According to the American College of Obstetricians and Gynecologists (ACOG) and the American Academy of Pediatrics, the menstrual cycle is a vital sign that clinicians can use to evaluate female reproductive health.1, 2 Menstrual cycle data provides insight into a patient’s overall health status and the underlying hormonal environment needed to support ovulation.3 In a 2015 Committee Opinion, ACOG stated that the clinical evaluation of abnormal menstrual patterns in adolescence may improve early detection of health concerns in adulthood.2
ORIGINAL ARTICLES
Fertility Awareness-Based Methods for Family Planning and Women’s Health: Impact of an Online Elective
Marguerite Duane, MD, MHA, MSPH | Logan Waechtler, MPH, MPA | Margaret May, BS | Deepa Manda, MPH, BS | Noah F. Gomez, MD | Theresa M. Stujenske, PhD, RN
Fam Med. 2024;56(7):414-421.
DOI: 10.22454/FamMed.2024.562177
Background and Objectives: Fertility awareness-based methods (FABMs) are evidence-based means of tracking observable biomarkers of a woman’s fertility for the purpose of reproductive health monitoring and family planning. However, medical education regarding FABMs is limited. The purpose of this study was to examine the effect of a 4-week, two-part online elective on students’ knowledge of FABMs, confidence in explaining and offering them to patients, and anticipated behaviors in future practice.
Methods: The online elective, “FABMs for Family Planning and Women’s Health,” was delivered from August 2020 to May 2023. Students completed pre- and postknowledge surveys. Paired t tests and the Wilcoxon signed rank test were used for analysis of the data.
Results: A total of 571 students completed the elective, and 462 students completed both pre- and posttest surveys (response rate=81%). Students’ knowledge of FABMs increased significantly. Posttest scores increased by a mean of 9.02 for Part A and 5.95 for Part B. We identified a significant increase in students’ confidence discussing FABMs to avoid pregnancy, achieve pregnancy, monitor reproductive health, and address reproductive health concerns. At the completion of the elective, students were significantly more likely to offer FABMs as an option for most or all women.
Conclusions: This online elective addresses the knowledge gap in FABMs and was effective in improving students’ knowledge of FABMs and their confidence and willingness to offer these methods to patients for family planning and management of common women’s health conditions.
The Fifth Vital Sign
To monitor this vital sign of health, individuals can learn to track observable external biomarkers, including vaginal bleeding, cervical fluid secretions, basal body temperature, and urinary hormone measurements, through the use of fertility awareness-based methods (FABMs).4 By learning to chart the signs of the reproductive cycle using FABMs, women gain insight into their daily hormonal health and knowledge to identify their fertility status for family planning purposes.3-5 Furthermore, physicians trained in FABMs can use menstrual cycle data to aid in the diagnosis, evaluation, and management of myriad medical conditions, including abnormal uterine bleeding, irregular cycles, mood disorders, and painful periods.6
Research has shown that 43% of women would be interested in using FABMs for health monitoring, and 50-61% of surveyed women have expressed interest in learning these methods for family planning.7, 8 The recent explosion of fertility tracking apps and growth in the FemTech industry suggests an increasing public awareness of the importance of menstrual health data and increases the urgency for future medical professionals to learn about FABMs, particularly the evidence supporting various technologies available to track and monitor the menstrual cycle. 4, 9
Gap in FABM Education
Menstrual cycle data has important implications for health monitoring, family planning, medical diagnosis, and disease management; however, studies consistently have shown that only 1% to 4% of medical professionals receive formal training in FABMs.10, 11 A 2022 study objectively evaluated medical school reproductive health curricula by counting the number of mentions of approximately 70 terms documented in official course content.12 Of the more than 9,000 mentions, FABMs were mentioned less than 4% of the time, and fewer than one-third of schools specifically mentioned modern, evidence-based methods.12 More commonly, the general terms “fertility awareness” or “natural family planning,” or outdated terminology such as the “rhythm method” were mentioned.
Research has shown that the overwhelming majority of physicians do not counsel patients about FABMs because they do not feel qualified due to significant knowledge gaps.13-18 A 2010 study of obstetricians/gynecologists and family physicians in Canada showed that only 3% to 6% had correct knowledge of the effectiveness of methods, including the basal body temperature, standard days, lactational amenorrhea, and the Billings ovulation method.17 Another survey found that most primary care physicians are misinformed about the effectiveness of FABMs. Half of them do not mention them as an option when patients ask about contraception, and an additional 24% only mention them with reservations.14 Another survey of clinicians from Title X clinics showed considerable variability in their understanding of what FABMs are and how the methods may be used in the clinical setting.19 However, physicians and nurses both agreed that the single most important factor for providing fertility awareness education is the presence of trained medical professionals, ideally educated via an online certification program.16 Given the implications of FABMs for health promotion and family planning, adequate training in these methods is vital for medical professionals. Increasing medical professionals’ knowledge of FABMs will facilitate reproductive and family planning programs marked by informed choice through the use of a shared decision-making model that incorporates patient preferences.20-23 Given the knowledge gap in FABMs, 12, 13 an urgent need exists for an elective course that specifically addresses these methods so that they be incorporated in clinical practice among the other options offered in reproductive and family planning services. 20
Elective Course
In 2018, Georgetown University approved a 2-week, online elective on FABMs for family planning offered through the Fertility Appreciation Collaborative to Teach the Science (FACTS), a collaborative project of the Family Medicine Education Consortium. The elective was primarily offered to fourth-year medical students around the country. Simultaneously, the university offered a 6-week hybrid elective (online and in-person) to second-year Georgetown medical students. Then, in 2019, in collaboration with faculty at Carroll College, the elective was offered to nursing students during the spring semester via a hybrid model. 17 From July 2018 through June 2020, 120 students participated in the elective, including 80 fourth-year medical students, 16 second-year medical students, and 24 nursing students.18 The results showed a statistically significant increase in knowledge scores for all three groups of students, regardless of format, highlighting the effectiveness of both an online and hybrid course model for improving students’ knowledge and confidence in offering FABMs to future patients. 18
In the summer of 2020, the elective was expanded from a single 2-week elective focused on FABMs for family planning to a 4-week course focused on the role of FABMs for women’s health. In addition, we integrated live case studies facilitated by leading experts in the field of restorative reproductive medicine (RRM), which seeks to identify and correct underlying causes and factors contributing to infertility and reproductive dysfunction. 4, 24 To further enhance the students’ clinical experiences, we coordinated online clinical observations with fertility educators and telemedicine visits with clinicians trained in FABMs.
Aims
This study aimed to assess the impact that an online elective had on the students’ knowledge, confidence in explaining, and anticipated behaviors in future practice according to Kirkpatrick Levels 2 and 3. The study hypothesized that an elective about FABMs for family planning and women’s health would:
-
Improve knowledge of FABMs (Kirkpatrick Level 2);
-
Improve confidence in explaining and offering FABMs (Kirkpatrick Level 3); and
-
Impact the students’ anticipated behaviors in future practice (Kirkpatrick Level 3).
For this study, we used a pre–post cohort design examining the effectiveness of an online elective, entitled “FABMs for Family Planning and Women’s Health.” The 4-week online elective, delivered via Learn Dash (StellarWP), was divided into two equal 2-week parts. Part A covered the application of FABMs for family planning. Part B included the scientific foundation for FABMs and covered the clinical applications of FABMs for reproductive and gynecologic health (see Appendix A for specific topics). Each part consisted of three synchronous and 12 asynchronous lectures, four live case study discussions, and three to five online clinical observations with FABM educators and clinicians. In addition to the two course directors, 22 faculty members gave prerecorded presentations, and a pool of 24 faculty members gave live presentations and/or led case studies. Students had the option to enroll in one or both parts of the elective. Enrolled students were included in the study if they consented to participate and completed both pre- and postelective surveys, without any further exclusion criteria. From August 2020 to May 2023, 571 students enrolled in the elective from 103 different schools, with an average of 21 students per session. A total of 553 students consented to participate; 500 students completed at least one survey; and 462 completed all the assessments. This study received Institutional Review Board exemption through Georgetown University.
Study participants completed a baseline questionnaire via an online survey describing their interest in the elective, previous knowledge, and familiarity with FABMs. Demographic information, including sex, age, desired medical specialty, type of medical training program, relationship status, religion, and reasons for enrollment in the course, was collected. Study instruments included two pre–post elective surveys. The first survey included 25 questions to evaluate the participants’ knowledge. The second survey included nine questions to assess participants’ anticipated behavioral changes and level of confidence offering FABMs in their clinical practice. Participants were asked to rank their level of confidence on a scale ranging from 1 to 5 (1=no confidence, 5=complete confidence). Participants were asked to rate their likelihood of offering FABMs to manage different aspects of family planning and women’s health on a scale of 1 to 5 (1=not at all likely, 5=almost certainly). We performed data analysis using Stata for Windows version 15.1 (StataCorp). We used paired t tests and the Wilcoxon signed rank test to test the hypotheses. A P value of <.05 was considered statistically significant.
During the study time period, 571 total students enrolled in and completed the elective. A total of 533 (93%) consented to participate, and 500 (88%) completed one of the two surveys. A total of 462 students completed both surveys (response rate=81%). All students who completed the surveys were included in the assessment of knowledge gained from the course—a total of 863 exams (428 for Part A and 435 for Part B). Because students could enroll in both parts of the elective, some completed both exams.
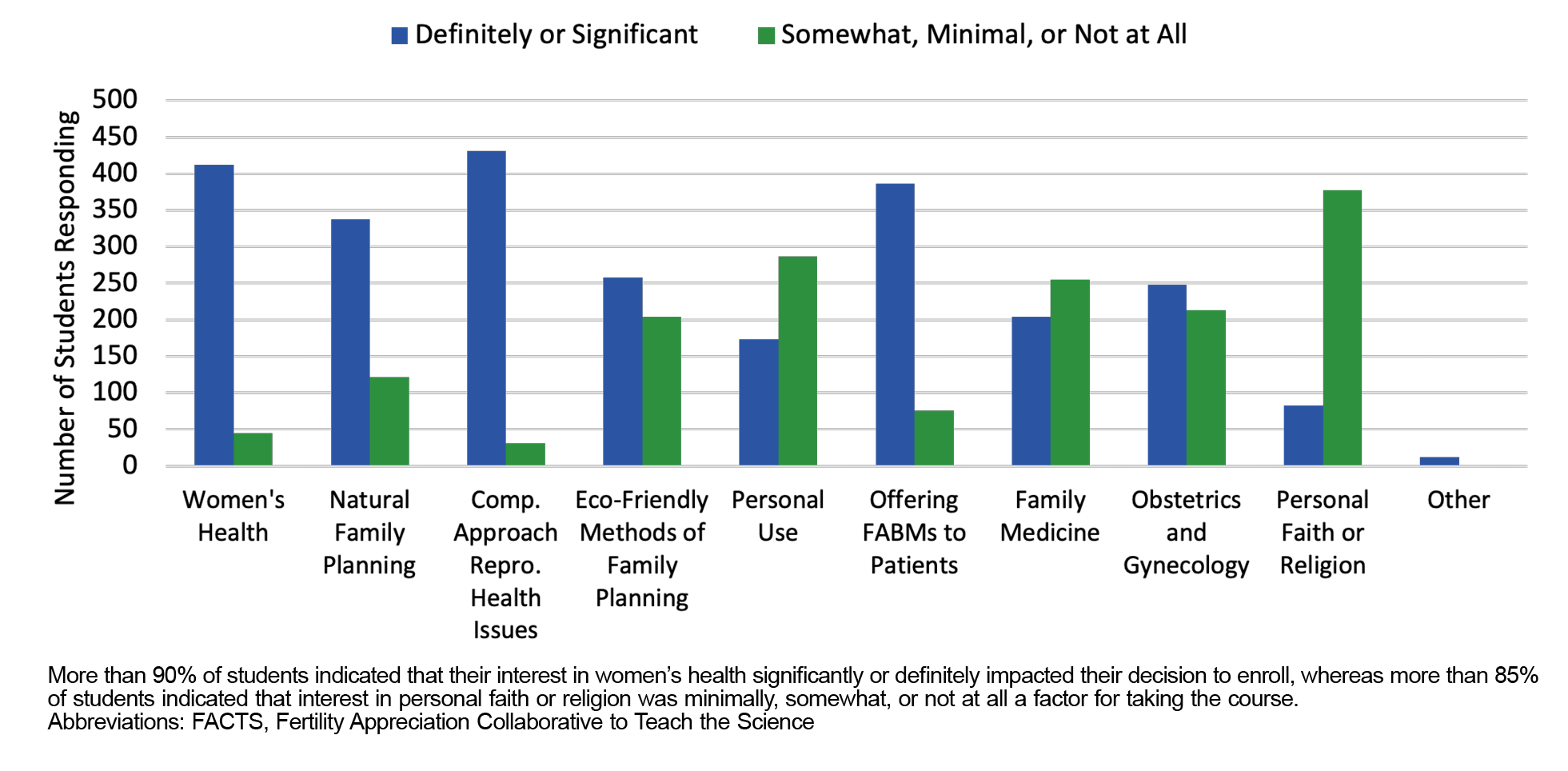
Of the 462 study participants, the majority were female (85%), single (70%), and age 26 to 30 (73%). Additionally, 24% identified as Catholic, 26% were Christian, 27% reported no religious affiliation, and 32% identified with another religion. Two-thirds of the participants were enrolled in a DO program, and 33% planned to pursue family medicine as a specialty (Table 1). When asked to provide their motivation for enrolling in the elective, 90% responded that their interest in women’s health either significantly or definitely impacted their decision to enroll, and 93% indicated that their motivation was due to their interest in a comprehensive approach to reproductive health issues (Figure 1). Overall, 18% of study participants indicated that their interest in the course was due to personal faith or religious reasons.
|
Demographics |
n (%) |
|
Sex |
|
|
Male |
67 (15) |
|
Female |
394 (85) |
|
Prefer not to say |
1 (0) |
|
Age (years) |
|
|
18–25 |
76 (16) |
|
26–30 |
336 (73) |
|
31–35 |
35 (8) |
|
36+ |
15 (3) |
|
Degree anticipated* |
|
|
MD |
139 (68) |
|
DO |
312 (30) |
|
Nursing |
1 (0) |
|
Other |
9 (2) |
|
Marital status* |
|
|
Married |
138 (30) |
|
Not Married |
323 (70) |
|
Religion** |
|
|
Catholic |
112 (24) |
|
Christian |
120 (26) |
|
No religion |
123 (27) |
|
Other religion |
148 (32) |
|
Specialty |
|
|
Pediatrics |
48 (10) |
|
Anesthesia |
11 (2) |
|
Family medicine |
151 (33) |
|
OB/GYN |
144 (31) |
|
Internal medicine |
30 (7) |
|
Psychiatry |
27 (6) |
|
Other |
50 (11) |
*N=461.
**Students were allowed to select more than one option, so the count is greater than N=462.
Abbreviation: OB/GYN, obstetrics/gynecology
Knowledge Scores
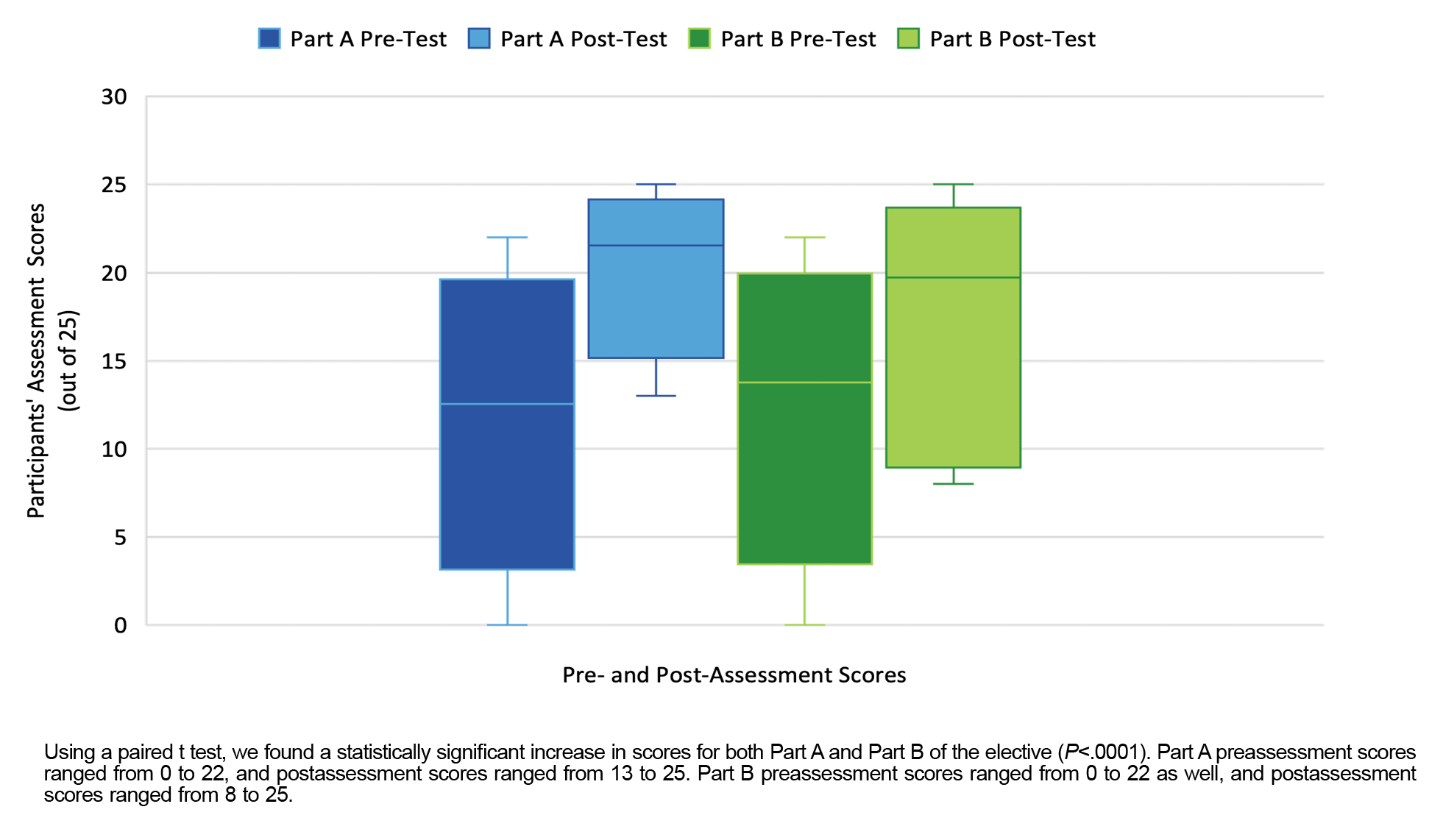
The elective had a statistically significant effect on knowledge scores (Figure 2). The Part A pre-elective mean score was 12.54 and the postelective mean was 21.56. Mean scores increased by 9.02 (t[427]=54.26, P<.0001). The Part B pre-elective mean score was 13.76, and the postcourse mean was 19.71, yielding a statistically significant difference of 5.95 (t[434]=37.83, P<.0001). In Part A, 99.77% of students experienced at least a 1-point increase in their score. In Part B, 97.01% had at least a 1-point increase.
Using a paired t test, we found a statistically significant increase in scores for both Part A and Part B of the elective (P<.0001). Part A preassessment scores ranged from 0 to 22, and postassessment scores ranged from 13 to 25. Part B preassessment scores ranged from 0 to 22 as well, and postassessment scores ranged from 8 to 25.
Confidence Level
The elective had a statistically significant positive effect on participants’ level of confidence offering FABMs in their clinical practice. Prior to the elective, participants’ mean confidence level was between no confidence and moderate confidence. After the elective, participants were significantly more confident in offering FABMs to patients for avoiding pregnancy, achieving pregnancy, monitoring reproductive health, and addressing women’s health issues.
The Wilcoxon signed rank test showed statistically significant improvements in each question (P<.0001). The most significant change was for monitoring reproductive health (mean=2.32, z=17.96, P<.0001), and the lowest was for achieve pregnancy (mean=2.22, z=17.84, P<.0001). Responses to the other questions, avoid pregnancy and address reproductive health concerns, also were significantly improved (mean=2.24, z=17.87 and mean=2.36, z=17.90, respectively; P<.0001).
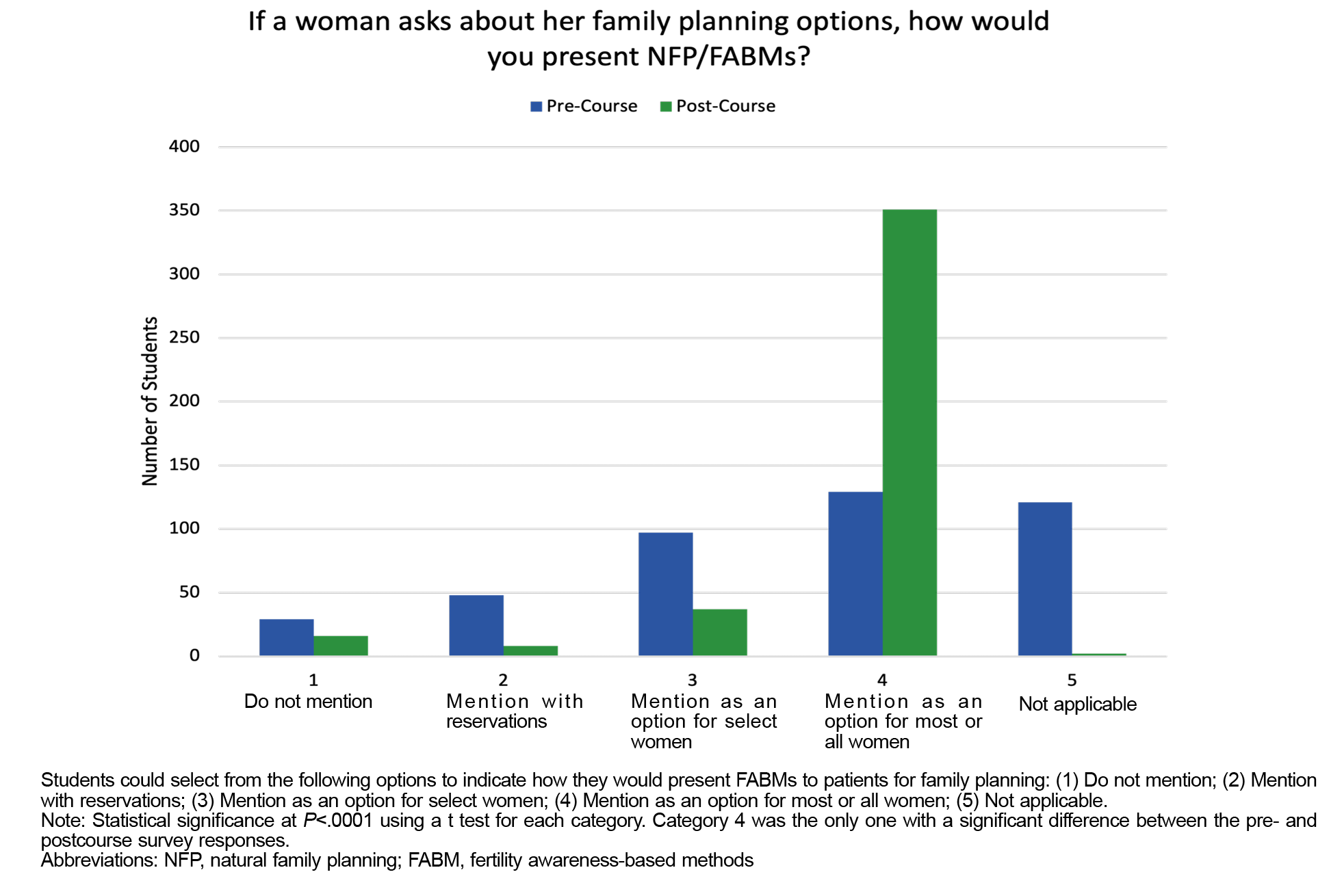
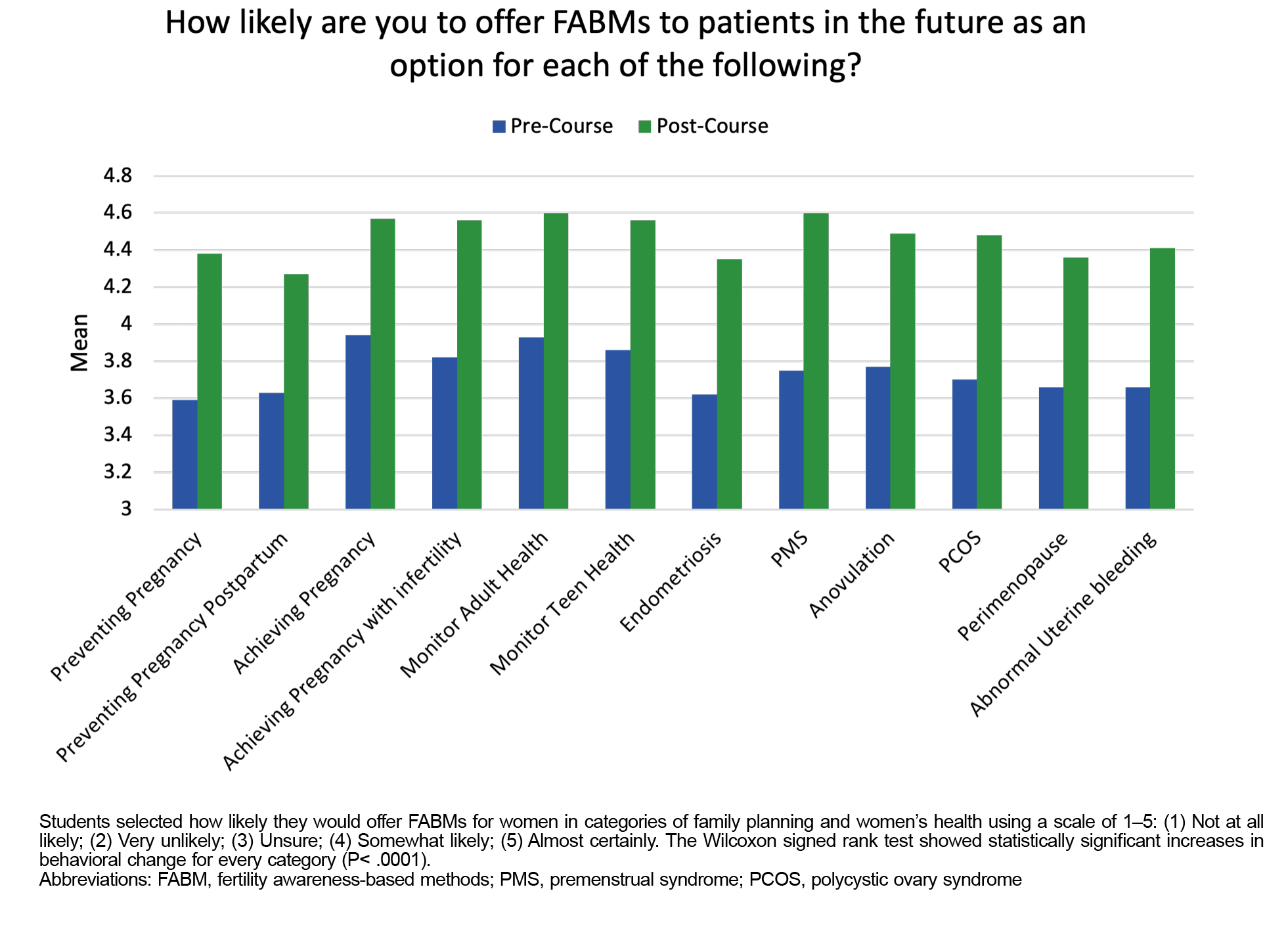
Behavioral Change
At the completion of the elective, on average, participants indicated that they would be more likely to offer FABMs as an option for women’s health issues, reproductive health monitoring, and family planning to their future patients. The majority of students (76%) reported that they would mention FABMs as an option for most or all women (Figure 3). We also assessed how likely students would be to offer FABMs to manage different aspects of family planning and reproductive or hormonal women’s health (Figure 4). A Wilcoxon signed rank test revealed that all categories were statistically significant, with the preventing pregnancy and polycystic ovary syndrome categories yielding the most significant change (z=11.06 and z=10.67, respectively; P<.0001). Using FABMs to treat premenstrual syndrome had the largest postelective mean value at 4.6, and using FABMs to avoid pregnancy in the postpartum period was the lowest value at 4.27. On average, students’ anticipated behavior indicated that they were at least somewhat likely to offer FABMs for family planning, monitoring reproductive health, and treating hormonal health conditions (Figure 4).
The results of this study demonstrate that a 2-week online elective significantly increases participants’ knowledge of FABMs, their confidence in explaining and offering these methods to patients, and their likelihood of offering FABMs to address women’s family planning and health care needs in their clinical practice. Our findings are consistent with a 2017 study in which Danis et al assessed the impact of a brief educational intervention on third-year medical students’ knowledge of FABMs and their confidence in using that knowledge.25 In that study, two lectures about FABMs and their clinical applications were given during the obstetrics and gynecology rotation, and the researchers concluded that brief and focused education can increase medical students’ knowledge of and confidence with FABMs. The results of these studies can be used to advocate for the incorporation of FABM education into medical school curricula.
The written feedback collected at the conclusion of the elective highlighted students’ appreciation and enthusiasm. One student remarked, “This course has opened my eyes to basic reproductive health facts that I have never been exposed to as a female and as a medical student, and I will be forever grateful.” Not only had she not learned about the female reproductive system earlier in life, but also her medical school curriculum did not afford her the opportunity to master the fundamentals of biological female health. Several other students reported similar experiences with this gap in medical education. Another student reflected, “I would never have known about or felt comfortable addressing fertility awareness with only what I had learned in medical school.”
In addition to improved knowledge, students expressed growth in their confidence discussing FABMs. Ultimately, this confidence gives way to actual physician behavior changes and interactions with patients. An elective participant commented, “It was great learning more about female cycles and how to effectively track at home. I’m positive I will use this information with future patients.” Many comments like this highlighted the impact the online elective had on future physician behavior and underscored the relevance of expanding educational opportunities about FABMs for medical school students and residents.
At the conclusion of our course, we elicited student feedback on how the course could be improved. Students requested standardized presentation times for live lectures or case studies; therefore, these are now scheduled at 12 noon ET during week 1 and at 2pm ET in week 2. Students also voiced a desire for more interactive case studies; therefore, we developed a standardized protocol and orientation for our case study leaders, with the clear expectation of interacting with students via question and answer sessions and discussions regarding cycle charts. Furthermore, students felt that more diverse patient encounters would be beneficial, and accordingly, we expanded our pool of preceptors to include clinicians who care for adolescents, patients in the perimenopausal period, and men with fertility issues. Finally, students felt a need for more clinical observations and experiences; therefore, we expanded our reach to include multiple clinics that regularly practice restorative reproductive medicine.
The findings from this study highlight the importance of expanding education regarding FABMs for medical students and residents. Expanding education in this area will contribute to increasing the number of physicians who understand the science supporting FABMs and who feel confident enough in their knowledge to offer these methods to patients. An increase in the number of clinicians trained in FABMs will expand patient access to FABMs as an evidence-based option for family planning and as a way to address a wide range of reproductive and hormonal health issues such as infertility, endometriosis, and polycystic ovarian syndrome.
The FACTS elective course used in this study is a unique learning experience with presentations developed and delivered by leading experts in the field of FABMs and RRM throughout the world. Presentations may be difficult to replicate because relatively few clinicians have significant expertise in these methods. Additionally, live case study and clinical preceptor experiences depend on the established relationships with health care professionals and educators trained in FABMs and RRM. Other schools seeking to provide a similar course to their students may run into barriers because of these limitations.a
This study included only students who took the elective. Because it is not a required course, participants may have been highly motivated to learn the material covered. Accordingly, the results may not be generalizable to the entire medical student population. A strength of the study is the large sample size of students from more than 100 medical schools across the United States and the high response rate.
This study adds to the findings of previous research demonstrating that online electives are effective approaches in improving students’ knowledge of FABMs, confidence, and willingness to offer these methods. Because most medical schools offer limited instruction on FABMs, a significant knowledge gap currently exists. The FACTS elective addresses that knowledge gap by offering lectures about FABMs, their scientific foundation, their effectiveness for family planning, and their applications for women’s health. When medical students learn about FABMs and observe how they may be used in the clinical setting, they can then discuss them as options to aid in the care of women and provide more family planning options for patients. FABM-trained physicians can then work with their patients to provide more targeted diagnoses and restorative treatment of common gynecologic concerns.
aFACTS now offers the option to license the course content to those who are interested in creating a course using the already existing material.
Acknowledgments
We are grateful for the support and contribution of Sean McCann and Madeline Olson, who helped us complete various aspects of this project.
References
-
American College of Obstetricians and Gynecologists Committee Opinion No. 651. Menstruation in girls and adolescents: using the menstrual cycle as a vital sign. Obstet Gynecol. 2015;126(6):e143-e146. doi:10.1097/AOG.0000000000001215
-
American Academy of Pediatrics, Committee on Adolescence; American College of Obstetricians and Gynecologists, Committee on Adolescent Health Care. Menstruation in girls and adolescents: using the menstrual cycle as a vital sign. Pediatrics. 2006;118(5):2,245-2,250. doi:10.1542/peds.2006-2481
-
Vigil P, Lyon C, Flores B, Rioseco H, Serrano F. Ovulation, a sign of health. Linacre Q. 2017;84(4):343-355. doi:10.1080/00243639.2017.1394053
-
Duane M, Stanford JB, Porucznik CA, Vigil P. Fertility awareness-based methods for women’s health and family planning. Front Med (Lausanne). 2022;9:858977. doi:10.3389/fmed.2022.858977
-
Manhart MD, Duane M, Lind A, Sinai I, Golden-Tevald J. Fertility awareness-based methods of family planning: a review of effectiveness for avoiding pregnancy using SORT. Osteopathic Family Physician. 2013;5(1):2-8. doi:10.1016/j.osfp.2012.09.002
-
Hilgers T. The new women’s health science of NaProTECHNOLOGY. Archives of Perinatal Medicine. 2011;17(4):191-198.
-
Smith A. Fertility Awareness Based Methods (FABMs): Evaluating and Promoting Female Interest for Purposes of Health Monitoring and Family Planning. Master’s thesis. University of Arkansas; 2019. Accessed November 13, 2023. https://scholarworks.uark.edu/etd/3279
-
Leonard CJ, Chavira W, Coonrod DV, Hart KW, Bay RC. Survey of attitudes regarding natural family planning in an urban Hispanic population. Contraception. 2006;74(4):313-317. doi:10.1016/j.contraception.2006.05.075
-
Duane M, Contreras A, Jensen ET, White A. The performance of fertility awareness-based method apps marketed to avoid pregnancy. J Am Board Fam Med. 2016;29(4):508-511. doi:10.3122/jabfm.2016.04.160022
-
Fehring RJ. The future of professional education in natural family planning. J Obstet Gynecol Neonatal Nurs. 2004;33(1):34-43. doi:10.1177/0884217503258549
-
Beeman P. Natural family planning in education and practice: a narrative review of the literature. Linacre Q. 2010;77(4):399-414. doi:10.1179/002436310803888592
-
Duane M, Carson G, VanderKolk K, Adams E, Gordon L. An evaluation of US medical schools’ reproductive health and family planning curricula. Issues Law Med. 2022;37(2):117-128.
-
Duane M, Motley R, Manhart M. Physicians need more education about natural family planning. Am Fam Physician. 2013;88(3):158-159. Accessed November 13, 2023. https://www.aafp.org/pubs/afp/issues/2013/0801/p158.html
-
Stanford JB, Thurman PB, Lemaire JC. Physicians’ knowledge and practices regarding natural family planning. Obstet Gynecol. 1999;94(5 Pt 1):672-678. doi:10.1016/S0029-7844(99)00388-9
-
Miklavcic AY, Isaacs CR. Obstetric-gynecology resident education regarding barrier and over-the-counter contraceptives: a national study. J Womens Health. 2012;21(11):1,196-1,200. doi:10.1089/jwh.2012.3546
-
Hampton KD, Newton JM, Parker R, Mazza D. A qualitative study of the barriers and enablers to fertility-awareness education in general practice. J Adv Nurs. 2016;72(7):1,541-1,551. doi:10.1111/jan.12931
-
Choi J, Chan S, Wiebe E. Natural family planning: physicians’ knowledge, attitudes, and practice. J Obstet Gynaecol Can. 2010;32(7):673-678. doi:10.1016/S1701-2163(16)34571-6
-
Kudesia R, Chernyak E, McAvey B. Low fertility awareness in United States reproductive-aged women and medical trainees: creation and validation of the Fertility & Infertility Treatment Knowledge Score (FIT-KS). Fertil Steril. 2017;108(4):711-717. doi:10.1016/j.fertnstert.2017.07.1158
-
Kelly PJ, Witt J, McEvers K, et al. Clinician perceptions of providing natural family planning methods in Title X funded clinics. J Midwifery Womens Health. 2012;57(1):35-42. doi:10.1111/j.1542-2011.2011.00107.x
-
Solo J, Festin M. Provider bias in family planning services: a review of its meaning and manifestations. Glob Health Sci Pract. 2019;7(3):371-385. doi:10.9745/GHSP-D-19-00130
-
Duane M, Martinez V, Berry M, Manhart MD. Evaluation of a fertility awareness-based shared decision-making tool part 1: study design and impact on clinician knowledge. PEC Innov. 2022;1:100061. doi:10.1016/j.pecinn.2022.100061
-
Duane, M, Martinez V, Berry M, Gilpatrick S, Manhart MD. Evaluation of a fertility awareness-based shared decision-making tool part 2: Patient experiences. PEC Innov. 2023;2:100169. doi:10.1016/j.pecinn.2023.100169
-
Dehlendorf C, Levy K, Ruskin R, Steinauer J. Health care providers’ knowledge about contraceptive evidence: a barrier to quality family planning care? Contraception. 2010;81(4):292-298. doi:10.1016/j.contraception.2009.11.006
-
Stanford JB, Carpentier PA, Meier BL, Rollo M, Tingey B. Restorative reproductive medicine for infertility in two family medicine clinics in New England, an observational study. BMC Pregnancy Childbirth. 2021;21(1):495. doi:10.1186/s12884-021-03946-8
-
Danis PG, Kurz SA, Covert LM. Medical students’ knowledge of fertility awareness-based methods of family planning. Front Med (Lausanne). 2017;4:65. doi:10.3389/fmed.2017.00065
Lead Author
Marguerite Duane, MD, MHA, MSPH
Affiliations: Department of Family Medicine, Georgetown University, Washington, DC | College of Osteopathic Medicine, Duquesne University, Pittsburgh, PA
Co-Authors
Logan Waechtler, MPH, MPA - Department of Public Health, Utah Valley University, Orem, UT
Margaret May, BS - School of Osteopathic Medicine, University of the Incarnate Word, San Antonio, TX
Deepa Manda, MPH, BS - Kentucky College of Osteopathic Medicine, University of Pikeville, Pikeville, KY
Noah F. Gomez, MD - Department of Obstetrics and Gynecology, Sisters of Charity Hospital, Buffalo, NY
Theresa M. Stujenske, PhD, RN - School of Nursing, Duquesne University, Pittsburgh, PA
Corresponding Author
Marguerite Duane, MD, MHA, MSPH
Correspondence: Department of Family Medicine, Georgetown University, Washington, DC; College of Osteopathic Medicine, Duquesne University, Pittsburgh, PA
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.