Background and Objective: Although the opioid epidemic continues to affect millions of Americans, many family physicians feel underprepared to perform chronic pain management (CPM) and treat opioid use disorder (OUD). To address this gap, we created organizational policy changes and implemented a didactic curriculum to help improve patient care, including medication-assisted treatment (MAT) into our residency. We investigated whether the educational program improved the comfort and ability of family physicians to prescribe opioids and utilize MAT.
Method: Clinic policies and protocols were updated to align with the 2016 Centers for Disease Control and Prevention Guidelines for Prescribing Opioids. A didactic curriculum was created to improve resident and faculty comfort with CPM and introduce MAT. An online survey was completed pre- and postintervention between December 2019 and February 2020, utilizing paired sample t test and percentage effective (z test) to assess for change in provider comfort with opioid prescribing. Assessments were made using clinical metrics to monitor compliance with the new policy.
Results: Following the interventions, providers reported improved comfort with CPM (P=.001) and perception of MAT (P<.0001). Within the clinical setting there was significant improvement in the number of CPM patients who had a pain management agreement on file (P<.001) and completed a urine drug screen within the past year (P<.001).
Conclusion: Provider comfort with CPM and OUD increased over the course of the intervention. We were also able to introduce MAT, adding a tool to the toolbox to help our residents and graduates treat OUD.
The opioid epidemic is a well known and complicated issue gripping the United States. 1, 2 In 2015, 11.5 million Americans misused opioid pain medications, 2 and in 2018, 67,000 Americans died from opioid overdoses. 3 Of those who have misused opioids, 1.9 million have been diagnosed with opioid use disorder (OUD). 2 Medication-assisted treatment (MAT), has been approved for the treatment of OUD; however, as of 2015 only 15,000 of the 435,000 primary care physicians in the United States participate in MAT. 4
Primary care providers (PCPs) write 45% of all opioid prescriptions in the United States, 5 however many physicians note that their training in residency was inadequate to properly provide chronic pain management (CPM) to patients on long-term opioids. 6 In addition, preparation in residency is one of the biggest factors in determining whether a physician will prescribe MAT in practice. 7 Despite the need for early training to improve the number of physicians prescribing MAT, most residencies do not offer the training as part of their program, citing lack of faculty prescribers, competing priorities, and lack of ancillary support (counseling/social work). 8, 9 In recent years, residencies have started implementing changes to address these concerns, however more work is needed to overcome the care deficits in this area. 9, 10
The University of Kansas School of Medicine-Wichita (KUSM-W) Family Medicine Residency Program at Ascension Via Christi (VCFM) sought to implement policy and curriculum changes to help address deficiencies in our care of patients with chronic pain on opioids as well as OUD. The primary objective was to evaluate a skill-based, CPM educational program on the comfort and ability of family physicians to prescribe opioids and utilize MAT.
Our study involved the voluntary participation of 18 faculty family physicians and 46 family medicine residents associated with VCFM. In the fall of 2019, a multidisciplinary CPM committee consisting of attendings, residents, clinical pharmacists, social workers, and behavioral health specialists reviewed and modified the residency’s CPM protocols to ensure they aligned with the Centers for Disease Control and Prevention’s (CDC’s) 2016 Guidelines for Prescribing Opioids for Chronic Pain. 11 A series of five lectures on CPM and OUD by an addiction specialist and members of the CPM committee were held during the residency’s didactic sessions between December 19, 2019 and February 25, 2020, including the in-class portion of a hybrid MAT training and education on the new protocols and standardized documentation. The KUSM-W Institutional Review Board approved the study protocol for quality improvement.
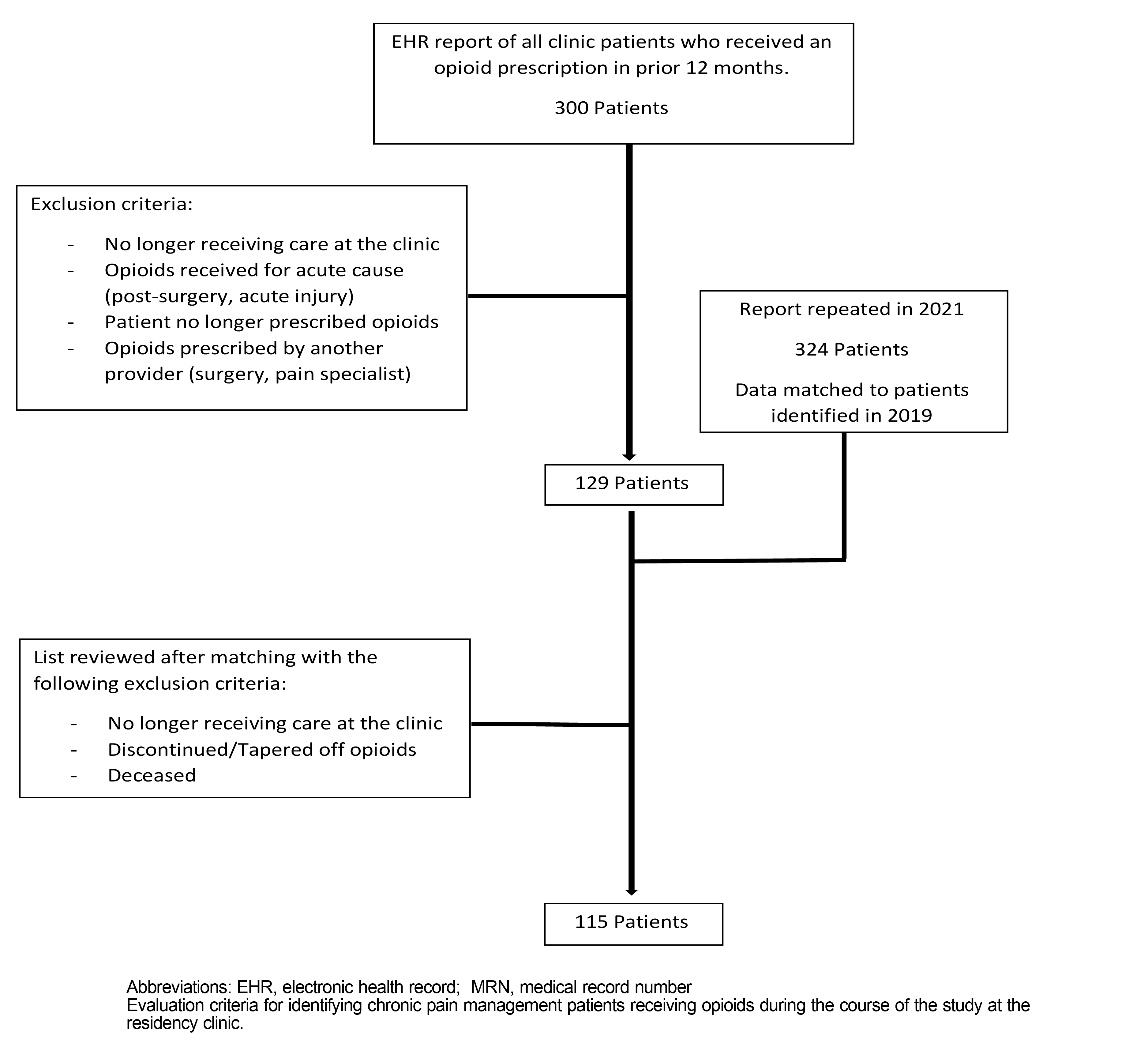
Participants completed two online assessment surveys at baseline and after completion of the lecture series utilizing a 5-point Likert Scale to evaluate comfort (1=very uncomfortable; 5=very comfortable) and knowledge (1=strongly disagree; 5=strongly agree) on OUD and MAT. The measures were developed using a multistage process, including expert review and cognitive interviews. In addition, a report through the electronic health record (EHR) was created identifying 300 clinic patients who had received an opioid prescription from the clinic in the past year. The list was reviewed and patients not receiving CPM were excluded, leaving 129 patients (Figure 1). We used a HIPAA-compliant G-Suite drive to create standardized spreadsheets for each chronic pain patient to monitor adherence and follow-up. Following intervention, the EHR report was regenerated, and patients were matched based on medical record number (MRN). After excluding patients who no longer received care at the clinic or no longer received opiates, 115 patients remained for final analysis.
We used standard descriptive statistics, paired sample t test, and percentage effective (z test), to estimate the effect of the CPM program on the outcome variables. All analyses were 2-sided with an α of 0.05.
Participant Characteristics
All 64 participants completed the baseline survey and 59 (92.2%) provided data in the postintervention survey. Table 1 presents the demographic profile of participants at baseline.
|
Characteristics
|
All Participants, n (%)
|
|
Biological Sex at Birth
|
|
|
Male
|
28 (43.8)
|
|
Female
|
36 (56.3)
|
|
Career Status
|
|
|
Faculty physicians
|
18 (28.1)
|
|
Resident physicians
|
46 (71.9)
|
|
First-year residents
|
16 (34.8)
|
|
Second-year residents
|
16 (34.8)
|
|
Third-year residents
|
14 (30.4)
|
Comfort
As Table 2 shows, the participants’ comfort scores of each scale item on postdidactic surveys significantly increased from baseline. In addition, the participants reported an overall significant improvement in their ability to comfortably assess and manage patients using controlled substances for chronic noncancer pain postdidactic, mean difference (MD, 2.5; 95% CI, 1.11-3.87; t[52]=3.61, P<.001).
|
Questions b
|
Time Point a
|
Mean Difference (95% CI)
|
t
|
P Value
|
|
Baseline (N=64)
|
Postdidactic (N=59)
|
|
1. How comfortable are you seeing patients who use controlled substances for nonmalignant pains?
|
3.1 (1.0)
|
3.6 (0.9)
|
0.5 (0.13 to 0.89)
|
2.68
|
.010
|
|
2. How comfortable are you prescribing a long-acting narcotic medication for chronic use?
|
2.6 (1.2)
|
3.1 (1.0)
|
0.5 (0.04 to 0.92)
|
2.18
|
.034
|
|
3. How comfortable are you recommending taper of opioids to chronic pain patients?
|
3.3 (1.2)
|
3.8 (1.0)
|
0.5 (0.05 to 0.89)
|
2.25
|
.029
|
|
4. How comfortable are you offering alternative medication and therapy for chronic pain patients?
|
3.8 (1.0)
|
4.3 (0.6)
|
0.4 (0.07 to 0.71)
|
2.47
|
.017
|
|
5. How comfortable do you feel screening patients for opioid use disorder?
|
2.9 (0.9)
|
3.5 (1.0)
|
0.6 (0.22 to 1.00)
|
3.12
|
.003
|
|
Overall level of comfort (5-25)
|
15.5 (3.7)
|
18.0 (3.3)
|
2.5 (1.11 to 3.87)
|
3.61
|
.001
|
Participants noted improved understanding of both the basic principles and indications for MAT (Table 3). The participants reported overall significant improvement in their perception of using MAT to treat OUD after the program (MD, 2.5; 95% CI, 10.89-2.83; t[43]=3.88, P<.001).
|
Statements b
|
Time Point a
|
Mean Difference (95% CI)
|
t
|
P Value
|
|
Baseline (N=64)
|
Postdidactic (N=59)
|
|
I have a basic understanding of the principles for MAT therapy
|
3.2 (1.2)
|
4.0 (0.8)
|
0.8 (0.26 to 1.21)
|
3.29
|
.002
|
|
I have a basic understanding of the indications for MAT therapy
|
3.0 (1.2)
|
4.0 (0.9)
|
1.0 (0.53 to 1.4)
|
4.36
|
<.0001
|
|
I am concerned that prescribing MAT will negatively affect our clinic (reversed scored ).
|
2.1 (1.1)
|
2.2 (1.0)
|
0.02 (-0.37 to 0.42)
|
0.12
|
.908
|
|
Our clinic would benefit from the opportunity to prescribe MAT
|
3.9 (1.0)
|
4.0 (0.9)
|
0.1 (-0.22 to 0.45)
|
0.68
|
.499
|
|
Overall perception of MAT (4-20)
|
12.3 (2.7)
|
14.1 (1.8)
|
1.9 (0.89 to 2.83)
|
3.88
|
<.0001
|
Clinical Measures
Physicians reported significant improvement in compliance regarding completing a medication agreement between the patient and provider (z=10.01, P<.001) and obtaining urine drug screens (z=3.73, P<.001, two tailed) after the didactic programs (Table 4).
|
Measure
|
Time Point
|
Percentage Effect (95% CI)
|
Z Test
|
P Value
|
|
Baseline (2019)
|
Postdidactics (2021)
|
|
Contract Obtained?
|
|
|
|
|
|
|
|
Yes
|
32
|
95
|
|
|
|
|
|
No
|
83
|
20
|
|
|
|
|
|
Total
|
115
|
115
|
|
|
|
|
|
Compliance
|
27.80%
|
82.60%
|
54.8% (44.1% to 65.5%)
|
10.01
|
<.001
|
|
UDS Obtained?
|
|
|
|
|
|
|
|
Yes
|
81
|
103
|
|
|
|
|
|
No
|
34
|
12
|
|
|
|
|
|
Total
|
115
|
115
|
|
|
|
|
|
Compliance
|
70.40%
|
89.60%
|
19.2% (9.1% to 29.2%)
|
3.73
|
<.001
|
The results of our interventions indicated that standardizing training and protocols within a residency clinic can improve compliance with the CDC guidelines as well as provider comfort in CPM and OUD. Providers reported increased comfort following the intervention period, and there was significant increase in compliance with our clinic policy based on the measures utilized in the study.
A strength of the study was the robust response within the residency, with over 60 providers, both residents and faculty participating. Also, we were able to evaluate both subjective data through the survey and objective data by reviewing patient compliance with the new clinic policies. A weakness of the study is there was no control group to compare the intervention to the general changes in knowledge and comfort that come with standard residency education. While the significant improvement in objective measures would indicate a system change, the subjective measures only evaluated comfort. Therefore, it is difficult to determine if individual prescriber habits were changed and limits the generalizability of the results.
In conclusion, as OUD becomes more recognized, it is imperative that family medicine residents acquire tools to treat this disorder. Our interventions have improved clinician comfort, compliance, and education to help combat the opioid epidemic in the United States.
Next Steps
The residency began screening for OUD in February 2020. However, the COVID-19 pandemic interrupted many services and project implementations, including the MAT clinic. Accordingly, the number of patients receiving MAT from the residency providers has been minimal to date. The residency is working to identify patients with OUD in our own clinic as well as partnering with local addiction programs to identify patients on MAT without a PCP.
Acknowledgments
Presentations: The findings from this study were presented in July 2019 at the American Academy of Family Physicians: Family Medicine Leads Emerging Leaders Institute.
References
-
Edlund MJ, Martin BC, Russo JE, DeVries A, Braden JB, Sullivan MD. The role of opioid prescription in incident opioid abuse and dependence among individuals with chronic noncancer pain: the role of opioid prescription.
Clin J Pain. 2014;30(7):557-564.
doi:10.1097/AJP.0000000000000021
-
Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM. Prescription Opioid Use, Misuse, and Use Disorders in U.S. Adults: 2015 National Survey on Drug Use and Health.
Ann Intern Med. 2017;167(5):293-301.
doi:10.7326/M17-0865
-
Hedegaard H, Miniño AM, Warner M. Drug Overdose Deaths in the United States, 1999-2018. NCHS Data Brief. 2020;356(356):1-8.
-
Substance Abuse and Mental Health Services Administration (US); Office of the Surgeon General (US). Facing Addiction in America: The Surgeon General's Report on Alcohol, Drugs, and Health. Washington (DC): US Department of Health and Human Services; November 2016.
-
Levy B, Paulozzi L, Mack KA, Jones CM. Trends in Opioid Analgesic-Prescribing Rates by Specialty, U.S., 2007-2012.
Am J Prev Med. 2015;49(3):409-413.
doi:10.1016/j.amepre.2015.02.020
-
Upshur CC, Luckmann RS, Savageau JA. Primary care provider concerns about management of chronic pain in community clinic populations.
J Gen Intern Med. 2006;21(6):652-655.
doi:10.1111/j.1525-1497.2006.00412.x
-
Tong ST, Hochheimer CJ, Peterson LE, Krist AH. Buprenorphine provision by early career family physicians.
Ann Fam Med. 2018;16(5):443-446.
doi:10.1370/afm.2261
-
Tesema L, Marshall J, Hathaway R, et al. Training in office-based opioid treatment with buprenorphine in US residency programs: A national survey of residency program directors.
Subst Abus. 2018;39(4):434-440.
doi:10.1080/08897077.2018.1449047
-
Tiemstra JD, Walsh LH. Integrating Buprenorphine Treatment Into Family Medicine Resident Clinic.
Fam Med. 2020;52(9):653-655.
doi:10.22454/FamMed.2020.783547
-
Kunins HV, Sohler NL, Giovanniello A, Thompson D, Cunningham CO. A buprenorphine education and training program for primary care residents: implementation and evaluation.
Subst Abus. 2013;34(3):242-247.
doi:10.1080/08897077.2012.752777
-
Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain - United States, 2016.
MMWR Recomm Rep. 2016;65(1):1-49.
doi:10.15585/mmwr.rr6501e1



There are no comments for this article.