While most graduate medical training programs require attending physicians to meet, examine, and discuss the plan of care for every patient in order to bill insurance, the Medicare Primary Care Exception (PCE) permits indirect supervision of residents performing lower-complexity visits in primary care settings. 1 Higher-complexity visits in primary care historically have required direct (in-person) supervision. Previous studies have demonstrated that residents bill significantly fewer higher-complexity visits at programs applying PCE guidelines to all patients, compared to programs applying guidelines only to patients with Medicare. 2, 3
To promote physical distancing and to facilitate telemedicine during the COVID-19 pandemic, Medicare permitted use of higher-complexity codes without direct attending supervision, thus expanding the PCE to all patient visits. 4 This study investigated the impact on resident billing practices at a single family medicine residency during calendar year 2020. We hypothesized that universal indirect supervision would increase use of high-complexity codes.
We queried billing codes associated with the University of Washington Family Medicine Residency from January to December 2020. We disidentified data and filtered it to include only established evaluation and management (E/M) codes (99211-99215). Lower-complexity codes included 99211-99213; 99214-99215 were high-complexity. PCE-ineligible visits performed by first-year residents were excluded. We compared billing patterns by physician type (resident or attending) by quarter: Q1 (January-March 2020), Q2 (April-June 2020), Q3 (July-September 2020), Q4 (October-December 2020). Pre-PCE expansion is represented by Q1 of 2020. Medicare adopted the PCE for all patients in the last week of Q1. Due to the delay in rule adoption and decreased patient volumes in Q2 and Q3, we selected Q4 (October-December) for post-PCE expansion comparison. We used χ2 tests to analyze the bivariate relationship between resident/attending physician status and the proportion of visits coded complex during each quarter. We used generalized estimating equations to account for correlated visit data in all logistic regressions. Analyses were done using SAS version 9.4 (SAS Institute) statistical software.
This study was reviewed and exempted by the University of Washington Institutional Review Board.
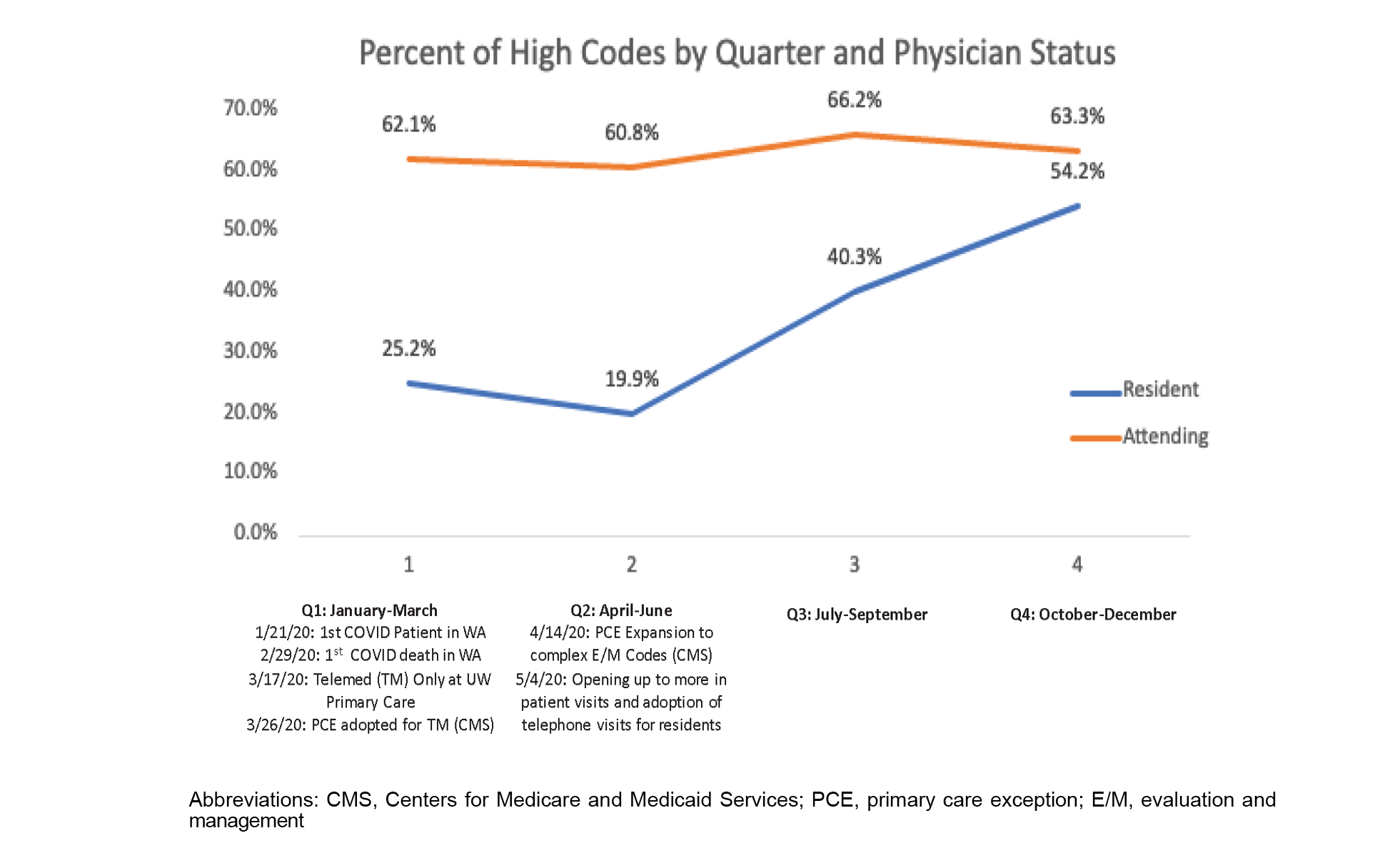
Table 1 describes physicians and their number of established E/M visits. Resident high-complexity code use increased in Q4 (OR 3.50 [2.34-5.23]) compared to Q1. No change was observed among attendings (OR 1.05 [0.86-1.28]). Resident and attending billing patterns became more similar following PCE expansion (OR for higher-complexity code use by physician type was 4.85 [3.43-6.85] in Q1, 1.46 [0.89-2.38] in Q4). Numbers of unique attending and residents represented by quarter are listed. Individual physician contribution to visits performed was not assumed to be equal across all quarters. Following implementation of PCE expansion guidelines in April 2020, resident physicians billed more higher-complexity visits.
Odds ratios of higher-complexity code usage between attending and resident physicians decreased throughout the year, with Q4 showing no significant difference in coding patterns (Table 2). Code usage comparison between Q4 and Q1 by physician type demonstrates that residents were significantly more likely to use higher-complexity billing codes in Q4, whereas code usage did not significantly change among attendings (Figure 1).
The COVID-19 pandemic PCE expansion created a natural experiment for universal indirect supervision of senior residents. Our finding that universal indirect supervision resulted in more frequent application of higher-complexity codes raises important questions about resident supervision in primary care training and has policy implications regarding the future of the PCE.
Pre-COVID PCE rules allowed indirect supervision of residents performing preventive and lower-complexity visits (represented by E/M codes 99211-3 for established patients). For residents to use higher-complexity E/M codes (99214-5), the pre-COVID PCE required direct attending supervision with in-person evaluation. 1
Previous work has suggested that billing practice is impacted when permission to use higher-complexity codes is contingent on residents making real-time decisions about precepting. High-complexity code usage has been shown to increase with implementation of universal direct precepting 5 and, conversely, to decrease in settings where PCE guidelines were applied to patients with all insurance types, not just Medicare. 2 This finding suggests that resident usage of high-level codes is not due to a lack of billing education but rather to the existence of other barriers, such as time, system rule interpretation, or preceptor availability.
Billing of lower complexity codes by residents when a higher code would be appropriate has an impact on financial health. A previous study of 16 family medicine residencies compared resident billing to Medical Group Management Association (MGMA) benchmarks and estimated the aggregate annual loss at $481,654. Over the study period, 13 of the 16 residency programs demonstrated a revenue loss. Three programs were projected to lose more than $100,000 annually. 6 A return to prepandemic PCE rules, which rely on resident discretion to identify higher-complexity and real-time precepting, likely will result in the use of more low-complexity codes. The negative financial consequences could harm residency clinics, especially programs with greater reliance on clinical revenue.
Some may be concerned that loosened supervision requirements will erode the quality of resident education or impact the quality of patient care. This is an area for further research. Other health professionals, notably nurse practitioners and physician assistants, see patients using indirect supervision without completing a period of supervised training (ie, residency) following graduation from programs shorter in duration than medical school. If these professionals are trusted to recognize their limits, one could argue that resident physicians are capable of the same level of autonomy.
The idea of supervision needs to be reevaluated in the context of the technological transformation in primary care that was accelerated by the pandemic with the rapid adoption of telemedicine. Residents in primary care no longer are caring for patients only in-person; they are performing telemedicine visits, reviewing patient-reported data, and providing care in other ways that do not require physical meetings. Remote precepting has the potential to improve preceptor-to-resident staffing ratios and reduce the burden of space constraints on physicians and support staff. Teleprecepting has been adopted across multiple institutions. 7 Reverting to prepandemic PCE rules has the potential to stifle innovative teaching methods.
With the PCE expansion, senior primary care resident physicians were empowered to bill higher-level codes under indirect universal supervision. The findings of this study have implications for the financial well-being and sustainability of primary care residency training and raise relevant policy questions about whether the PCE expansion should persist. Striking a balance between promoting resident independence and ensuring that residents have appropriate support and supervision during training is important. More research is needed to determine whether these findings were replicated in other primary care residency practices, the impact on resident education, and the impact on patient outcomes.



There are no comments for this article.