Background and Objectives: The family medicine residency application process is arduous and competitive. An important part of the application is the in-person interview process, which was affected during the last two interview cycles (2021-2022) due to restrictions imposed by the COVID-19 pandemic. Virtual interviews eliminate traveling costs associated with applications, potentially improving underrepresented minorities’ access to interviewing opportunities. Our goal was to assess if virtual interviews at our institution have negative or positive effects on access for underrepresented in medicine (URiM) applicants and our residency match results.
Methods: We analyzed data from 2019-2022 to compare application volumes, applicant demographics, and match results between two in-person cycles (2019 and 2020) and two virtual cycles (2021-2022). Data were analyzed using Pearson χ2 criteria and P=.05 defined significance. Differences between years for expected counts were determined using single sample χ2 tests.
Results: No statistical significance was noted on number of applications by URiM to our program despite decrease costs associated with virtual interview process. The number of URiM applicants matching to our program did not improve by simply implementing virtual interviews when compared to in-person interview seasons in the past.
Conclusions: Virtual interviews at our institution did not increase URiM applications to our program from substantial equivalent medical schools. Further research in this area from programs in other states may enhance our understanding of the impact of virtual interviews on URiM applications to residency and match results.
Applying to family medicine residency programs is an arduous and competitive process, with 7,425 applications for 4,916 available positions this past year. 1 An important component of this process is the in-person interview, which helped assess important qualities including communication and interpersonal skills. Recent application cycles were disrupted by the COVID-19 pandemic which impacted residency interview seasons with traveling bans, social distancing recommendations, and infection control practices. 2 The American Medical Association, Educational Commission for Foreign Medical Graduates, National Resident Matching Program, and most specialty organizations strongly encouraged virtual interviews. Based on risk assessment, the University of Texas Health San Antonio Family Medicine Residency Program decided on virtual interviewing for the past 2 years (2021-2022). Studies have shown the economic burden of interview season is a determining factor for many students who declined interviews, perhaps influenced by personal debt. 3-5 Virtual interviews eliminate traveling costs associated with applications. This potentially improves access to interviewing opportunities for those for whom costs are a barrier, including underrepresented minorities.
The Association of American Medical Colleges defines underrepresented in medicine (URiM) as racial and ethnic populations underrepresented in the medical profession relative to their number in general population. URiM includes Black, Mexican-American, Native American (American Indian, Alaska Native, Native Hawaiian), and mainland Puerto Rican people groups. 6 US populations are becoming increasingly diverse and there is evidence that more diverse physician workforces positively impact patient care by improving communication and health care use, lowering health care costs, and improving patient satisfaction and compliance. 7, 8
Our goal was to assess whether virtual interviews at our institution have negative or positive effects on access for URiM applicants and our residency match results.
Our urban program is located in San Antonio, Texas and is Accreditation Council for Graduate Medical Education- (ACGME) approved for 45 positions; 42 of those positions are funded. We analyzed data from four previous application cycles (2109-2022) to compare application volumes, applicant demographics, and match results between two in-person cycles and two virtual cycles. We had confidence in our existing interview process and incorporated most of its attributes into our virtual approach, therefore the structure of our interview seasons remained consistent throughout. Applicants were evaluated on overall academic performance, compatibility with program, communication skills, and commitment to family medicine. Team members scored each candidate on these factors that provide quantitative data to help create our rank-order list throughout interview seasons.
Institutional review board exemption was granted and data were collected from applications submitted to our residency program through Electronic Residency Application Service platform, including self-reported demographic information. An important part of our review process and analysis focuses on evaluation of applicants from schools that, according to Texas Medical Board, have demonstrated substantial equivalence of their medical education. 9 Students from schools that have not demonstrated equivalence are likely to have difficulty obtaining a Texas medical license after graduation and programs may have difficulty obtaining state funding throughout their training years. 6 We analyzed data using Pearson χ2 criteria and P=.05 defined significance. Differences between years for expected counts were determined using single sample χ2 tests. We used SPSS v28 software for all analyzes (STATA Corp, College Station, TX).
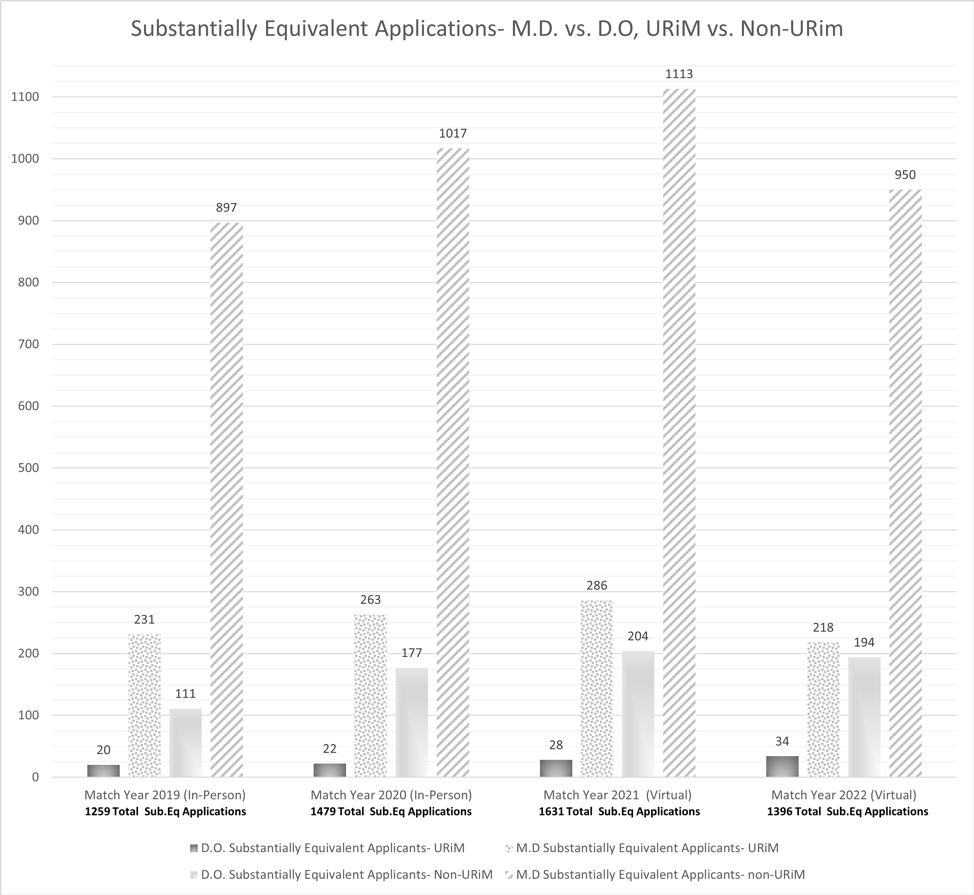
There was no difference in applications from substantially equivalent medical schools between in-person and virtual interview seasons. There was a slight increase in applications from URiM applicants during the virtual interview seasons but this was not statistically significant (Figure 1).
The number of invited URiM applicants remained stable throughout the interview seasons and the slight differences between in-person and virtual interview years were not statistically significant (single sample χ2 P=.66; Figure 2).
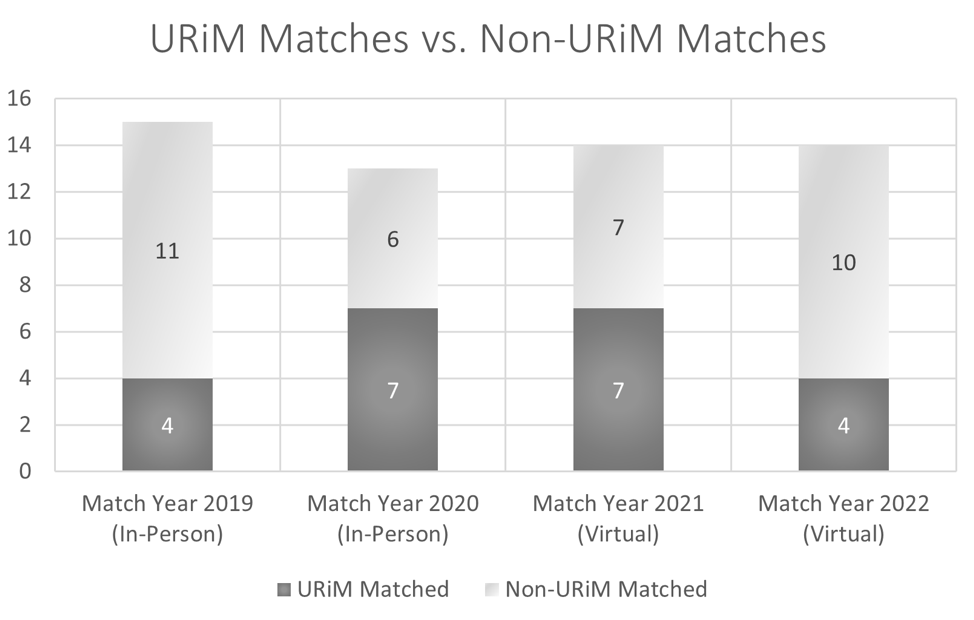
No significant difference was noted in the number of matched URiM applicants over the 4 years of data that were analyzed (P=.49; Figure 3).
Table 1 shows self-reported demographics of resident physicians matched to our program during the last four match cycles (2019-2022).
|
ERAS Self-identification- Match Year 2019 In-Person
|
Total Residents
|
AAMC URiM
|
|
White
|
4
|
N
|
|
Asian - Korean
|
3
|
N
|
|
Hispanic, Latino, or of Spanish origin - Cuban
|
2
|
N
|
|
Hispanic, Latino, or of Spanish origin - Mexican/Chicano
|
2
|
Y
|
|
Asian - Chinese
|
1
|
N
|
|
Asian - Vietnamese
|
1
|
N
|
|
Black or African American
|
1
|
Y
|
|
Hispanic, Latino, or of Spanish origin - Puerto Rican
|
1
|
Y
|
|
Self-identified on ERAS- Match Year 2020 In-Person
|
|
AAMC URiM
|
|
Hispanic, Latino, or of Spanish origin - Mexican/Chicano
|
6
|
Y
|
|
White
|
3
|
N
|
|
Hispanic, Latino, or of Spanish origin - Dominican
|
2
|
N
|
|
Hispanic, Latino, or of Spanish origin - Puerto Rican
|
1
|
Y
|
|
Other: Assyrian
|
1
|
N
|
|
Self-identified on ERAS- Match Year 2021 Virtual
|
|
AAMC URiM
|
|
Hispanic, Latino, or of Spanish origin - Mexican/Chicano
|
4
|
Y
|
|
White
|
2
|
N
|
|
Asian - Filipino
|
1
|
N
|
|
Asian - Indian
|
1
|
N
|
|
Black or African American - African American
|
1
|
Y
|
|
Black or African American - Afro-Caribbean
|
1
|
Y
|
|
Hispanic, Latino, or of Spanish origin - Colombian
|
1
|
N
|
|
Hispanic, Latino, or of Spanish origin - Puerto Rican
|
1
|
Y
|
|
Not Specified
|
1
|
N
|
|
Other: Middle Eastern
|
1
|
N
|
|
Self-identified on ERAS- Match Year 2022 Virtual
|
|
AAMC URiM
|
|
White
|
3
|
N
|
|
Asian - Filipino
|
2
|
N
|
|
Hispanic, Latino, or of Spanish origin - Colombian
|
2
|
N
|
|
Hispanic, Latino, or of Spanish origin - Mexican/Chicano
|
2
|
Y
|
|
American Indian or Alaskan Native: Tribal Affiliation: Cherokee
|
1
|
Y
|
|
Asian - Indian
|
1
|
N
|
|
Asian - Korean
|
1
|
N
|
|
Asian - Vietnamese
|
1
|
N
|
|
Black or African American - African American
|
1
|
Y
|
There was an increase in total number of applications received during first virtual season possibly driven by accessibility of virtual platforms as well as ACGME Single Accreditation System (SAS) efforts which integrated all osteopathic graduate medical education under ACGME. 10, 11 There was no statistically significant difference in number of substantially equivalent applications, URiM applications, or increase in number of URiM applicants matching to our program with virtual compared to in-person interviews.
DO applications to our residency program have increased over the years as expected with the implementation of SAS but the number of DO URiM applications has been small.
Our residency program URiM numbers are significantly higher than other residencies, currently 22 URiM resident physicians out of 45 positions. Mexican Americans are better represented in our residency, as reflective of the population of San Antonio, Texas and of the patients we serve. Virtual interviews did not increase URiM substantially equivalent applications to our program. If more opportunities for URiM are desired other efforts should be implemented as virtual platforms alone did not enhance our experience. Further research in this area from programs in other states may enhance our understanding of the impact virtual interviews have on URiM applications to residency and match results. Our URiM statistics may be an index of potential diversity in our residency program, however our match results highlight cultural and ethnic differences among our resident physicians that contribute to our program’s diversity and strengthen our training program as a whole but are not recognized by the URiM designation (Table 1).
We recognize that efforts to improve URiM diversity in GME are not achieved when simple metrics are met. Instead, improving diversity requires constant reinvestment into minority communities and their applicants.
References
-
-
-
Fogel HA, Liskutin TE, Wu K, Nystrom L, Martin B, Schiff A. The Economic Burden of Residency Interviews on Applicants. Iowa Orthop J. 2018;38:9-15.
-
Pourmand A, Lee H, Fair M, Maloney K, Caggiula A. Feasibility and Usability of Tele-interview for Medical Residency Interview.
West J Emerg Med. 2018;19(1):80-86.
doi:10.5811/westjem.2017.11.35167
-
Ojo E, Hairston D. Recruiting underrepresented minority students into psychiatry residency: a virtual diversity initiative.
Acad Psychiatry. 2021;45(4):440-444.
doi:10.1007/s40596-021-01447-6
-
Page KR, Castillo-Page L, Poll-Hunter N, Garrison G, Wright SM. Assessing the evolving definition of underrepresented minority and its application in academic medicine.
Acad Med. 2013;88(1):67-72.
doi:10.1097/ACM.0b013e318276466c
-
Silver JK, Bean AC, Slocum C, et al. Physician Workforce Disparities and Patient Care: A Narrative Review.
Health Equity. 2019;3(1):360-377. Published 2019 Jul 1.
doi:10.1089/heq.2019.0040
-
-
-
Fugazzi L, Cummings M. The AOA/ACGME Single Accreditation System and Its Immediate and Future Impact on Family Medicine.
Fam Med. 2022;54(2):91-96.
doi:10.22454/FamMed.2022.266260
-



There are no comments for this article.