Background and Objectives: Scholarly activity is a core requirement set by the Accreditation Council for Graduate Medical Education (ACGME). A previous study documented a significant 302% increase in scholarly activity at Eglin Family Medicine Residency after implementation of a standard set of interventions from 2016 to 2019. Few researchers have explained why such interventions to increase scholarly activity are effective. Prior work has suggested that many different interventions are helpful, but why? Our qualitative study took a multilevel approach to explain accompanying cultural factors and to determine how specific interventions led to the observed increases in quality and quantity of resident scholarship.
Methods: Taking a grounded theory qualitative approach, we interviewed a cross-section of high- and low-producing residents (12) and faculty (5) using a semistructured interview guide. Data analysis occurred concurrently with interviews. The team iterated the interview guide three times until core code saturation was achieved. Then axial coding occurred, and our team developed a grounded theory of scholarship cultural change.
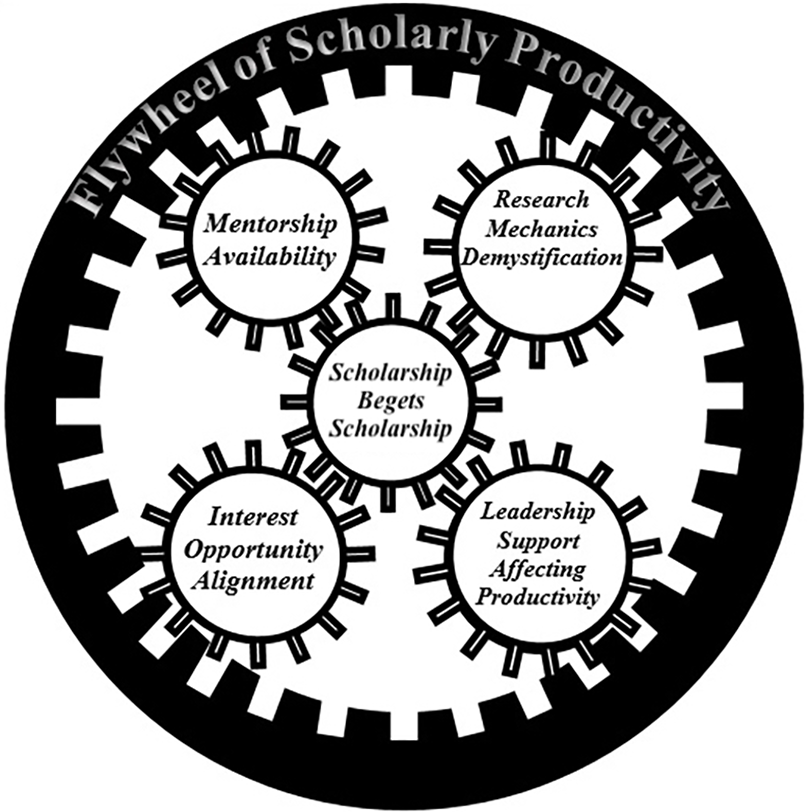
Results: During the transformation period of 2016 to 2019, participants identified mentorship availability, interest/opportunity alignment, research mechanics demystification, leadership support affecting productivity, and scholarship begets scholarship as key factors that promulgated the culture change leading to increased scholarship productivity. No single factor led to increased scholarship. Collectively, they mutually reinforced one another.
Conclusions: This explanatory inquiry developed into a multilevel model which suggests that the synergy of promoting elements drives increased scholarly productivity. Other residencies should consider fostering these combined elements instead of emphasizing only isolated individual elements to increase resident scholarship productivity.
A goal of the scholarly activity core requirements set by the Accreditation Council for Graduate Medical Education (ACGME) is for all residency programs to develop critical thinking, learn critical appraisal of the medical literature, and foster lifelong learning. 1 Within family medicine, residents should complete two scholarly activities, including a quality improvement project, and disseminate this scholarship prior to graduation. 2 Prior research documents several recognized barriers to accomplishing resident research, including lack of protected time, training, mentors, administrative support, presentation venues, and funding. 3 Due to these constraints, avoiding resident perception that scholarship is simply an additional requirement can be difficult.
To overcome these barriers, residencies have implemented interventions, including mentorship, providing protected time, and delivering didactics. 4 The Naval Hospital Jacksonville Family Medicine Residency program developed and implemented a primarily resident-driven scholarly activity curriculum, which resulted in a significant increase in scholarly activity and resident participation. 5 That curriculum included designating a resident research coordinator as a peer leader for scholarship, implementing an introduction to research basics case report workshop, 6 and sharing a scholarly activity guidebook. 7 Secondary changes included the institution of a scholarly activity point system, 8 prominent exhibition of scholarly activity in organizational hallways, intentional mentorship from faculty, 9 and frequent reminders of upcoming venues for research dissemination. Finally, increased networking and infrastructure from programs like the Military Primary Care Research Network (MPCRN) and the Council of Academic Family Medicine Educational Research Alliance (CERA) 10 were used to provide opportunities for intraprogram collaboration and sharing of resources. This success was then replicated at Eglin Family Medicine Residency, which is a 12/12/12 fully accredited program with 14 faculty nestled within a community military hospital as an unopposed residency. Application of this curriculum led to a documented 302% increase in conference presentation submissions compared to the previous 3-year average and a 91% increase compared to the preintervention year. 11
Across multiple programs, a similar theme has been noted: Implementing a wide array of interventions to foster scholarly activity increases production. 4 Indeed, Wood et al’s systematic review of 32 articles on initiatives to increase graduate medical education (GME) scholarly activity concluded, “A culture of emphasis on resident scholarship is the most important step.” This finding suggests commonalities underlying the nature of specific interventions. While Eglin’s scholarship output change was evaluated quantitatively, the second and fourth authors, who were present during the change, also sensed a culture shift in how scholarly activity was perceived and integrated in the residency. Focusing on the elements contributing to this cultural change, we conducted a qualitative study to determine what interactive elements existed during the observed period of increased scholarly productivity. Additionally, we wondered whether a penumbra of scholarship extended beyond residency participation. Did graduated residents, now attending physicians, persist in their scholarly pursuits?
Using a grounded theory approach, we designed and implemented a qualitative study to develop a model of influences that impacted resident scholarship after a period of curricular intervention. This study was deemed exempt by the Wilford Hall Ambulatory Surgical Center Institutional Review Board (IRB). For the purposes of this study, we defined scholarship as research or scholarly activity to include authoring peer-reviewed and nonpeer-reviewed articles, presentations, or chapters; or conducting Institutional Review Board–approved projects including research studies or exempted process or quality improvement projects. The terms research and scholarly activity were used interchangeably and usually together when interviewing participants.
Our primary research questions sought to explore the influences on residency scholarship’s quantity and quality at Eglin’s program during the years 2016 to 2019. We developed a subsequent secondary research question to understand how these influences impacted a residency graduate’s motivation to accomplish scholarship beyond graduation. That question explored the persistence, or its lack, of motivation beyond graduation from the residency milieu. Our three research questions were:
-
Why did the quantity of scholarly research increase between 2012 and 2018?
-
Why did the quality of scholarly research increase between 2012 and 2018?
-
How did this (these) intervention(s) affect resident motivation for scholarship beyond graduation?
We purposively sampled both high- and low-producing residency graduates and faculty who were at the program during the time of increasing scholarly productivity. We defined high producers as residents who produced three or more high-quality projects, which included IRB-approved projects and/or peer-reviewed publications. Low producers were those who met the minimum ACGME requirements of two scholarly activities. We did not quantify faculty output into high- and low-performing groups. The interviewer role was shared by all four authors. We chose this approach to enable a robust discussion about the emerging data. The interview was structured by a guide (Table 1 ) with two demographic questions and 12 open-ended questions, including additional probes as applicable. Topics included overall impressions of research, the program’s scholarly activity levels, and facilitators and barriers to scholarly activity. As data was gathered, we revised our interview guide using the constant comparative method, 12 combining data collection with data analysis. Our research team met three times to identify core codes and to revise our probes to capture emerging information from the next set of participants.
|
Demographics
|
|
What year did you graduate from medical school?
|
|
In the years 2016-2017, were you a resident or a faculty member at the Eglin Family Medicine Residency?
|
|
Focus Questions
|
|
If a faculty interview, skip this question. In medical school, did you participate in research or scholarly activity? Yes or no If yes, describe the activity. If no, move to the next question.
|
|
What made you choose this program for residency (or as a faculty member)? What was the reputation of the residency program in research or scholarly activity?
|
|
When you started at your FMRP, what were your first impressions of research or scholarly activity in the program?
|
|
Probe 1
|
How did residency requirements affect your participation in research or scholarly activity? If a faculty interview, skip this question. How did your motivation change over time to do scholarly activity?
|
|
Probe 2
|
When you first thought about doing research or scholarly activity, did you think that you could accomplish the requirements? Why or why not? What barriers did you actually encounter while accomplishing research or scholarly activity? How did you overcome the identified barrier?
|
|
Tell me about a time you did research or scholarly activity in residency.
|
|
Probe 1 (resident probe)
|
Tell me about another experience. What do you think was different between these experiences? Is there a reason you didn’t engage in more research or scholarly activity?
|
|
Probe 2 (faculty probe)
|
Tell me about a time you participated in research or scholarly activity with a resident.
|
|
What impact did your fellow residents or faculty have on your research or scholarly output?
|
|
Probe 1
|
How did your fellow residents impact your research or scholarly activity endeavors?
|
|
Probe 2
|
How did residency faculty impact your research or scholarly activity endeavors?
|
|
What was helpful for you in doing research or scholarly activity? Were specific resources helpful? Why?
|
|
Probe 1
|
What residency resources were helpful to you?
|
|
Probe 2
|
Did nonfaculty help you with research or scholarly activity? Yes or no If yes, what activities did they do that helped you? If no, was there anything you felt you needed to further help you?
|
|
For faculty (skip for residents): During your time in residency (or as faculty), how did the types of resident research or scholarly projects change? By types of projects, we mean poster presentations, FPIN, USAFP talks, IRB approved projects, help desk inquiries, PI/QI, book chapters.
|
|
During your time in residency (or as a faculty member) at this FMR, did the program’s curriculum change regarding research or scholarly activity from the time you started to the time you graduated?
|
|
Probe (if yes)
|
Tell me more about the specific program curriculum that changed. Why do you think your residency program changed the research or scholarly activity curriculum? How did you feel about the changing curriculum? What was your response to these changes?
|
|
Since graduating (or leaving as a faculty member), have you done any research or scholarly activity? Yes or no
|
|
Probe (if yes)
|
Tell me about what research or scholarly projects you have been involved with since graduating. How did your experience at FMR affect your research or scholarly activity after leaving?
|
|
Tell me about your plans for engaging in future research or scholarly activity.
|
|
Is there anything else you would like to tell me about what we have talked about today?
|
|
Do you have any questions for me?
|
We completed 17 interviews (three from the graduated class of 2017, four from the graduated class of 2018, and five from the graduated class of 2019; and five faculty interviews). The sample included a mix of six high and five low resident producers of scholarly activity. One resident graduate interview did not fit either the high or low producer category. Interviews resulted in 6 hours and 7 minutes of data collected, or 98 pages of transcribed text. The shortest interview lasted 11 minutes and 38 seconds. The longest interview lasted 27 minutes and 9 seconds.
The first, second, third, and fourth authors met to explore emergent core codes. Once we reached saturation of our core codes, we developed our codebook and then set about axial coding. Axial coding consists of identifying recurrent core codes, extracting the conceptual relationship within these recurrences, naming, and then applying this secondary order or axial code to the data. After we completed axial coding, we next developed a relational theory detailing these thematic factors. Finally, the authors developed a grounded theory to describe the interplay of these factors. To validate our findings, three research participants reviewed and approved our axial codes.
We found five elements or themes influencing the residency’s culture of increased scholarship productivity. Those themes were mentorship availability, interest/opportunity alignment, research mechanics demystification, leadership support affecting productivity, and scholarship begets scholarship (Table 2). We noted that these elements fostered scholarship at the individual level (mentorship, interest/opportunity alignment), the program level (research mechanics demystification), and the sponsoring institution level (leadership support affecting productivity). We realized that these levels underscored the comprehensive multilevel cultural change present during the residency’s transformation.
|
Mentorship availability : Availability of both faculty and residents’ mentors increased quantity and/or quality of scholarship.
|
|
“It was a resident . . . when I was an intern that helped me through that process because they had done something similar before . . . and not just the process of making it, but where he got the information. Some places to look for better resources for this particular topic, that kind of thing.”– Residency grad 8
“His [faculty] excitement about research is contagious . . . he really motivated me and was a great mentor.” – Residency grad 1
“Dr [faculty mentor] published one too at the very end of my third year. . . . He was very persistent and encouraging. . . . Just having a mentor that does that . . . and then agrees to read, review your rewrite, and help you submit, and ‘hey, what about this journal? What about that journal?’” – Residency grad 4
“So one of the faculty, he kind of took me under his wing and said, ‘Hey, I have this project. You wanna work on it?’ And I said, ‘Yep, I will work it with you. No problem.’ Because I knew I needed [it] for graduation . . . it also went in line . . . with my interests at the time.” —Residency grad 3
|
|
Interest/opportunity alignment : Advertising opportunities led to shared interests driving collaboration.
|
|
“That assigned mentor can plug them in with a mentor who might have interest similar to theirs or plug them into a project that might be interesting to the resident based on what they want to accomplish and what their own personal goals are.” – Residency grad 5
“Dr [faculty mentor] was there, too, and talking about all these different things that people have done in the past and kind of opportunities that come up frequently.” – Residency grad 1
“He [resident] was just really passionate. . . . He brought a few of my classmates into some of his projects. . . . When we stood up the concussion [clinic] protocol is when I think I felt a change in motivation to do research throughout the residency.” – Residency grad 5
“If you have a passion for something, then it’s a much better driver and incentive to do something than if you just tell somebody to do it just as an order. . . . If you tell somebody to do something just because you want them to or to meet a metric . . . they’ll go to the bare minimum as opposed to somebody who’s passionate about something, and you facilitate that passion. You will typically get a better quality result.” – Residency grad 3
|
|
Research mechanics demystification : The residency provided instructions and resources to aid scholarly activity processes.
|
|
“[Research instructors] actually came and visited the residency and told, you know, outlined their process for us. . . . We just kind of followed the steps, did the research, and . . . did wind up getting that published.” – Residency grad 6
“The biggest part of it was faculty that actually started pushing it and actually doing these didactic sessions and getting these workshops set aside where we had a full theme day [designated didactic half day] that was dedicated [to] writing an abstract and just making residents realize that this is something that you can do . . . is not meant to be something that’s this huge project that you’re never gonna be able to accomplish” – Residency grad 11
“Dr [resident mentor] was a resident as well at the same time, but having a mentor that was a year ahead of me on helping [with] some of the stuff . . . like primary research. . . . She was really good at helping navigate the logistics of obtaining that kind of information” – Residency grad 9
“We had the one presentation where they came in and actually taught how to do a case presentation. And that was the year that [there were] a lot of the case presentations . . . at USAFP [regional specialty chapter annual meeting] because it was finally a structured program. They came in for 4 hours. You almost had a full abstract by the end of the case study workshop . . . as far as this is how you set up in the case study. This is how you get started.” – Residency grad 11
|
|
Leadership support affected productivity: The presence and absence of leadership verbal and nonverbal support affected scholarly production.
|
|
“I could see the other residents secure time for themselves from the residency. . . . There was some time that I think took a research block . . . so it just made it clear to me that it was doable.” – Residency grad 2
“We had an increase in the amount of support staff we had. Like Dr [faculty mentor] became a stronger force . . . in helping us with analysis of data and getting different aspects of our research projects approved.” – Residency grad9
“They [faculty] would keep follow[ing] up. . . . ‘Need anything?’. . . ‘Do you know what the guidelines are? How can I help you find that stuff’ . . . just continuing to follow up because . . . if you don’t keep working on things, they just kind of fall off and peter out.” – Residency grad 4
“We [the faculty] have to put into writing a new expectation in the resident handbook and also just start modeling how we’re going to do things differently. . . . And then when research opportunities or presentation opportunities came up, the [hospital leadership] and the residency was certainly supportive of getting people to those locations and/or the printing of posters. That was certainly assist[sic] in things.” – Faculty 2
|
|
Scholarship begets scholarship: Scholarship involvement motivated further scholarship involvement by modeling project completion.
|
|
“I think once it started that people were doing above and beyond the required scholarship activities that it just feeds off itself and just kind of continued.” – Residency grad 8
“When you get involved with a project and that kind of sucks you in . . . then usually from one leads to the next.” – Residency grad 4
“So I started with a case presentation with one [of] my patients that I had as an intern. . . . That was just a really interesting case and I presented it at Mayo Clinic. And after that I was pretty hooked on case presentations. I thought that it was a lot of fun to do the research and actually, um, have the relationship with the patient and let them know, ‘Hey, I think your case is interesting. I think doctors can learn from it.’” – Residency grad 11
“I wanted to emulate some of my other classmates or older residents and I wanted to emulate my attending. I think I left Eglin with four different publications, and I have done three since I left.” – Residency grad 5
“There was a . . . nice bulletin board in the hall [where residents transit back and forth from offices] there that kind of highlighted and showcased some of the research that had been done there in the past. So that was always very motivating to walk past.” – Residency grad 4
|
Mentorship Availability
Mentorship availability increased both the quantity and quality of scholarship. Importantly, participants commented on the presence of both faculty and resident mentors. Mentorship often led to a better understanding of the research process and provided a means for interest/opportunity alignment. Mentorship occurred between and among both residents and faculty.
Interest/Opportunity Alignment
Participants repeatedly commented that advertising opportunities led to the discovery of shared interests that then seeded collaboration. Often these opportunities flowed between mentors, but we noted that informal and formal mentorship networks invariably developed when advertised opportunities provided shared interest expressed through collaboration.
Research Mechanics Demystification
When the program demystified the scholarly work process by providing instructions and resources, scholarly productivity increased. Participants expressed that mentors were important as resources to demystify perceived barriers.
Leadership Support Affecting Productivity
Participants reported that leadership support, through verbal and nonverbal cues, affected production. Leadership support fostered mentorship (through verbalized formal relationships) as well as research mechanics demystification through nonverbal cues including curricular support and resource allocation for conference attendance.
Scholarship Begets Scholarship
Participants depicted a cultural connection of norms and behavior, describing how scholarship begets scholarship. Participants observed that scholarship involvement motivated further scholarship involvement by modeling project completion.
As described earlier, mentorship availability, interest/opportunity alignment, research demystification, leadership support, and scholarship begetting scholarship all emerged from our interviews as contributors to culture development. Notably, all five themes were present among high/low performers and also were noted by faculty, suggesting how these themes expressed the development of a new culture of scholarship.
Moreover, these individual cultural elements interacted in intriguing ways. For instance, the availability of mentorship grew as more and more faculty and residents gained scholarship experience. As scholarship begot more scholarship, more opportunities emerged, leading to increased opportunities for residents to find opportunities aligned with their personal interests. Furthermore, the residency leadership provided support through formal education sessions and outside resources, which demystified the mechanics of research. This support, in turn, led to lowering barriers and fostering better participation, which in turn created the conditions for further mentorship, which then led to prior scholarship begetting future scholarship. As we considered the residency’s cultural change, a theory of this interaction began to emerge. We conceptualized the interaction visually as a planetary gear where the middle (or sun) gear spins the rest of the individual gears (Figure 1).
The complexity of our model points to the known interrelated nature of any cultural change. As the apparatus builds up speed, all elements must interact to spin faster and faster. The structure is not hierarchical because all elements must interact to spin the wheel. As the mechanism spins faster, it is dependent on its inner cogs to maintain velocity. Thus, if an institution has more scholarship, opportunities for mentorship and interest/opportunity alignment are greater. Moreover, the rate of the spin is limited by leadership support as well as research mechanics demystification. If additional resources are not provided, the rate of scholarly productivity is inhibited because the limited speed of any one element deleteriously impacts the speed of the others. Conversely, if leadership provides resources but no mentors and few opportunities, the mechanism will not turn faster.
We found further support for this interaction from graduated residents’ experiences with scholarly activity after residency. Interestingly, while numerous graduates expressed motivation for scholarly activity participation after residency, few actually participated. Beyond residency, our research indicated that motivation to continue research was maintained but that organizational factors often precluded participants from continuing scholarly activity. When asked about whether they had continued mentoring others in scholarly activity beyond graduation, one residency graduate (residency grad 4) in a nonacademic job responded, “No, I would love to but this just isn’t the place for it, because, um, yeah, everybody is just so tired. I don’t know. I’ll be honest. It’s just there’s no time for it, you know. It just goes by the wayside.” When asked about plans to engage in future research or scholarly activity, another (residency grad 2) reported, “openness to other research, yes. But no specific plans at this point. No, because I’m moving. . .. I don’t know the environment there and I don’t have a specific research question, but I’d be open to it, if something sort of fell into my lap or if an interest developed.” These comments suggested that interest alone was inadequate to accomplish scholarly activity, indicating that more than this was needed to sustain productivity.
Our findings suggested that the standard interventions of a resident research coordinator, a case report workshop, and a research guidebook fostered culture change and were not individually the main cause of the observed increased scholarly productivity. We suspect that implementing multiple interventions caused the cultural changes that fostered the scholarly productivity. The importance of multilevel interventions described in our study demonstrates the validity of prior work, which recommended that multiple interventions are needed to overcome real and perceived barriers to resident scholarship. 13 Additionally, our observed cultural elements (mentorship availability, leadership support, interest/opportunity alignment) have been previously described as bright spots in other successful family medicine research. 14 Our model also may explain why these other interventions have proven effective. 4, 14 The success was not the result of the interventions themselves, but rather from the multilevel culture changes they created. In other words, the interventions synergistically drove culture change. This cultural change reduced uncertainty about accomplishing the scholarly activity requirement and thus increased mentorship, which promoted resident scholarship productivity.
Ours is the first study to qualitatively assess cultural contributing factors experienced by participants during a period of significantly increased scholarly productivity at a community-based family medicine residency. Although our study’s findings are bound to this setting, the cultural elements of mentorship, leadership, scholarship opportunities, and scholarship instruction have been observed in other settings, including medical schools 14 and other subspecialty residencies. 4, 15 Our model proposes that multilevel interventions, as opposed to focusing on individual elements, will lead to increased scholarship through cultural transformation. Further, we contend that building such productivity hinges on fostering a synergistic interaction among multiple supporting elements.
While the precise interface and proportionality of each cultural element will differ from institution to institution, knowledge that such interactions existed in our resource-limited community-based military residency program and led to increased scholarship may prove helpful in other settings. Instead of resourcing one element exclusively, a residency program will likely find greater success by dividing limited resources to promote the individual elements (increasing mentorship, aligning resident interest with opportunities), the program element (demystifying research), and the institutional element (leadership support).
Our findings and emergent model must be considered within its original context.
Although we captured a diverse set of resident experiences by sampling from different class years with both high and low scholarly productivity, we did not interview all residents and all faculty during the study time frame. Thus, some perspectives may not be incorporated into our research. Also, we struggled to delineate between factors that increased quality versus quantity. The nature of our structured interviews lent themselves better to evaluating greater scholarly involvement as opposed to delineating the quality of such involvement. Although we observed factors that increased scholarly activity, we had difficultly determining whether such factors increased quantity or quality, or both. Future work in this area of research would involve exploring the presence and absence of these multilevel factors and their interactions in other settings that have experienced similar scholarly productivity increases. Such an approach would further refine our proposed theory of resident scholarship productivity.
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the US Department of the Air Force, the Department of Defense, or the United States Government.
Funding support was provided through a grant from the Uniformed Services Academy of Family Physicians (Grant number: #18 LG-1).
Acknowledgments
The authors thank the current and previous faculty and graduated residents of Eglin’s family medicine program for their participation. The authors also thank Esther Guard, DO, and Christy Ledford, PhD, for their assistance with project conceptualization and editing.
References
-
-
-
Lennon RP, Rabago D, Deneke E, et al. Results of a military family medicine scholarly activity training needs assessment.
Mil Med. 2023;188(1-2):e374-e381.
doi:10.1093/milmed/usab174
-
Wood W, McCollum J, Kukreja P, et al. Graduate medical education scholarly activities initiatives: a systematic review and meta-analysis.
BMC Med Educ. 2018;18(1):318.
doi:10.1186/s12909-018-1407-8
-
Lennon RP, Oberhofer AL, McNair V, Keck JW. Curriculum changes to increase research in a family medicine residency program. Fam Med. 2014;46(4):294-298.
-
-
-
-
Cafferty LA, Crawford PF, Jackson JT, Ledford CJW. Residency leader motivations to engage residents and residency faculty in scholarship: a qualitative study.
Fam Med. 2020;52(8):581-585.
doi:10.22454/FamMed.2020.437433
-
Seehusen DA, Mainous AG III, Chessman AW. Creating a centralized infrastructure to facilitate medical education research.
Ann Fam Med. 2018;16(3):257-260.
doi:10.1370/afm.2228
-
Lennon RP, Fuentes RWC, Broszko C, Koch JJ, Sanchack K, Keck JW. A curriculum to increase resident scholarly activity.
Fam Med. 2020;52(8):557-561.
doi:10.22454/FamMed.2020.257274
-
Glaser BG, Strauss AL. The Discovery of Grounded Research: Strategies for Qualitative Research. Aldine De Gruyter; 1967.
-
Ledford CJ, Seehusen DA, Villagran MM, Cafferty LA, Childress MA. Resident scholarship expectations and experiences: sources of uncertainty as barriers to success.
J Grad Med Educ. 2013;5(4):564-569.
doi:10.4300/JGME-D-12-00280.1
-
Liaw W, Eden A, Coffman M, Nagaraj M, Bazemore A. Factors associated with successful research departments a qualitative analysis of family medicine research bright spots.
Fam Med. 2019;51(2):87-102.
doi:10.22454/FamMed.2018.652014
-
Robbins MS, Haut SR, Lipton RB, et al. A dedicated scholarly research program in an adult and pediatric neurology residency program.
Neurology. 2017;88(14):1,366-1,370.
doi:10.1212/WNL.0000000000003626



There are no comments for this article.