Background and Objectives: Competency based medical education (CBME) aims to produce graduates prepared for independent practice. Many equate the outcome of “preparedness for practice” with acquisition of competence. As educators evaluate the outcomes of CBME, being clear on the concept of preparedness for practice will clarify the results that are measured and assessed. This study examined how preparedness for practice is conceptualized in the literature and by family physicians (FPs) in Canada.
Methods: This multimethod qualitative descriptive study included (1) rapid review and narrative synthesis, and (2) focus groups with early-career FPs using maximum variation sampling until thematic saturation was reached. Focus groups explored the FPs’ conceptualizations of preparedness for practice. Focus groups were audio-recorded, transcribed, and coded before content analysis.
Results: Thirty-four articles met the inclusion criteria, and 59 early-career FPs participated in the focus groups. We found no consensus on the conceptualization of preparedness for practice in the literature; however, the concept often was described as acquiring competencies for program requirements. In the literature and focus groups, we identified four themes for the conceptualization of preparedness for practice. These themes included competence, self-confidence (self-efficacy, self-concept), capability, and adaptability.
Conclusions: Preparedness for practice involves an interplay of dynamic and complex constructs from competence, self-confidence, capability, and adaptability. Preparedness is more than possessing several competencies; it calls for integrating and applying competencies in complex and changing environments. This study aimed to start a discussion on what end point is desirable for residency education and proposed that the end point needs to move beyond competencies.
The overarching goal of medical education programs is to prepare the physician workforce to provide the highest quality of care and meet the needs of patients and populations. 1-5 However, preparing medical graduates for practice is challenging because the health care needs of modern society are changing; consequently, what graduates need to know in preparation for practice is continually evolving. 2
Residency programs worldwide have been changing to better prepare physicians for independent practice. Accrediting bodies have enhanced residency training by adopting competency-based medical education (CBME). 4, 6 CBME is an approach to preparing physicians for a practice oriented around competencies based on societal and patient needs. 6 In CBME, clearly defined outcomes are paramount 1; however, tactics to achieve outcomes vary. Proponents of CBME suggest that it fosters individualized learning through feedback and observation, self-reflection, and accountability. 4 Critics have raised some concerns 7-9 about whether this approach produces better physicians since it is based on deeply held assumptions that CBME is about competence. 10 Thus, the approach may be too focused on achieving a checklist of competencies related to the skills and knowledge aspects of medical education, focusing less on the graduate’s self-confidence, capability, and adaptability. 11
In Canada, most family physicians (FPs) are trained within the accredited 2-year family medicine (FM) residency programs affiliated with one of the 17 medical schools. 6 Third-year residency programs are available in various areas of practice. 12 Currently, Canada has the shortest length of FM training worldwide. 13
In 2010, the College of Family Physicians of Canada introduced the Triple C Competency-based Curriculum as a guide to support programs to train FPs to be “competent to enter and adapt to the independent practice of comprehensive FM anywhere in Canada.” 6, 14, 15 Comprehensive care refers to care provided to a patient population across the life span, addressing a multitude of health problems in various clinical settings. 16 The curriculum is based on assumptions that achieving competence at the end of training is equivalent to being prepared for practice. However, despite the implementation of this curriculum, medical graduates report not feeling prepared for practice even though they are considered competent based on their certification and licensing examinations. 17 The lack of perceived preparedness has been associated with nonrural training programs and practicing in rural locations. 18 Preparedness for practice is one potential factor amongst others that may explain declining trends in scope of practice in Canada. 19, 20
FPs’ lack of perceived preparedness for practice suggests a misalignment between what FM programs teach students and what learners need to be prepared for practice. Thus, an understanding of how preparedness for practice is conceptualized is needed. 21, 22 This understanding will help inform the educational strategies that should be implemented and the outcomes that should be measured and assessed at the end of FM training. To our knowledge, no studies have examined the conceptualization of preparedness for practice in family medicine. This study aimed to understand how preparedness for practice is conceptualized and operationalized in the literature and by early-career FPs in Canada.
Study Design
We conducted a multimethod qualitative study to understand new physicians’ conceptualization and operationalization of preparedness for practice. The focus group study was part of a larger multimethod study (survey and focus groups) examining the experiences of early-career FPs. The study was situated within an interpretive research paradigm that aimed to understand lived experience (ie, preparedness for practice) based on participants’ interpretations, perceptions, and experiences. 23 Data collection for the study took place in two stages. First, we conducted a rapid review to explore the concept of preparedness for practice. Second, we conducted focus groups with Canadian FPs to understand how they conceptualized and operationalized being prepared for practice. We defined early-career FPs as physicians that completed the residency training program and were 2 to 5 years in independent practice in Canada. We used the Consolidated Criteria for Reporting Qualitative Studies (COREQ) guidelines for this study. 24 The study received ethics approval from the University of Toronto under protocol number #39077.
Sampling and Data Collection
Rapid Review. We conducted a scoping rapid review to systematically search, select, and synthesize knowledge on preparedness for practice, 25 including selective searching. 26 Rapid reviews conducted in medicine 2 are considered suitable methodology for generating timely results to inform decision-makers. 27 The search strategy for the study was guided in consultation with a medical information specialist (Supplementary Material 1). Our search took place in Medline and Embase because these include a large inventory of publications related to the field of medicine. We also searched various relevant national and international websites (eg, Royal Colleges of Medicine) representing the gray literature.
The criteria for literature inclusion focused on the preparedness of trainees and graduates across medical specialties, availability in full text and English, and publication between January 2004 and February 2020 (the period recommended by the medical information specialist). Although this study focused on the preparedness of early-career FPs, we also included studies from other specialties because we wanted a thorough understanding of how preparedness for practice is understood in the literature. We excluded studies if they were seminar papers, letters to the editor, focused on the transition from postgraduate training to independent practice, study protocols, articles in the press, articles not available in full text, and articles with insufficient information to chart the data.
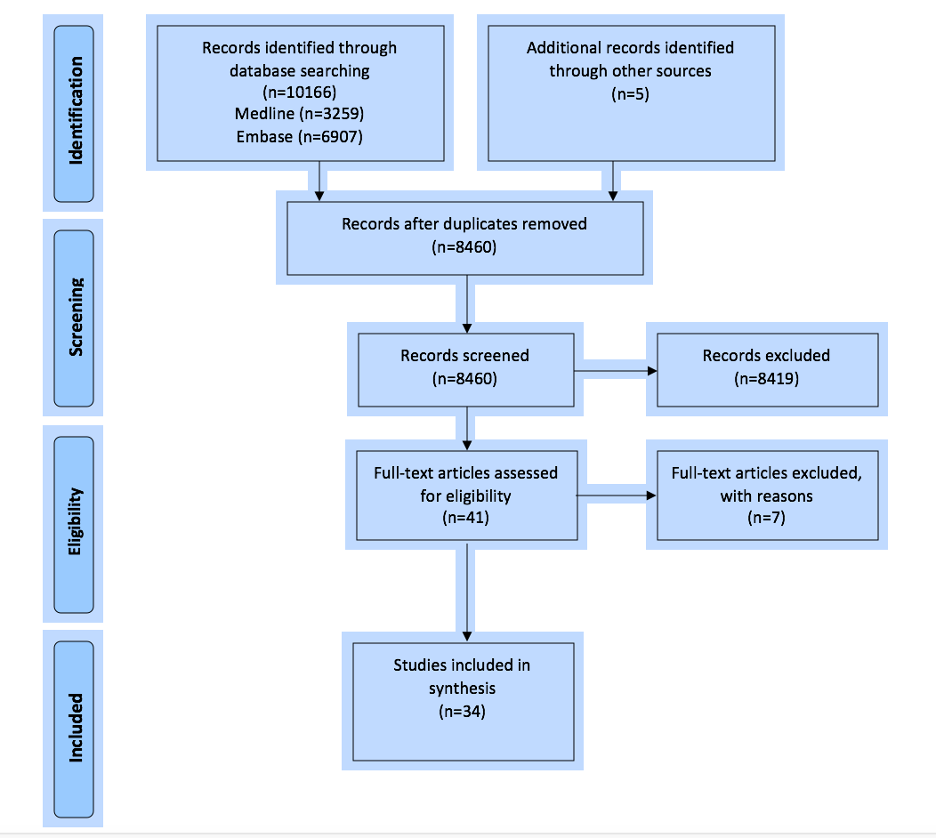
The search strategy yielded 10,166 records from two databases and five records from the gray literature. After the screening process, 41 full-text articles based on the exclusion and inclusion criteria were reviewed independently by two reviewers (A.G., M.A.; Figure 1). Seven articles were excluded from the review due to missing information. In total, 34 papers met the inclusion criteria for the final thematic analysis. From the included studies, two reviewers (M.A. and R.A.) independently extracted data on their objectives, settings, populations, study design, results, definition of preparedness, and components, including measurement outcomes. We resolved disagreements through discussions in meetings.
Focus Groups. We report on the qualitative focus group data collected through a larger mixed-methods study examining the preparedness of practice of early-career FPs and the factors contributing to practice choices in Canada.
To maximize the representativeness of all early-career FPs in Canada, we conducted 12 virtual focus groups: one in each of five provinces (Alberta, British Columbia, Manitoba, Newfoundland and Labrador, and Saskatchewan); one combined focus group representing New Brunswick, Prince Edward Island, and Nova Scotia due to smaller geographies; and two in each of the Territories, Ontario, and Quebec. The criteria for this study included being an early-career FP, having completed residency training in Canada, and practicing for 2 to 5 years since graduation. Maximum variation sampling 28 guided our selection of participants to obtain diversity in age, gender, years in training, university of training, practice location, type of services provided in practice, and involvement in different practice models (eg, interprofessional teams and academic activities).
We recruited early-career FPs through multiple recruitment methods: email, posts to virtual notice boards and social media, and snowball sampling. We invited 160 early-career FPs. In total, 59 FPs participated in the focus groups with a heterogeneous group of 6 to 8 participants per provincial/territorial focus group by age, practice location, type, and gender. We provided participants with study information and an honorarium ($50 gift card). We conducted the focus groups using a web-based videoconference platform and a semistructured guide (Supplemental Material 2). Two qualitative researchers, the principal investigator (M.A.) and a research assistant (R.A.), conducted the focus groups. The interview questions explored the perceptions of participants concerning the definition of preparedness for practice, areas of preparedness, and factors that shape preparedness and practice choices. Focus groups lasted approximately 90 to 110 minutes (mean, 95). The facilitators had no prior relationship with the participants. The facilitators took notes and met after each focus group to debrief. Focus groups were recorded, transcribed verbatim, and securely deleted once transcripts were coded.
Data Analysis
Rapid Review
For the rapid review, we used thematic analysis and narrative synthesis to identify prominent themes in the literature. 29 Members of the research team agreed on the themes and discussed discrepancies until a consensus was reached.
Focus Groups
We used qualitative content analysis to analyze the data from the focus groups. 30 Our content analysis followed a four-step process described by Krippendorff. 31 Guided by the results of the rapid review, we began our analysis of the focus groups’ data using a directed content analysis with the major categories previously identified. 32, 33 Two researchers (M.A. and R.A.) coded the transcripts. The coding schema was augmented with the iterative addition of codes as they arose from a series of discussions in team meetings, and the codes were then grouped into categories. 33 In focus groups where participants shared written comments within the chatbox, the data were analyzed using the same methodology as the transcripts. We used NVivo version 12 (Lumivero) software to code and organize the data. 34 Both R.A. and M.A. met several times to resolve discrepancies and reach consensus on themes and subthemes. Alternative understandings of the data were also discussed. We documented emerging interpretations of the data to help add transparency to the data analysis process. 35 We also shared a summary of the findings with a few early-career FPs to validate study results. Two participants provided feedback and indicated that they agreed with the findings.
Thirty-four papers met our inclusion criteria and were included in our thematic analysis. Table 1 displays the characteristics of the included studies. Data extraction tables of documents are available in Supplementary Material 3. The focus groups consisted of a diverse sample of FPs (Table 2).
|
Study purpose
|
Number of
studies
|
Citations
|
|
Examined preparedness to practice
|
23
|
2, 35-37, 41-46, 48, 52-59, 61, 62, 64,67
|
|
Described the influence of factors, culture, context, or training program on preparedness
|
8
|
38, 47, 49-51, 60, 63, 65
|
|
Described a new medical curriculum
|
1
|
40
|
|
Involved the development of an inventory of tasks
|
1
|
34
|
|
Aimed at defining preparedness
|
1
|
39
|
|
Country
|
|
|
|
United Kingdom
|
13
|
2, 35, 37-39, 42, 43, 45, 53, 55, 61-63
|
|
Netherlands
|
7
|
35, 47, 49, 50, 57, 64, 65
|
|
United States
|
4
|
46, 52, 56, 58
|
|
Canada
|
4
|
41, 48, 51, 54
|
|
Australia
|
3
|
40, 59, 67
|
|
Switzerland
|
1
|
44
|
|
Sweden
|
1
|
36
|
|
Pakistan
|
1
|
60
|
|
Study
population
|
|
|
|
Medical graduates
|
13
|
2, 36, 38, 45, 53, 55, 56, 59, 60-62, 65,67
|
|
Specialty physicians
|
14
|
34, 35, 37, 41, 43,47-50, 54, 57, 58, 63, 64
|
|
Family physicians
|
5
|
39, 44, 46, 51, 52
|
|
Stakeholders
|
1
|
42
|
|
No study population
|
1
|
40
|
|
Method
|
|
|
|
Quantitative methods (cross-sectional surveys)
|
21
|
35, 37, 38, 41, 45-47, 49-57, 59, 60, 62, 65, 67
|
|
Qualitative methods
|
6
|
39, 42, 44, 48, 61, 64
|
|
Mixed methods
|
5
|
34, 36, 43, 58, 63
|
|
Review article
|
2
|
2, 40
|
|
|
|
AB
|
BC
|
MB
|
Maritimes
|
NL
|
ON
|
QC
|
SK
|
Territories
|
|
Number of participants
|
|
10
|
9
|
7
|
6
|
8
|
13
|
8
|
7
|
7
|
|
Age in years (mean)
|
|
33.2
|
34.7
|
33.4
|
37.8
|
33.8
|
34.2
|
32.1
|
33.1
|
35.0
|
|
Gender
|
Female
Male
Prefer not to answer
|
6
4
—
|
8
1
—
|
3
3
1
|
6
—
—
|
7
1
—
|
6
7
—
|
6
2
—
|
4
3
—
|
6
1
—
|
|
Years in practice
|
2
3
4
5
Missing
|
—
10
—
—
—
|
2
6
1
—
—
|
1
4
2
—
—
|
—
4
1
1
—
|
3
2
1
2
—
|
—
10
3
—
—
|
1
4
3
—
—
|
—
1
3
2
1
|
—
4
1
2
—
|
|
Residency training location
|
University of BC
University of Calgary
University of Alberta
University of SK
University of MB
University of WO
McMaster University
University of Toronto
NOSM
University of Ottawa
Queen’s University
Université de Sherbrooke
Université de Montréal
McGill University
Université Laval
Dalhousie University
Memorial University
Outside Canada
|
—
4
6
—
—
—
—
—
—
—
—
—
—
—
—
—
—
—
|
5
—
—
—
—
—
—
—
—
—
1
—
—
—
—
—
3
—
|
—
—
—
—
6
—
—
—
—
1
—
—
—
—
—
—
—
—
|
—
—
—
—
1
—
—
—
—
—
—
—
—
—
—
4
1
—
|
—
—
—
—
—
—
1
—
—
—
—
—
—
—
—
—
7
—
|
—
1
—
—
—
2
1
5
2
—
1
—
—
—
—
—
—
—
|
—
—
—
—
—
—
—
—
—
1
—
2
1
3
—
—
—
1
|
1
—
—
6
—
—
—
—
—
—
—
—
—
—
—
—
—
—
|
1
1
—
1
—
—
—
4
—
—
—
—
—
—
—
—
—
—
|
|
Practice location
|
Inner city
Urban/suburban
Small town
Rural
Remote/isolated
Mixture of environments
|
—
4
2
2
—
2
|
1
6
—
—
—
2
|
1
2
—
1
—
3
|
1
2
2
—
—
1
|
—
2
—
4
—
2
|
1
4
1
3
1
3
|
—
4
2
—
—
2
|
—
3
1
1
—
2
|
—
1
—
—
2
4
|
|
Practice model
|
Solo practice
Group physician practice
Interprofessional team-based practice
Mixed practice
Other
|
—
7
—
1
2
|
—
6
2
1
—
|
—
—
3
3
1
|
1
—
4
1
—
|
2
4
2
—
—
|
—
4
7
—
2
|
—
5
2
—
1
|
—
2
4
—
1
|
—
3
3
—
1
|
|
Practice type
|
Comprehensive in one setting
Comprehensive in multiple settings
Comprehensive with a special interest
Focused
Other
|
1
7
—
1
1
|
2
3
4
—
—
|
—
5
—
1
1
|
1
3
—
1
1
|
—
4
1
—
3
|
4
6
1
1
1
|
4
1
2
1
—
|
—
3
1
1
2
|
—
5
1
1
—
|
|
Academic affiliation
|
Yes
No
|
8
2
|
6
3
|
6
1
|
4
2
|
5
3
|
9
4
|
7
1
|
7
—
|
6
1
|
Defining Preparedness
Rapid Review
Our results highlight a lack of conceptual clarity on the definition of preparedness for practice. While all articles used the term preparedness, 24 (70.5%) studies provided explicit or implicit definitions of preparedness for practice. Looking across studies, we found no consistency in the definition. An agreed-upon definition was absent even when comparing studies from the same jurisdiction.
In our thematic analysis of the literature, we found that preparedness for practice includes four conceptual dimensions: (a) competence, (b) self-confidence (including self-concept and self-efficacy), (c) capability, and (d) adaptability.
In the literature, competence was described as the learner’s possession of competencies expressed as observable abilities reflecting their knowledge, technical and clinical skills, values, and attitudes across specific domains and tasks. Competencies as elements of competence 36-42 were the most reported dimension in the studies (n=24/34, 70.5%). 2, 36-59 Table 3 lists the competencies cited.
|
Competencies
|
Number of studies, N=34,
n (%)
|
Citations
|
|
Clinical skills (ie, performing a laboratory test or imaging procedure)
|
24 (70.5)
|
2, 36-41, 43-59
|
|
Intrinsic competencies
|
18 (53)
|
2, 37-39, 41, 43-50, 52, 53, 59-67
|
|
Intrinsic competencies—collaboration
|
7 (18)
|
43, 47, 49, 50, 52, 59, 67
|
|
Communication
|
10 (29)
|
39, 41, 43-46, 49, 50, 52, 59
|
|
Leadership
|
2 (6)
|
50, 52
|
|
Mentorship
|
4 (12)
|
39, 45, 50, 52
|
|
Financial management
|
2 (6)
|
45, 58
|
|
Managerial
|
9 (26)
|
37, 39, 43, 45, 49, 52, 58-59, 67
|
|
Legal
|
3 (9)
|
44, 47, 58
|
|
Ethical management
|
4 (12)
|
44, 47, 48, 58
|
|
End of life
|
3 (9)
|
43, 48, 58
|
|
Rural practice
|
1 (3)
|
53
|
|
Research
|
7 (20.5)
|
39, 43, 44, 47, 49, 50, 59
|
|
Continuous professional development
|
6 (18)
|
38, 43, 47, 52, 59, 67
|
Confidence, with its related terms, was the second most cited dimension of preparedness in the literature. Self-confidence was identified in 10 studies (n=10/34, 29%), 37, 40, 41, 44, 46, 51, 54, 55, 59 referring to the feeling of having a required skill or knowledge. In the studies, self-confidence was used interchangeably with self-concept (n=1/34, 3%) 44 and self-efficacy (n=4/34, 12%). 40, 44, 51, 59
Adaptability, the third dimension of preparedness for practice, refers to an individual’s capacity to deal with and undertake actions in specific contexts that are new, changing, uncertain, or ambiguous. 41, 46, 60 Wiener-Ogilvie et al (2014) indicated that training in different contexts fosters adaptability by providing exposure to managerial approaches, clinical care approaches, and patient populations. 41
Capability, the fourth dimension, emerged in seven studies. 42, 52, 55, 59-62 Capabilities were used interchangeably with competencies in some studies. 62 Competence refers to delivering specific competencies in a relatively predictable context, and capability reflects the ability to take effective action in unfamiliar, complex, and changing circumstances. 56 Capability is a complex construct that includes the integration of competence, self-confidence in abilities to operate in unfamiliar situations, and willingness to engage in ongoing learning and problem-solving. 63
Most studies (n=17, 70.8%) examined preparedness for practice from a short-term perspective, immediately or soon after graduation. 2, 36-38, 40, 50, 51, 53, 54, 55, 57-59, 61, 64-66 Four studies focused on long-term preparedness and examined preparedness for physicians that had been practicing 5 to 10 years. 39, 45, 56, 59 Ten studies (29.4%) examined preparedness while transitioning into independent practice. 2, 40, 41, 46, 50, 52, 67, 66, 68, 69 One study focused on a surgeon’s preparedness for practice in a leadership role. 67 Another study viewed preparedness for practice specific to building physician identity 41 as an outcome.
Focus Groups
Participants talked explicitly about their conceptualization of preparedness for practice in response to questions or implicitly when sharing their experiences about their perceived preparedness and the factors contributing to preparedness. We found the conceptualization of preparedness for practice by early-career FPs to be consistent with the findings of the rapid review. We support our findings with illustrative quotes in Table 4.
|
Theme
|
Supporting quotes
|
|
Competence
|
“I would say either having the knowledge or the toolbox in which to find the knowledge for the daily activities you need to provide in your daily practice.” (Newfoundland FG)
“The first thing that comes to mind for me is like feeling well-equipped to provide the care that you need to the full spectrum of patients that might be presented to you in your particular practice and feeling competent in the skills that you have.” (Alberta FG)
“A lot of the time, when we prepare for practice, we think a lot about the medicine and the competence from like being a family medicine expert and like a physician expert. But also, what I find was the biggest gap that I was struggling with in my preparedness to practice was my ability to be the manager role, the administrative role.” (Ontario First FG)
|
|
Self-confidence
|
“When I started practice, like, that feeling of like confidence and being in control and supported, like it was difficult, in a rural setting.”
(Saskatchewan FG)
“I actually think it’s much more about your belief in yourself and your willingness to put yourself in an uncomfortable situation.” (Territories First FG)
“Having like confidence to be a staff practitioner. I won’t say that I felt like I had all of the confidence I needed to practice solo but certainly more confidence than I had as a resident.” (British Columbia FG)
“I think somewhere in the second year of residency, I got to a point with family medicine where I felt that way, that I was confident about what I’m doing and/or I knew where to look for the information that I needed if I didn’t feel confident about something.” (British Columbia FG)
|
|
Capability
|
“And so to have an approach to situations where you don’t know exactly what’s going on, to know the limits of your capabilities and know when to ask for help. Because sometimes you don’t have help, or you don’t have adequate help, right. Sometimes you call somebody and they’re not helpful.” (Ontario 2nd FG)
“[Capability is] to find the knowledge and the knowledge to know what [they] didn’t know and to know where to find the answers.” (Maritimes FG)
|
|
Adaptability
|
“I think that no matter how much we prepare or how much training we get in residency, what you encounter in your actual practice is going to be likely very different. . . . The ability to adapt to different changes and what your expectations are of your practice is something that I personally would have liked to be prepared for in training.” (Alberta FG)
“So I felt like there was a lot of my residency that prepared me to be a locum in particular because you’re constantly switching clinics, you’re switching gears, you’re switching focuses. And so there’s that confidence in me and the adaptability to approach, you know, the new learning challenges. And I think that’s especially key in family medicine. Again, as my colleagues are saying, you know, you may not know everything but you know where to find out or where to look.” (British Columbia FG)
“I mean there’s that issue of competence, confidence, your capacity, and your ability to be adaptable in early practice, in addition to your training component. So, I think it’s complicated.” (Ontario First FG)
“But it’s more so having the resilience to modify their practice and feel competent to doing that, and pivoting and just being adaptable. Resilient residents—like building that skill set as opposed to building every individual skill set that you mentioned—is a lot more valuable. It’s just harder to measure quantitatively or to integrate into your curriculum. So I think that’s where the disparity is. Everyone wants something different out of their residency program as a family medicine resident. So you’re not going to satisfy everyone, and you’re not going to make everyone feel prepared. But if you can make them feel confident and flexible and adaptable, that’s the end goal.” (Ontario First FG)
|
The degree to which the concepts for preparedness for practice were important, however, was variable among FPs. Competence and self-confidence were most frequently identified as key concepts of their preparedness. These were followed almost equally by the concepts of adaptability and capability.
Early-career FPs highlighted the importance of being competent in clinical and nonclinical areas. However, participants indicated that competence alone was insufficient for feeling prepared for practice and that confidence was equally important. This was particularly true in unfamiliar situations when critical decisions are made rapidly or in less resourceful environments. Some participants discussed self-concept and described it as confidence in oneself or their role as a practitioner. Others discussed the importance of self-efficacy, the confidence in their skills, knowledge, capabilities, and actions.
Participants indicated that adaptability was essential to the feeling of preparedness for practice because the training environment often differs from the practice environment, and FPs must have the skills to adapt to different settings, populations, and situations. Participants noted that the capability to continuously learn and “to find the knowledge and the knowledge to know what [they] didn’t know and to know where to find the answers” (Maritimes FG) was essential to preparedness for practice. FPs most frequently identified the importance of having problem-solving capabilities and being efficient and effective in practice. FPs highlighted that preparedness is a dynamic process that can grow or diminish over time. Preparedness increases with the support of colleagues in practice and decreases when physicians discontinue practicing in specific domains, resulting in the loss of skills. Respondents also suggested that preparedness for practice was a complex term and an interplay of all these concepts.
Our study explored how preparedness for practice is conceptualized and operationalized in the literature and by Canadian early-career FPs. While all studies used the term preparedness, we found no agreement on a definition for preparedness for practice. Four dynamic and complex constructs emerged to define preparedness for practice: competence, self-confidence, capability, and adaptability.
Competence and capability are terms sometimes used interchangeably in the literature71; however, our study highlighted distinct differences. Whereas competence is the possession of a set of correct-answer skills, knowledge, and the performance of specific tasks in relatively predictable circumstances, capability is the confidence that one can effectively use and develop their skills in complex and changing circumstances. 70, 71, 18 Capability is about responsiveness, creativity, contingent thinking and growth, and the ability to adapt to relatively uncertain situations. 71 Capable people develop their skills and knowledge long after leaving formal education. 72
Self-confidence is differentiated from competence because the former requires an internal assessment of self versus reliance on an external assessment. 40 Bandura distinguished self-confidence from self-efficacy according to the strength of the belief in one’s ability to obtain a desired outcome. 73 Self-confidence is linked to achievement. 73, 74 The extent learners believe that they are prepared to practice reflects their self-concept. Self-concept is related to professional identity formation, defined by Cruess et al as “a representation of self, achieved in stages over time during which the characteristics, values, and norms of the medical profession are internalized, resulting in an individual thinking, acting, and feeling like a physician.” 75 Given the diversity of practice contexts that graduates may enter, adaptability is an essential dimension of preparedness for FM.
This study shows that a fulsome definition of preparedness for practice extends beyond competence to embrace the concepts of self-confidence (self-concept, self-efficacy), capability, and adaptability. Preparedness for practice is a dynamic process in which learners must possess the competence and the ability to confidently apply these skills in familiar and uncertain situations, and engage in continuous self-reflection, learning, and problem-solving.
If the end point of medical training is to prepare graduates for practice, this study indicates that a multidimensional approach is needed. Key dimensions include graduates who are competent, capable, self-confident (with a sense of self-concept and self-efficacy), and able to adapt to changing contexts. This vision aligns with Scott’s professional capability framework, which identifies competencies and capabilities that enable professionals to adapt confidently to the many challenges of practice. 71 In the context of society’s changing and complex needs, our findings highlight the need to include these concepts in education strategies for teaching, learning, and assessment—during residency training and continuing with professional development opportunities. Future research should focus on developing a capability framework for FM, which can help inform educational strategies for curriculum development and assessment.
Limitations
Because preparedness for practice is not described consistently, some relevant research may be absent from this rapid review due to our selective searching. Our study’s intent was not to capture all articles but to provide an overview of the literature. Furthermore, the narrative review is primarily descriptive and does not examine how preparedness for practice is measured or assessed. The sample may overrepresent some characteristics of FPs (eg, gender, academic affiliation). In addition, the population of participants may vary among new FPs, resulting in self-selection bias. However, we are assured that the diversity among participants (eg, age, practice location, years in practice, practice type) and the large sample from across Canada make our results transferable to other contexts, such as outside of Canada, including rural towns. Lastly, we acknowledge that given the complexity of preparedness for practice, a singular definition of this concept may not be feasible. Instead, our study aimed to provide an initial understanding of potential constructs that can contribute to a universal understanding of this term.
If the main goal of residency training is to prepare graduates for independent practice, then knowing what preparedness means is critically important. Our study suggests a conceptualization of preparedness for practice that combines the constructs competence, self-confidence (self-efficacy, self-concept), capability, and adaptability. We propose that medical education recalibrates with an approach that ensures graduating physicians are competent, confident, capable, and adaptable to the challenges and dilemmas of professional practice that will emerge over the coming decades.
Funding for the study is from the College of Family Physicians of Canada. The grant name was Preparedness for Practice and Practice Choices: A Qualitative Study on the Perspectives of Early-Career.
Dr Ivy Oandasan (Director of Education) and Dr Nancy Fowler (Executive Director, Academic Family Medicine) are employed by the College of Family Physicians of Canada (CFPC). Dr Monica Aggarwal was partially compensated for her time on this project through the CFPC and the University of Toronto.
Acknowledgments
We acknowledge Ms Aasha Gnanalingam for research assistance with the rapid review and the College of Family Physicians of Canada for sponsoring this study. We also acknowledge Dr Brian Hutchison from McMaster University and Dr Maria Mylopoulos from the University of Toronto for feedback on this manuscript.
References
-
Holmboe ES, Sherbino J, Englander R, Snell L, Frank JR; ICBME Collaborators. A call to action: the controversy of and rationale for competency-based medical education.
Med Teach. 2017;39(6):574-581.
doi:10.1080/0142159X.2017.1315067
-
Monrouxe LV, Grundy L, Mann M, et al. How prepared are UK medical graduates for practice? A rapid review of the literature 2009-2014.
BMJ Open. 2017;7(1):e013656.
doi:10.1136/bmjopen-2016-013656
-
McGaghie WC, Sajid AW, Miller GE, Telder TV, Lipson L (eds.). Competency-based curriculum development in medical education: an introduction. World Health Organization; 1978
-
Frenk J, Chen L, Bhutta ZA, et al. Health professionals for a new century: transforming education to strengthen health systems in an interdependent world.
Lancet. 2010;376(9,756):1,923-1,958.
doi:10.1016/S0140-6736(10)61854-5
-
Carraccio C, Englander R, Van Melle E, et al. Advancing competency-based medical education: a charter for clinician–educators.
Acad Med. 2016;91(5):645-649.
doi:10.1097/ACM.0000000000001048
-
-
Eyal L, Cohen R. Preparation for clinical practice: a survey of medical students’ and graduates’ perceptions of the effectiveness of their medical school curriculum.
Med Teach. 2006;28(6):e162-e170.
doi:10.1080/01421590600776578
-
Lempp H, Cochrane M, Rees J. A qualitative study of the perceptions and experiences of pre-registration house officers on teamwork and support.
BMC Med Educ. 2005;5(1):10.
doi:10.1186/1472-6920-5-10
-
Tallentire VR, Smith SE, Wylde K, Cameron HS. Are medical graduates ready to face the challenges of Foundation training?
Postgrad Med J. 2011;87(1,031):590-595.
doi:10.1136/pgmj.2010.115659
-
Brydges R, Boyd VA, Tavares W, et al. Assumptions about competency-based medical education and the state of the underlying evidence: a critical narrative review.
Acad Med. 2021;96(2):296-306.
doi:10.1097/ACM.0000000000003781
-
Sherbino J, Regehr G, Dore K, Ginsburg S. Tensions in describing competency-based medical education: a study of Canadian key opinion leaders.
Adv Health Sci Educ Theory Pract. 2021;26(4):1,277-1,289.
doi:10.1007/s10459-021-10049-8
-
-
Buchman S. It’s about time: 3-year FM residency training. Can Fam Physician. 2012;58(9):1,045-1,045.
-
-
-
The College of Family Physicians of Canada. Family medicine longitudinal survey: exit survey (T2) results 2020, aggregate data for 17 participating FM programs. 2021.
-
Aggarwal M, Holtby A, Oandasan I. Factors That Influence Practice Choices of Early-Career Family Physicians: An Outcomes of Training Project evidence summary. College of Family Physicians of Canada; January 2022.
-
Whiteside C, Mathias R. Training for rural practice. Are graduates of a UBC program well prepared? Can Fam Physician. 1996;42:1,113-1,121.
-
Chan BT. The declining comprehensiveness of primary care. CMAJ. 2002;166(4):429-434.
-
Freeman TR, Boisvert L, Wong E, Wetmore S, Maddocks H. Comprehensive practice: normative definition across 3 generations of alumni from a single family practice program, 1985 to 2012. Can Fam Physician. 2018;64(10):750-759.
-
Ottrey E, Rees CE, Kemp C, et al. Exploring health care graduates’ conceptualisations of preparedness for practice: A longitudinal qualitative research study.
Med Educ. 2021;55(9):1,078-1,090.
doi:10.1111/medu.14475
-
White W, Brenman S, Paradis E, et al. Lesbian, gay, bisexual, and transgender patient care: medical students’ preparedness and comfort.
Teach Learn Med. 2015;27(3):254-263.
doi:10.1080/10401334.2015.1044656
-
Denzin NK, Lincoln YS. The Sage Handbook of Qualitative Research. Sage; 2011.
-
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups.
Int J Qual Health Care. 2007;19(6):349-357.
doi:10.1093/intqhc/mzm042
-
Khangura S, Konnyu K, Cushman R, Grimshaw J, Moher D. Evidence summaries: the evolution of a rapid review approach.
Syst Rev. 2012;1(1):10.
doi:10.1186/2046-4053-1-10
-
Linda NS, Phetlhu DR, Klopper HC. Significance of literature when constructing a theory: a selective literature review. Afr J Phys Health Edu Recreat Dance. 2014;20(sup-1):502-512.
-
-
-
Dixon-Woods M. Using framework-based synthesis for conducting reviews of qualitative studies.
BMC Med. 2011;9(1):39.
doi:10.1186/1741-7015-9-39
-
-
Krippendorff K. Content Analysis: An Introduction to Its Methodology. Sage; 2018.
-
Assarroudi A, Heshmati Nabavi F, Armat MR, Ebadi A, Vaismoradi M. Directed qualitative content analysis: the description and elaboration of its underpinning methods and data analysis process.
J Res Nurs. 2018;23(1):42-55.
doi:10.1177/1744987117741667
-
Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis.
Qual Health Res. 2005;15(9):1,277-1,288.
doi:10.1177/1049732305276687
-
Edhlund B, McDougall A. NVivo 12 Essentials. Lulu.com; 2019.
-
-
Dijkstra IS, Pols J, Remmelts P, et al. What are we preparing them for? Development of an inventory of tasks for medical, surgical and supportive specialties.
Med Teach. 2013;35(4):e1,068-e1,077.
doi:10.3109/0142159X.2012.733456
-
-
Lindberg O. ‘The next step’—alumni students’ views on their preparation for their first position as a physician.
Med Educ Online. 2010;15(1):4884.
doi:10.3402/meo.v15i0.4884
-
McKinstry B, Macnicol M, Elliot K, Macpherson S. The transition from learner to provider/teacher: the learning needs of new orthopaedic consultants.
BMC Med Educ. 2005;5(1):17.
doi:10.1186/1472-6920-5-17
-
Cave J, Woolf K, Jones A, Dacre J. Easing the transition from student to doctor: how can medical schools help prepare their graduates for starting work?
Med Teach. 2009;31(5):403-408.
doi:10.1080/01421590802348127
-
Wiener-Ogilvie S, Bennison J, Smith V. General practice training environment and its impact on preparedness.
Educ Prim Care. 2014;25(1):8-17.
doi:10.1080/14739879.2014.11494236
-
McNeil HP, Hughes CS, Toohey SM, Dowton SB. An innovative outcomes-based medical education program built on adult learning principles.
Med Teach. 2006;28(6):527-534.
doi:10.1080/01421590600834229
-
Lieberman L, Hilliard RI. How well do paediatric residency programmes prepare residents for clinical practice and their future careers?
Med Educ. 2006;40(6):539-546.
doi:10.1111/j.1365-2929.2006.02479.x
-
Monrouxe LV, Bullock A, Gormley G, et al. New graduate doctors’ preparedness for practice: a multistakeholder, multicentre narrative study.
BMJ Open. 2018;8(8):e023146.
doi:10.1136/bmjopen-2018-023146
-
Morrow G, Burford B, Redfern N, Briel R, Illing J. Does specialty training prepare doctors for senior roles? A questionnaire study of new UK consultants.
Postgrad Med J. 2012;88(1044):558-565.
doi:10.1136/postgradmedj-2011-130460
-
Junod Perron N, Audetat MC, Mazouri S, Schindler M, Haller DM, Sommer J. How well are Swiss French physicians prepared for future practice in primary care?
BMC Med Educ. 2018;18(1):65.
doi:10.1186/s12909-018-1168-4
-
Watmough S, Cherry MG, O’Sullivan H. A comparison of self-perceived competencies of traditional and reformed curriculum graduates 6 years after graduation.
Med Teach. 2012;34(7):562-568.
doi:10.3109/0142159X.2012.675457
-
Weidner AKH, Chen FM. Changes in preparation and practice patterns among new family physicians.
Ann Fam Med. 2019;17(1):46-48.
doi:10.1370/afm.2337
-
Busari JO, Verhagen EA, Muskiet FD. The influence of the cultural climate of the training environment on physicians’ self-perception of competence and preparedness for practice.
BMC Med Educ. 2008;8(1):51.
doi:10.1186/1472-6920-8-51
-
Best LR, Sengupta A, Murphy RJL, et al. Transition to practice in radiation oncology: mind the gap.
Radiother Oncol. 2019;138:126-131.
doi:10.1016/j.radonc.2019.06.012
-
Dijkstra IS, Pols J, Remmelts P, Rietzschel EF, Cohen-Schotanus J, Brand PLP. How educational innovations and attention to competencies in postgraduate medical education relate to preparedness for practice: the key role of the learning environment.
Perspect Med Educ. 2015;4(6):300-307.
doi:10.1007/S40037-015-0219-3
-
Westerman M, Teunissen PW, Jørgensen RL, et al. The transition to hospital consultant: Denmark and the Netherlands compared on preparedness for practice, perceived intensity and contextual factors.
Med Teach. 2013;35(6):481-489.
doi:10.3109/0142159X.2013.774332
-
Woloschuk W, Crutcher R, Szafran O. Preparedness for rural community leadership and its impact on practice location of family medicine graduates.
Aust J Rural Health. 2005;13(1):3-7.
doi:10.1111/j.1440-1854.2004.00637.x
-
Geramita EM, Parker IR, Brufsky JW, Diergaarde B, van Londen GJ. Primary care providers’ knowledge, attitudes, beliefs, and practices regarding their preparedness to provide cancer survivorship care.
J Cancer Educ. 2020;35(6):1,219-1,226.
doi:10.1007/s13187-019-01585-4
-
Burford B, Whittle V, Vance GH. The relationship between medical student learning opportunities and preparedness for practice: a questionnaire study.
BMC Med Educ. 2014;14(1):223.
doi:10.1186/1472-6920-14-223
-
Card SE, Snell L, O’Brien B. Are Canadian general internal medicine training program graduates well prepared for their future careers?
BMC Med Educ. 2006;6(1):56.
doi:10.1186/1472-6920-6-56
-
Cave J, Goldacre M, Lambert T, Woolf K, Jones A, Dacre J. Newly qualified doctors’ views about whether their medical school had trained them well: questionnaire surveys.
BMC Med Educ. 2007;7(1):38.
doi:10.1186/1472-6920-7-38
-
Chen CA, Kotliar D, Drolet BC. Medical education in the United States: do residents feel prepared?
Perspect Med Educ. 2015;4(4):181-185.
doi:10.1007/S40037-015-0194-8
-
Dijkstra IS, Pols J, Remmelts P, Brand PL. Preparedness for practice: a systematic cross-specialty evaluation of the alignment between postgraduate medical education and independent practice.
Med Teach. 2015;37(2):153-161.
doi:10.3109/0142159X.2014.929646
-
Barr J, Ogden KJ, Rooney K, Robertson I. Preparedness for practice: the perceptions of graduates of a regional clinical school.
Med J Aust. 2017;206(10):447-452.
doi:10.5694/mja16.00845
-
Scicluna HA, Grimm MC, O’Sullivan AJ, et al. Clinical capabilities of graduates of an outcomes-based integrated medical program.
BMC Med Educ. 2012;12(1):23.
doi:10.1186/1472-6920-12-23
-
Zafar A, Rehman A. Clinical capability self-appraisal as indicative of preparedness for future medical practice. a graduates׳ perspective.
Health Prof Educ. 2017;3(1):44-49.
doi:10.1016/j.hpe.2016.07.001
-
Stephenson J, Yorke M. Capability and Quality in Higher Education. Routledge; 1998.
-
Maisonneuve JJ, Lambert TW, Goldacre MJ. Doctors’ views about training and future careers expressed one year after graduation by UK-trained doctors: questionnaire surveys undertaken in 2009 and 2010.
BMC Med Educ. 2014;14(1):270.
doi:10.1186/s12909-014-0270-5
-
Morrow G, Johnson N, Burford B, et al. Preparedness for practice: the perceptions of medical graduates and clinical teams.
Med Teach. 2012;34(2):123-135.
doi:10.3109/0142159X.2012.643260
-
-
Kilminster S, Zukas M, Quinton N, Roberts T. Preparedness is not enough: understanding transitions as critically intensive learning periods.
Med Educ. 2011;45(10):1,006-1,015.
doi:10.1111/j.1365-2923.2011.04048.x
-
Westerman M, Teunissen PW, van der Vleuten CP, et al. Understanding the transition from resident to attending physician: a transdisciplinary, qualitative study.
Acad Med. 2010;85(12):1,914-1,919.
doi:10.1097/ACM.0b013e3181fa2913
-
Wijnen-Meijer M, Ten Cate OT, Van Der Schaaf M, Borleffs JC. Vertical integration in medical school: effect on the transition to postgraduate training.
Med Educ. 2010;44(3):272-279.
doi:10.1111/j.1365-2923.2009.03571.x
-
Phelps R, Hase S, Ellis A. Competency, capability, complexity and computers: exploring a new model for conceptualising end‐user computer education.
Br J Educ Technol. 2005;36(1):67-84.
doi:10.1111/j.1467-8535.2005.00439.x
-
Scott G. Transforming graduate capabilities & achievement standards for a sustainable future. Final Report National Senior Teaching Fellowship. Australian Government Office for Learning and Teaching; 2016.
-
Schwartzstein RM, Dienstag JL, King RW, et al; Pathways Writing Group. The Harvard medical school pathways curriculum: reimagining developmentally appropriate medical education for contemporary learners.
Acad Med. 2020;95(11):1,687-1,695.
doi:10.1097/ACM.0000000000003270
-
-
Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains.
Acad Med. 2004;79(10)(suppl):S70-S81.
doi:10.1097/00001888-200410001-00022
-
Cruess RL, Cruess SR, Boudreau JD, Snell L, Steinert Y. Reframing medical education to support professional identity formation.
Acad Med. 2014;89(11):1,446-1,451.
doi:10.1097/ACM.0000000000000427



There are no comments for this article.