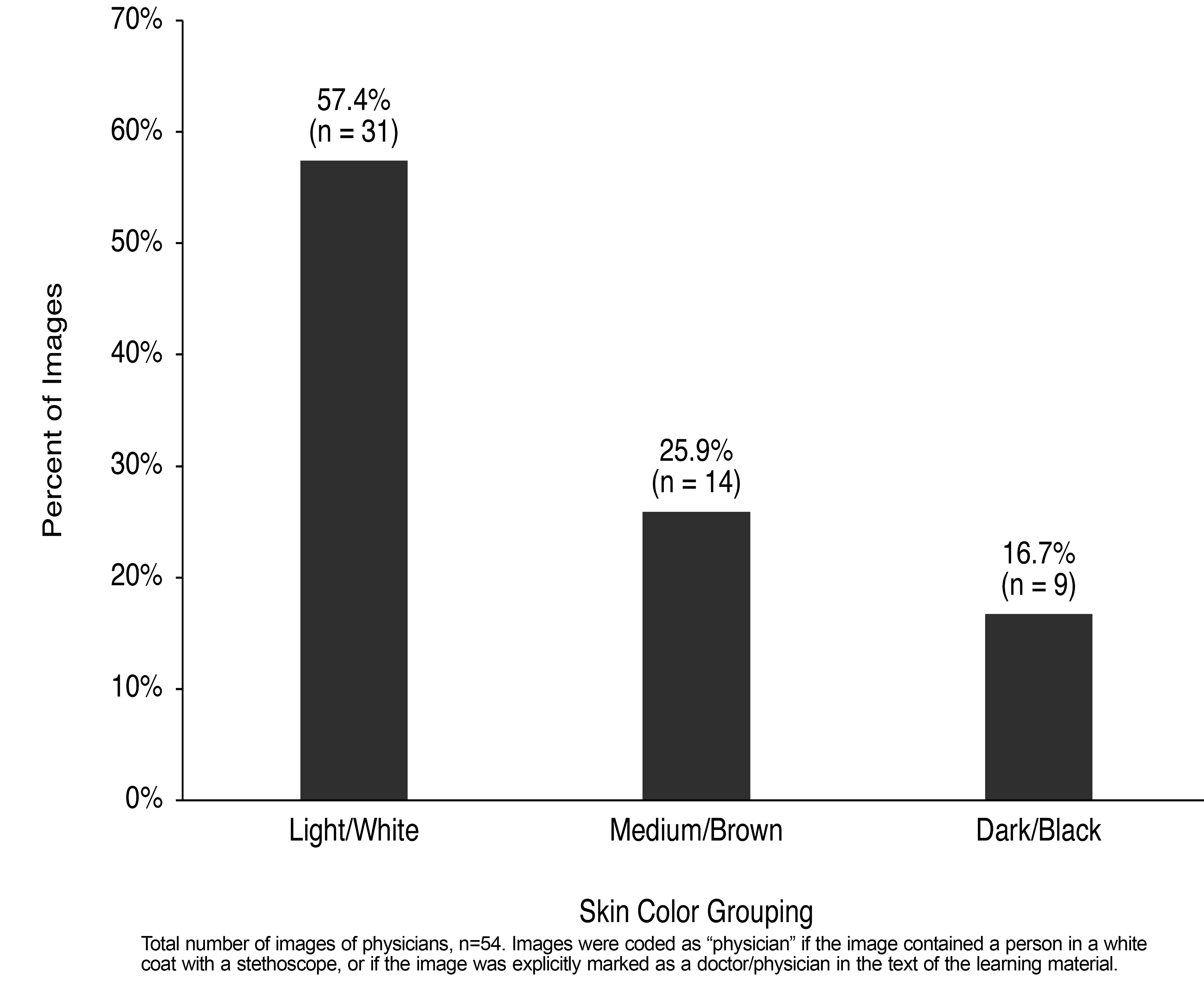
There were 54 images of physicians depicted in the learning material; 57.4% (n=31) of the physicians had light/white skin, 25.9% (n=14) had medium/brown skin and 16.7% (n=9) had dark/black skin (Figure 2).
Images of medium/brown and dark/black skin were shown most frequently with diagnoses of tinea infections, systemic lupus erythematous, cholera, psoriasis, atopic dermatitis, and seborrheic keratoses. Additionally, there was a significant association between skin color grouping and infectious diseases (χ2=15.46, P<.001). Skin color scores on the 11-point NIS Skin Color Scale were significantly higher in the images related to infectious diseases compared to images not related to infectious diseases (Z=-3.44, P<.001).
Our results demonstrate that light/white skin is the standard used for visual learning images in preclinical medical education at this institution. We found that in all images of patients throughout the learning material, 71% had light/white skin. While these results are from a single, large academic institution, our findings further substantiate the lack of images of brown and black skin used in medical education.
Previous studies have suggested that the representation of skin color used in medical education should be representative of the general population. 4, 13, 17 However, the United States (US) population is becoming increasingly more diverse. The US Census Bureau projects that by 2044 the majority of the US population will have nonwhite skin. 18 We argue that the learning environment should strive for equal representation of all skin colors to prepare students to care for all populations. Based on this standard, skin conditions should be presented on a spectrum of skin colors including images of light/white, medium/brown, and dark/black skin to demonstrate differences in disease manifestations based on constitutive skin color.
While overall light/white skin was overrepresented in the learning material, we found that images of infectious diseases were more frequently represented in medium/brown and dark/black skin. This pattern has been previously identified in studies analyzing images in medical textbooks, which show that dark skin is overrepresented in chapters on infectious diseases, particularly in images of sexually transmitted infections, while dark skin is underrepresented elsewhere throughout the same text. 9, 19 Transmissible diseases are historically viewed as socially undesirable and threatening to others, which can lead to social stigma. 20 Overrepresentation of medium/brown and dark/black skin depicting these stigmatized diseases can contribute to harmful stereotypes about negative health behaviors and can lead to suboptimal care. 21 This may also cause learners to make inappropriate associations between skin color and disease risk. 21
Additionally, our analysis showed that more than half (57.4%) of the images of physicians in the learning material had light/white skin. We must be mindful of this type of representation in medical education as leaders are calling to diversify the field. Images used to teach undergraduate and graduate medical trainees portray more than just the appearance of skin disease. The dominant portrayal of light/white skin in photographs of physicians can contribute to the “hidden curriculum,” which refers to the unspoken and often unintended lessons, values, and norms that exist in the educational setting. 22 As formal medical education emphasizes the importance of diversity and equity, the unequal representation of skin color contradicts these explicit classroom lessons. 23
Lastly, we found that there were different proportions of skin color representation between the preclinical courses. This difference in representation may be the result of alternative resource utilization and awareness. Educators who are not dermatologists may be more likely to use images from medical textbooks or search engines to find examples of skin disease. Kamath et al demonstrated that the majority of search results for common dermatologic conditions on Google, Bing, and Yahoo are of light/white skin.1 There are many examples of bias inherent in Google’s search algorithms, and if our resources are racially biased, this may impact the images used to teach our future clinicians. 24, 25 In Appendix 2 we recommend several resources, including textbooks and free online image databases, that focus specifically on presenting dermatologic conditions in brown and black skin. Images from these resources can be utilized by all educators to diversify course content.
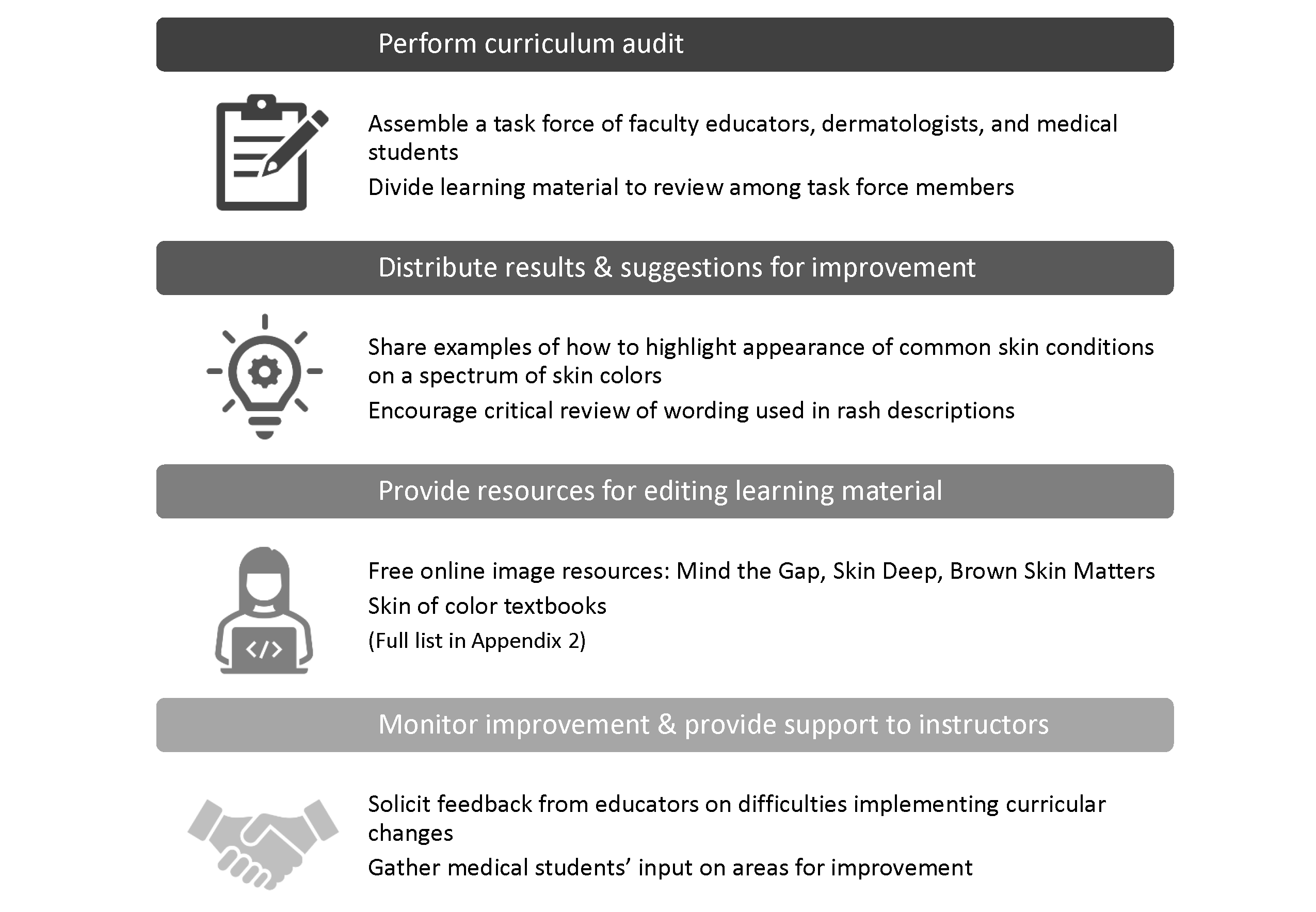
On average, medical institutions require less than 5 hours of preclinical time devoted to dermatology education. 26 In our study, more than half of the images of skin disease depicted in the learning material came from courses other than the dermatology course. For this reason, studies focusing solely on dermatology lecture slides are limited, as they may miss the majority of skin education in other medical school courses. We urge faculty to analyze all course material presented to students and trainees, regardless of whether the topic explicitly addresses skin diseases. Using our process as a model, we outline specific steps for implementing a course audit and suggestions for curricular reform in Figure 3. Institutions may decide to perform their own audit or move directly to advising all medical educators to include a spectrum of skin colors in their visual learning images.
This study has several limitations. Data were collected from one US medical school, which limits the generalizability of our results. We also narrowed our assessment to learning material in the preclinical years and did not analyze educational content presented to students during the third and fourth years. There is no consensus on a validated scale for standardized assessment of skin color for research. We selected the NIS Skin Color Scale for its wide variety of skin colors; however, the NIS Skin Color Scale has not been validated for use of scoring images. Visual scoring of skin color with any scale is subjective and can vary based on a viewer’s personal characteristics and contextual situation. 27 We had one independent reviewer score 10% of the images with significant interrater agreement, however, future analyses would be improved by use of computer image processing to objectively score skin color. We recognize that skin color stratification can contribute to the persistence of colorism, the historical discrimination against people with darker skin color in our society. However, we focus on color as a descriptive term based on the biologic impact of melanin causing variable visual presentation of skin conditions on the range of light/white, medium/brown, or dark/black skin color. Lastly, we did not assess representation of race or ethnicity in preclinical medical education, as we were not able to evaluate written or verbal discussions on race, particularly the use of race identifiers in cases or discussions of racial health disparities throughout the curriculum.
Despite these limitations, our project is novel in highlighting disparities in representation of skin color used in the medical school curriculum. Future studies could benefit from a comprehensive course audit assessing representation of race/ethnicity, gender, ability status, and body size, in addition to skin color, within the medical school curriculum. Additional research is needed to assess how visual learning images impact students’ medical knowledge as well as their attitudes and beliefs about patients and disease states.
Studies suggest that physicians’ inability to identify the erythema migrans rash, a sign of early Lyme disease, among people with dark skin may explain why people identified as Black race are more likely to present with late-stage Lyme disease compared to people identified as White race. 10, 28 Additionally, Black patients with melanoma present at later stages and have worse survival outcomes compared to White counterparts. 11 Lack of competency in assessing skin conditions in people with black and brown skin may negatively impact the patient-provider relationship and reinforce the mistrust of the health care system in this population. 9 It is imperative that we analyze and revise medical school curricula, because inequitable visual learning images impact learning and result in negative health outcomes for people with brown and black skin. Clinician educators, medical education faculty, and students will need to collaborate to change the current educational structure to one that promotes diversity and equity in medical education and ensure that the next generation of health professionals are educated to care for all patients.
Acknowledgments
The authors thank Li Wang, MS, and Philip J. Grosse, PhD, at the Clinical and Translational Sciences Institute at the University of Pittsburgh for statistical consultation.
References
-
Kamath P, Sundaram N, Morillo-Hernandez C, Barry F, James AJ. Visual racism in internet searches and dermatology textbooks.
J Am Acad Dermatol. 2021;85(5):1348-1349.
doi:10.1016/j.jaad.2020.10.072
-
Nijhawan RI, Jacob SE, Woolery-Lloyd H. Skin of color education in dermatology residency programs: does residency training reflect the changing demographics of the United States?
J Am Acad Dermatol. 2008;59(4):615-618.
doi:10.1016/j.jaad.2008.06.024
-
Mundluru SN, Ramalingam ND, Tran HN. Skin in the Game-Taking Skin of Color Dermatology to the Classroom.
J Grad Med Educ. 2019;11(3):336-337.
doi:10.4300/JGME-D-18-00900.1
-
-
Jones VA, Clark KA, Shobajo MT, Cordova A, Tsoukas MM. Skin of color representation in medical education: an analysis of popular preparatory materials used for United States Medical Licensing Examinations.
J Am Acad Dermatol. 2021;85(3):773-775.
doi:10.1016/j.jaad.2020.07.112
-
Buster K, Yang L, Elmets C. Are dermatologists confident in treating skin disease in African-Americans? presented at: J Invest Dermatol Meeting Abstracts; 2011.
-
Mundluru SN, Ramalingam ND, Tran HN. Addressing Internal Medicine Residents’ Discomfort With Basic Dermatology in Persons of Color in the Primary Care Clinic.
Am J Med Qual. 2019;34(5):513.
doi:10.1177/1062860619850130
-
Wilmer EN, Gustafson CJ, Ahn CS, Davis SA, Feldman SR, Huang WW. Most common dermatologic conditions encountered by dermatologists and nondermatologists. Cutis. 2014;94(6):285-292.
-
Lester JC, Taylor SC, Chren MM. Under-representation of skin of colour in dermatology images: not just an educational issue.
Br J Dermatol. 2019;180(6):1521-1522.
doi:10.1111/bjd.17608
-
Fix AD, Peña CA, Strickland GT. Racial differences in reported Lyme disease incidence.
Am J Epidemiol. 2000;152(8):756-759.
doi:10.1093/aje/152.8.756
-
Dawes SM, Tsai S, Gittleman H, Barnholtz-Sloan JS, Bordeaux JS. Racial disparities in melanoma survival.
J Am Acad Dermatol. 2016;75(5):983-991.
doi:10.1016/j.jaad.2016.06.006
-
Turbes S, Krebs E, Axtell S. The hidden curriculum in multicultural medical education: the role of case examples.
Acad Med. 2002;77(3):209-216.
doi:10.1097/00001888-200203000-00007
-
Martin GC, Kirgis J, Sid E, Sabin JA. Equitable Imagery in the Preclinical Medical School Curriculum: Findings From One Medical School.
Acad Med. 2016;91(7):1002-1006.
doi:10.1097/ACM.0000000000001105
-
Massey DS, Martin JA. The NIS Skin Color Scale. Office of Population Research, Princeton University; 2003.
-
Syder NC, McKenzie S, Omar D, Brown-Korsah JB, Taylor SC, Elbuluk N. Gaps in Medical Education Curricula on Skin of Color in Medical School, Residency, and Beyond.
J Am Acad Dermatol. 2022;S0190-9622(22)00545-X.
doi:10.1016/j.jaad.2022.03.053
-
Rana A, Witt A, Jones H, Mwanthi M, Murray J, Zickuhr L. Representation of Skin Colors in Images of Patients With Lupus Erythematosus [published online ahead of print, 2021 May 31].
Arthritis Care Res (Hoboken). 2021.
doi:10.1002/acr.24712
-
Reilley-Luther J, Cline A, Zimmerly A, Azinge S, Moy J. Representation of Fitzpatrick skin type in dermatology textbooks compared with national percentiles.
Dermatol Online J. 2020;26(12):13030/qt91h8k9zc.
doi:10.5070/D32612051349
-
Colby SL, Ortman JM. Projections of the Size and Composition of the U.S. Population: 2014 to 2060. Curr Popul Rep [Spec Censuses]. 2014;•••:25-1143.
-
Adelekun A, Onyekaba G, Lipoff JB. Skin color in dermatology textbooks: an updated evaluation and analysis.
J Am Acad Dermatol. 2021;84(1):194-196.
doi:10.1016/j.jaad.2020.04.084
-
Fischer LS, Mansergh G, Lynch J, Santibanez S. Addressing Disease-Related Stigma During Infectious Disease Outbreaks.
Disaster Med Public Health Prep. 2019;13(5-6):989-994.
doi:10.1017/dmp.2018.157
-
Dretler AW, Trolard A, Bergquist EP, et al. The influence of race and sex on gonorrhea and chlamydia treatment in the emergency department.
Am J Emerg Med. 2020;38(3):566-570.
doi:10.1016/j.ajem.2019.05.054
-
Alsubaie MA. Hidden Curriculum as One of Current Issue of Curriculum. J Educ Pract. 2015;6(33).
-
Lehmann LS, Sulmasy LS, Desai S; ACP Ethics, Professionalism and Human Rights Committee. Hidden Curricula, Ethics, and Professionalism: Optimizing Clinical Learning Environments in Becoming and Being a Physician: A Position Paper of the American College of Physicians.
Ann Intern Med. 2018;168(7):506-508.
doi:10.7326/M17-2058
-
-
-
McCleskey PE, Gilson RT, DeVillez RL. Medical Student Core Curriculum in Dermatology Survey.
J Am Acad Dermatol. 2009;61(1):30-35.e4.
doi:10.1016/j.jaad.2008.10.066
-
Hill ME. Race of the Interviewer and Perception of Skin Color: Evidence from the Multi-City Study of Urban Inequality.
Am Sociol Rev. 2002;67(1):99-108.
doi:10.2307/3088935
-
Ly DP. Black-white differences in the clinical manifestations and timing of initial Lyme disease diagnoses. J Gen Intern Med. 2022 Aug;37(10):2597-2600. doi: 10.1007/s11606-021-07129-1. Epub 2021 Sep 30.



There are no comments for this article.