Background and Objectives: We compared experiences of patients who reported usually being seen by a resident with those usually seen by a staff physician.
Methods: We analyzed responses to a patient experience survey distributed at 13 family medicine teaching practices affiliated with the University of Toronto between May and June 2020. We analyzed responses to seven questions pertaining to timely access, continuity, and patient-centeredness. We compared responses between two types of usual primary care clinicians and calculated odds ratios before and after adjustment for patient characteristics.
Results: We analyzed data from 6,545 unique surveys; 18.6% reported their usual clinician was a resident physician. Resident patients were more likely to be older, born outside of Canada, report a high school education or less, and report having difficulty making ends meet. Compared to patients of staff physicians, patients of resident physicians had lower odds of being able to see their preferred primary care clinician and lower odds of getting nonurgent care in a reasonable time. They also had lower odds of reporting patient-centered care, but we found no significant differences in whether the time for an urgent appointment was about right or whether accessing care after hours was easy.
Conclusions: In our setting, patients who reported usually seeing resident physicians had worse continuity of care and timeliness for nonurgent care than patients who reported usually seeing staff physicians despite resident patients being older, sicker, and having a lower socioeconomic position. Postgraduate training programs need to test models to support access and continuity for resident patient panels.
Continuity and patient-centered care are central to family medicine postgraduate training programs. Relational continuity—seeing the same clinician over time—has been shown to be associated with better adherence to recommended care guidelines,1-3 better health outcomes,4-6 lower health service use,7-13 lower costs,12, 14, 15 and even lower mortality.16, 17 To model time in practice and to increase patient-clinician continuity, some residency programs encourage residents to build their own patient panels. This approach allows patients to book directly with resident physicians in addition to their primary staff physician and helps residents gain experience in long-term management of patients.
While resident physicians often are viewed favorably by patients,18, 19 studies have found that resident physicians have lower continuity with patients compared to staff physicians; this finding usually is attributed to scheduling and resident requirements to attend to off-service rotations such as general surgery or internal medicine.20 Time in clinic, panel size, and feeling of ownership are factors that have been associated with resident-patient continuity.20, 21 A recent scoping review found that interventions to improve continuity have had mixed effects, but outcomes were largely measured through administrative data and not from a patient perspective. 21
Few studies have examined patients’ experience of care, including dimensions of timely access and continuity, when a resident is most responsible for their primary care. Studies that have assessed the effects of innovations in academic clinic structure on access and continuity often did not use patient-reported measures or did not stratify responses by level of training of the primary care clinician. 22- 25
We conducted a subanalysis of responses to a common patient experience survey done in 2020 at multiple teaching sites affiliated with a large Canadian family medicine residency program. All patients at the teaching clinics are enrolled to staff physicians. A subset of staff physician patients are selected to be followed by resident physicians during their standard 2-year training period. These patients are selected by residents and/or staff physicians based on learning needs, complexity, and comorbidities, and with the patients’ permission. In our setting, residents typically empanel approximately 150 patients. Clerical staff try to preferentially book resident patients with resident physicians, although patients can choose to book an appointment with their staff physician instead.
We analyzed patient experience data to understand differences in timely access, continuity, and patient-centeredness between patients who reported usually seeing a resident versus a staff physician as their primary care clinician.
Context and Setting
We analyzed results from a cross-sectional patient survey distributed at 13 academic family medicine teaching clinics associated with the University of Toronto between May 2020 and June 2020. The University of Toronto has the largest family medicine residency program in North America, training approximately 320 residents in any given year. Clinics range in size, serving between 14,000 and 50,000 patients. Twelve of the 13 sites receive funding from the government for nonphysician health professionals, including nurses, nurse practitioners, social workers, and pharmacists who are part of the clinical team.
Almost all teaching clinics provide after-hours care on some evenings and weekends. At most sites, patients also can access care outside of clinic hours through an on-call phone line, which is usually run by family medicine residents. Urgent daytime appointments may be triaged at some sites by nursing staff at the clinic, and same- or next-day appointments are given to those who require urgent medical attention. During the study period, both in-person and phone appointments were offered.
At all times, to maintain patient continuity, family medicine residents are scheduled for a minimum of one half day per week of clinic. On average, most have 3 months per year when they are scheduled in clinic more intensively for 4 days per week, although some residents spread out their family medicine clinics more evenly through the year. The remaining clinical time is scheduled for off-service rotations such as general surgery or internal medicine.
Residents are paid by salary. Staff physicians working at the teaching clinic are paid largely by capitation with some fee-for-service payments, financial incentives for preventive and chronic condition care, and stipends.
Study Population and Recruitment
Surveys were conducted from May to June 2020 for the purposes of quality improvement. Every quarter, sites email a link to an online patient experience survey to patients with a valid email address on file; sampling each quarter is based on birth month, with all eligible patients receiving a survey in a given year. This subanalysis includes the results of the survey sent to patients whose birthdays fall in March, April, or May. The survey was hosted on Qualtrics (Qualtrics LLC), a secure web-based survey system. One reminder email was sent 2 weeks after the initial invitation to complete the survey. All responses were anonymized. Patients were not provided any incentives, and participation was voluntary. In some cases where patients could not complete the survey themselves, caregivers were allowed to complete it on the patients’ behalf. Surveys were conducted in English, except for one site also conducting the survey in French.
Study Design and Survey
Details on survey development can be found elsewhere.26 The survey included questions in the following domains: (a) seeking and delaying care during the pandemic, (b) use and comfort with virtual care, (c) timely access and continuity, (d) patient centeredness, and (e) patient demographics and contextual factors (Supplemental Appendix A). In the last section, patients reported on the question “Which primary care provider do you usually see?” with answers including staff physician, resident physician, nurse practitioner, or unsure. Survey data was stored on a secure server at the University of Toronto, and all potential identifiable information was removed by a script, including (a) IP addresses, (b) email addresses, (c) longitude/latitude coordinates, and (d) any free text fields that may contain unsolicited protected health information. In our subanalysis, the primary exposure was the type of primary care clinician usually seen. Outcome measures were the dichotomized responses to questions 16, 18, 20, and 22–25 of the original 54-question survey conducted in 2020. These questions related to timely access (for urgent issues and regular appointments), continuity, and patient-centeredness (Supplemental Appendix B).
Research Ethics
Our initiative was formally reviewed by institutional authorities at Unity Health Toronto and deemed to neither require Research Ethics Board approval nor written informed consent from participants.
Analysis
All surveys completed in English with at least one answered question and a completed response regarding the level of training of their usual primary care clinician were included in statistical analysis. We compared the demographic characteristics and then stratified outcome measures by type of usual primary care clinician. We built separate logistic regression models for each outcome measure to compare the odds of a positive experience by clinician type, both before and after adjustment for patient demographics that we hypothesized a piori were potential confounders (age, gender, education level, trouble making ends meet, whether born in Canada, preferred language, and self-rated health). We do not report on the nurse practitioner data due to low patient volumes. All data analysis was performed in R version 4.0 (R Foundation).
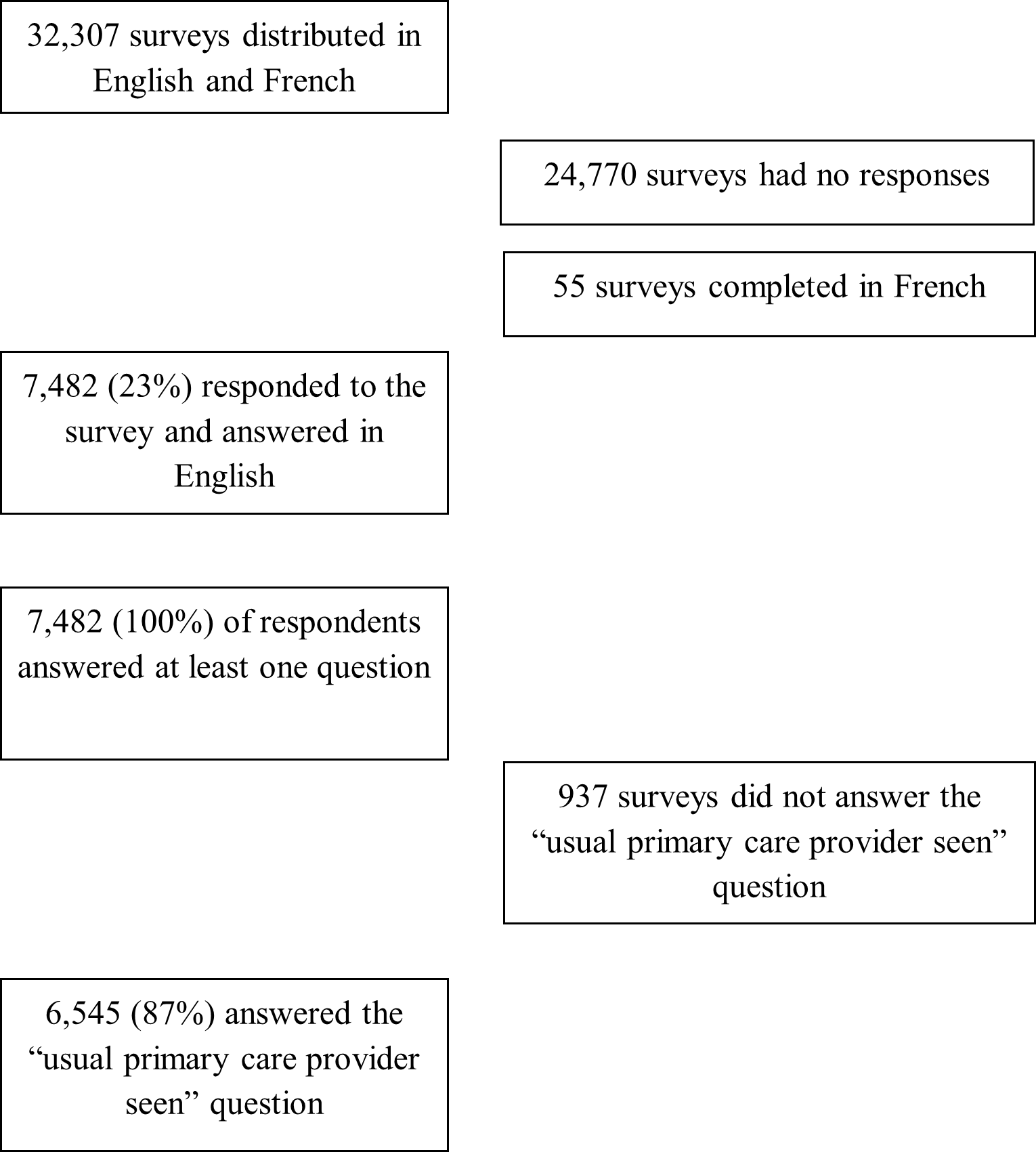
A total of 32,307 surveys were distributed via email to patients at 13 teaching sites. We analyzed data for 6,545 surveys (Figure 1). Seventy-four percent (n=4,842) of included respondents reported that their usual primary care clinician was a staff physician, 18.6% (n=1,217) a resident physician, 2.6% (n=173) a nurse practitioner, and 4.8% (n=313) were unsure (Supplemental Appendix C). Compared to patients of staff physicians, more patients of resident physicians reported being men (31.6% vs 38.3%), over age 65 (34.3% vs 39.4%), not being born in Canada (26.8% vs 34.0%), having high-school or less education (19.7% vs 26.8%), having difficulty making ends meet (8.5% vs 10.0%), and having fair or poor health (13.7% vs 18.2%; Table 1).
Compared to patients of staff physicians, patients of residents had lower odds of reporting getting an urgent appointment the same or next day when they needed care; however, the differences between groups were not significant after adjustment for patient demographics (68.6% vs 57.0%; UOR 0.61, 95% CI 0.41 to 0.91; AOR 0.71, 95% CI 0.46 to 1.12; Table 2). We found no significant differences in the proportion of resident and staff patients reporting that the length of time between booking and their appointment was just right (77.0% vs 73.4%; UOR 0.83, 95% CI 0.53 to 1.30; AOR 1.10, 95% CI 0.67 to 1.87), or with resident and staff physician patients reporting that booking an urgent appointment in the evenings or weekends was very or somewhat easy (46.4% vs 52.8%; UOR 1.29, 95% CI 0.63 to 2.68; AOR 1.09, 95% CI 0.47 to 2.52).
|
Demographic characteristic
|
Patients reporting being seen by staff physicians (n=4,842) n (%)
|
Patients reporting being seen by resident physicians (n=1,217) n (%)
|
P value
|
|
|
|
|
|
Age (n=6,509)
|
0 to 17 years old
|
217 (4.5)
|
75 (6.2)
|
<.001
|
|
18 to 24 years old
|
75 (1.6)
|
17 (1.4)
|
|
|
25 to 34 years old
|
336 (7.0)
|
95 (7.9)
|
|
|
35 to 49 years old
|
994 (20.6)
|
248 (20.5)
|
|
|
50 to 64 years old
|
1,545 (32.1)
|
298 (24.7)
|
|
|
>65 years old
|
1,654 (34.3)
|
476 (39.4)
|
|
|
|
|
|
|
|
Gender (n=6,488)
|
Woman
|
3,229 (67.2)
|
719 (59.7)
|
<.001
|
|
Man
|
1,520 (31.6)
|
462 (38.3)
|
|
|
Other or prefer not to answer
|
56 (1.2)
|
24 (2.0)
|
|
|
|
|
|
|
|
Education level (n=6,380)
|
High school or less
|
932 (19.7)
|
314 (26.8)
|
<.001
|
|
College/university
|
2,330 (49.2)
|
559 (47.6)
|
|
|
Graduate/professional
|
1,473 (31.1)
|
301 (25.6)
|
|
|
|
|
|
|
|
Trouble making ends meet (n=6,357)
|
Yes
|
399 (8.5)
|
117 (10.0)
|
<.001
|
|
No
|
3,850 (81.6)
|
885 (75.6)
|
|
|
Prefer not to answer
|
471 (10.0)
|
168 (14.4)
|
|
|
|
|
|
|
|
Born in Canada (n = 6,437)
|
Yes
|
3,490 (73.2)
|
790 (66.0)
|
<.001
|
|
No
|
1,275 (26.8)
|
407 (34.0)
|
|
|
|
|
|
|
|
Preferred language (n = 6,490)
|
English
|
4,745 (98.8)
|
1,184 (98.3)
|
.33
|
|
Non-English
|
60 (1.3)
|
20 (1.7)
|
|
|
|
|
|
|
|
Self-rated health (n = 6,487)
|
Excellent or very good health
|
2,701 (56.2)
|
581 (48.4)
|
<.001
|
|
Good health
|
1,446 (30.1)
|
401 (33.4)
|
|
|
Fair or poor health
|
658 (13.7)
|
218 (18.2)
|
|
|
Question (affirmative response)
|
Usual primary care clinician seen
|
Affirmative responses, n (%)
|
Unadjusted OR (95% CI)
|
Adjusted OR (95% CI)
|
|
How many days did it take from when you first tried to book an appointment at our clinic to when you received care? (same day or next day)
|
Staff physician
|
358 (68.6)
|
|
|
|
Resident physician
|
69 (57.0)
|
0.61 (0.41 to 0.91) *
|
0.71 (0.46 to 1.12)
|
|
How would you describe the length of time it took between making the appointment and receiving care? (about right)
|
Staff physician
|
418 (77.0)
|
|
|
|
Resident physician
|
91 (73.4)
|
0.83 (0.53 to 1.30)
|
1.10 (0.67 to 1.87)
|
|
How easy or difficult was it to get urgent care from clinic on an evening, weekend, or holiday during the COVID-19 pandemic? (very easy or somewhat easy)
|
Staff physician
|
77 (46.4)
|
|
|
|
Resident physician
|
19 (52.8)
|
1.29 (0.63 to 2.68)
|
1.09 (0.47 to 2.52)
|
|
How often did you receive care from the doctor or nurse practitioner that you prefer? (always or usually)
|
Staff physician
|
2,619 (82.6)
|
|
|
|
Resident physician
|
539 (71.5)
|
0.53 (0.44 to 0.64) *
|
0.53 (0.44 to 0.65) *
|
|
How often did you receive care within a reasonable time from your doctor or nurse practitioner? (always or usually)
|
Staff physician
|
2,917 (90.1)
|
|
|
|
Resident physician
|
703 (85.3)
|
0.64 (0.51 to 0.81) *
|
0.70 (0.55 to 0.90) *
|
|
When you received care from your doctor or nurse practitioner, how often did they involve you as much as you want to be in decisions about your care and treatment? (always or usually)
|
Staff physician
|
3,106 (95.9)
|
|
|
|
Resident physician
|
769 (93.3)
|
0.60 (0.44 to 0.83) *
|
0.68 (0.48 to 0.97) *
|
|
When you received care from your doctor or nurse practitioner, how often did they spend enough time with you? (always or usually)
|
Staff physician
|
3,093 (95.5)
|
|
|
|
Resident physician
|
762 (92.5)
|
0.58 (0.43 to 0.79) *
|
0.64 (0.46 to 0.90) *
|
Compared to patients of staff physicians, patients of residents had lower odds of reporting that they always or usually were able to receive care within a reasonable time for a nonurgent appointment (85.3% vs 90.1%; UOR 0.64, 95% CI 0.51 to 0.81; AOR 0.70, 95% CI 0.55 to 0.90) and had lower odds of reporting that they were always or usually able to see their preferred clinician (71.5% vs 82.6%; UOR 0.53, 95% CI 0.44 to 0.64; AOR 0.53, 95% CI 0.44 to 0.65), even after adjustment for patient demographics. As well, compared to patients of staff physicians, patients of residents had significantly lower odds of feeling involved in their medical decisions (93.3% vs 95.9%; UOR 0.60, 95% CI 0.44 to 0.83; AOR 0.68, 95% CI 0.48 to 0.97) and had significantly decreased odds of reporting spending enough time with their clinician (92.5% vs 95.5%; UOR 0.58, 95% CI 0.43 to 0.79; AOR 0.64, 95% CI 0.46 to 0.90).
Respondents who were unsure of their regular clinician indicated significantly lower adjusted odds of affirmative responses in all questions that did not pertain to urgent care (Supplemental Appendix D).
We compared the care experience between patients of resident and staff physicians at 13 teaching clinics associated with the largest family medicine residency training program in North America. We found that patients who reported usually seeing a resident physician had lower odds of reporting timely care for nonurgent concerns and seeing their preferred clinician compared to patients who reported usually seeing a staff physician.
Others have analyzed visit data and also found lower continuity among resident versus staff physicians.20, 21 A survey of Quebec family medicine residents noted “decreased time in clinic” and “scheduling” as barriers to maintaining relational continuity.20 These barriers relate, in large part, to residents being away from clinic during off-service rotations (ie, training rotations other than family medicine). Other studies also have suggested that the complexities of resident schedules at academic teaching sites influence timeliness and continuity for patients. For example, a study of US family medicine clinics showed significantly decreased access among academic teaching sites compared to community clinics. 27 In our study, lower odds of seeing their preferred clinician also may relate to patients who usually see a resident preferring to see their staff physician.
Various solutions have been proposed to increase continuity and access for patients of resident physicians, including the use of an open-scheduling policy to allow for same-day bookings or a system where two residents empanel the same patients to increase the likelihood of seeing at least one of their regular clinicians.28 Using the electronic medical record to document resident patient panels, engaging the reception staff, redesigning appointment schedules, using appointment cards for residents, and collecting midrotation feedback are also practical strategies that have been suggested to increase continuity.29 Augmenting availability for walk-in or same-day appointments can increase timely access at academic centers but does not necessarily increase relational continuity with the same resident.30 Despite the plethora of promising strategies, a scoping review noted that the impact of interventions to improve continuity of care in residency teaching clinics has been mixed, and more research is needed to identify successful models. 21
We did not find significant differences between patients of resident versus staff physicians for timely access to urgent care and ease of after-hours care. We hypothesize that these findings relate to practice policies at many of our teaching clinics that prioritize access for urgent issues. For example, many practices have policies to support triage of urgent calls, directing them to a covering nurse or doctor if the patient’s usual clinician is away. We found patients of resident physicians had lower odds of feeling involved in medical decisions and spending enough time with their clinician, although differences were small. We hypothesize that this finding may reflect residents’ developing time management and shared decision-making skills, because typical resident patient appointments (15-30 min) are the same or longer than for staff physicians (15 min).
Notably, we found resident patients were more likely to be older, born outside of Canada, report a high school education or less, report having difficulty making ends meet, and report poor or fair health. Why these differences exist is unclear, but potential reasons include deliberate selection of patients related to learning value, staff physicians trying to accommodate more at-need patients despite already full panels, or more marginalized patients being less likely to advocate for care from staff physicians.
We found that nearly 5% of respondents were unsure of who their primary clinician was; even when adjusting for demographic differences, this group of patients was less likely to report timeliness or care continuity. More research is needed to understand why they are unsure and how this affects care.
Strengths and Limitations
We examined differences in access and continuity between patients who reported usually seeing resident versus staff physicians. Using a patient lens, we analyzed data from more than 6,500 patients who responded to a common patient experience survey. We examined seven patient experience outcomes and adjusted our analysis for various sociodemographic factors. However, several factors may limit external generalizability. The survey was done in the first few months of the pandemic. All practices were affiliated with the University of Toronto; most were team-based practices, and all had physicians paid via blended capitation. As well, response bias is a risk. The response rate was 23%, the survey was distributed in English and French to those with an email address, and some who received the survey chose not to respond; unfortunately, we do not have demographic data for nonresponders. Further, patients who were more engaged in care or could more easily recall their experiences may have been more likely to respond. We could not control for inherent differences between patients who agree to resident empanelment versus those who maintain only a staff physician as their usual primary care clinician. We did not have information in the survey about year of training, so we could not explore that factor. Finally, resident patients are coempaneled to both residents and staff, and patients of resident physicians may have been commenting on staff physician care in their responses, including how frequently they saw their preferred clinician.
We found that patients who reported usually seeing a resident versus staff physician had lower odds of reporting timely access for nonurgent concerns and relational continuity with their preferred clinician. Resident patients also were sicker and had lower socioeconomic position. Further research could link survey data with electronic medical record data to correlate different measures of continuity. More research is also needed to understand why patients with higher care needs are disproportionately served by residents who, on average, seem not able to provide the same degree of timely access and continuity, in part because of the demands of residency training that require them to be outside of the clinic. Ultimately, more innovation and research are needed to understand what postgraduate program structures and primary care practice policies optimize patient experience, care and outcomes alongside resident training outcomes and practice intentions.
Dr Kiran is the Fidani Chair of Improvement and Innovation in Family Medicine at the University of Toronto and is supported as a Clinician Scientist by the Department of Family and Community Medicine (DFCM) at the University of Toronto and at St. Michael’s Hospital. Funds from the Fidani Chair supported Dr Agarwal as the Patient Experience Measurement Lead for the DFCM.
TK conceived of the study, and SD and TK designed it. RW conducted the analysis. All authors helped interpret the data. SD and TK drafted the manuscript, and all authors critically reviewed it. All authors read and approved the final manuscript.
Acknowledgments
We thank Frances Cousins, Tiffany Florindo, Navsheer Gill, Susie Kim, Joanne Laine-Gossin, Thuy-Nga Pham, Noor Ramji, Jennifer Stulberg, Sam Tirkos, and Gina Yip for their support in developing and implementing the survey at their respective teaching practices; Trish O’Brien for supporting the survey implementation across all sites; the patient partners who helped us refine the survey questions; and Erin Plenert for her comments on the manuscript.
References
-
Dossa AR, Moisan J, Guénette L, Lauzier S, Grégoire JP. Association between interpersonal continuity of care and medication adherence in type 2 diabetes: an observational cohort study.
CMAJ Open. 2017;5(2):E359-E364.
doi:10.9778/cmajo.20160063
-
Warren JR, Falster MO, Tran B, Jorm L. Association of continuity of primary care and statin adherence.
PLOS ONE. 2015;10(10):e0140008.
doi:10.1371/journal.pone.0140008
-
Hong JS, Kang HC, Kim J. Continuity of care for elderly patients with diabetes mellitus, hypertension, asthma, and chronic obstructive pulmonary disease in Korea.
J Korean Med Sci. 2010;25(9):1,259-1,271.
doi:10.3346/jkms.2010.25.9.1259
-
-
van Walraven C, Oake N, Jennings A, Forster AJ. The association between continuity of care and outcomes: a systematic and critical review.
J Eval Clin Pract. 2010;16(5):947-956.
doi:10.1111/j.1365-2753.2009.01235.x
-
Chen HM, Tu YH, Chen CM. Effect of continuity of care on quality of life in older adults with chronic diseases: a meta-analysis.
Clin Nurs Res. 2017;26(3):266-284.
doi:10.1177/1054773815625467
-
Cunningham C, Patil T, Shahid R, Patel A, Oddie S. Patient–physician relational continuity and health system utilization among patients in Alberta.
Healthc Q. 2020;22(4):13-21.
doi:10.12927/hcq.2020.26089
-
Tammes P, Purdy S, Salisbury C, MacKichan F, Lasserson D, Morris RW. Continuity of primary care and emergency hospital admissions among older patients in England.
Ann Fam Med. 2017;15(6):515-522.
doi:10.1370/afm.2136
-
Huntley A, Lasserson D, Wye L, et al. Which features of primary care affect unscheduled secondary care use? A systematic review.
BMJ Open. 2014;4(5):e004746.
doi:10.1136/bmjopen-2013-004746
-
Kohnke H, Zielinski A. Association between continuity of care in Swedish primary care and emergency services utilisation: a population-based cross-sectional study.
Scand J Prim Health Care. 2017;35(2):113-119.
doi:10.1080/02813432.2017.1333303
-
Barker I, Steventon A, Deeny SR. Association between continuity of care in general practice and hospital admissions for ambulatory care sensitive conditions: cross sectional study of routinely collected, person level data.
BMJ. 2017:356:j84.
doi:10.1136/bmj.j84
-
Bazemore A, Petterson S, Peterson LE, Bruno R, Chung Y, Phillips RL Jr. Higher primary care physician continuity is associated with lower costs and hospitalizations.
Ann Fam Med. 2018;16(6):492-497.
doi:10.1370/afm.2308
-
van Loenen T, van den Berg MJ, Westert GP, Faber MJ. Organizational aspects of primary care related to avoidable hospitalization: a systematic review.
Fam Pract. 2014;31(5):502-516.
doi:10.1093/fampra/cmu053
-
Amjad H, Carmichael D, Austin AM, Chang CH, Bynum JPW. Continuity of care and health care utilization in older adults with dementia in fee-for-service Medicare.
JAMA Intern Med. 2016;176(9):1,371-1,378.
doi:10.1001/jamainternmed.2016.3553
-
Sveréus S, Larsson K, Rehnberg C. Clinic continuity of care, clinical outcomes and direct costs for COPD in Sweden: a population based cohort study.
Eur Clin Respir J. 2017;4(1):1290193.
doi:10.1080/20018525.2017.1290193
-
Baker R, Freeman GK, Haggerty JL, Bankart MJ, Nockels KH. Primary medical care continuity and patient mortality: a systematic review.
Br J Gen Pract. 2020;70(698):e600-e611.
doi:10.3399/bjgp20X712289
-
Pereira Gray DJ, Sidaway-Lee K, White E, Thorne A, Evans PH. Continuity of care with doctors—a matter of life and death? A systematic review of continuity of care and mortality.
BMJ Open. 2018;8(6):e021161.
doi:10.1136/bmjopen-2017-021161
-
Malcolm CE, Wong KK, Elwood-Martin R. Patients’ perceptions and experiences of family medicine residents in the office. Can Fam Physician. 2008;54(4):570-1, 571.e1-6.
-
Nakar S, Levi D, Rosenberg R, Vinker S. Patient attitudes to being treated by junior residents in the community.
Patient Educ Couns. 2010;78(1):111-116.
doi:10.1016/j.pec.2009.05.017
-
Lee A, Kennett S, Khera S, Ross S. Perceptions, practice, and “ownership”: experiences in continuity of the patient-doctor relationship in a family medicine residency.
Can Med Educ J. 2017;8(4):e74-e85.
doi:10.36834/cmej.42288
-
Walker J, Payne B, Clemans-Taylor BL, Snyder ED. Continuity of care in resident outpatient clinics: a scoping review of the literature.
J Grad Med Educ. 2018;10(1):16-25.
doi:10.4300/JGME-D-17-00256.1
-
Paul KJ, Hidaka BH, Ford P, Morris C. Measuring greater patient-provider continuity in a clinic-first family medicine residency curriculum.
Perm J. 2021;25(3):20.290.
doi:10.7812/TPP/20.290
-
Adam P, Hersch D, Peek CJ. Implementing clinic first guiding actions across 4 family medicine residency clinics.
Acad Med. 2022;97(2):233-238.
doi:10.1097/ACM.0000000000004180
-
Zeller TA, Ewing JA, Asif IM. Prevalence of clinic first curricula: a survey of AFMRD members.
Fam Med. 2019;51(4):338-343.
doi:10.22454/FamMed.2019.666943
-
-
Agarwal P, Wang R, Meaney C, et al. Sociodemographic differences in patient experience with primary care during COVID-19: results from a cross-sectional survey in Ontario, Canada.
BMJ Open. 2022;12(5):e056868.
doi:10.1136/bmjopen-2021-056868
-
Carvajal DN, Blank AE, Lechuga C, Schechter C, McKee MD. Do primary care patient experiences vary by teaching versus nonteaching facility?
J Am Board Fam Med. 2014;27(2):239-248.
doi:10.3122/jabfm.2014.02.130222
-
Hudon C, Luc M, Beaulieu MC, et al. Implementing advanced access to primary care in an academic family medicine network: participatory action research. Can Fam Physician. 2019;65(9):641-647.
-
Schers H, van den Hoogen H, Grol R, van den Bosch W. Continuity of care through medical records—an explorative study on GPs’ management considerations.
Fam Pract. 2006;23(3):349-352.
doi:10.1093/fampra/cml002
-
Johnson BJ, Mold JW, Pontious JM. Reduction and management of no-shows by family medicine residency practice exemplars. Ann Fam Med. 2007;5(6):534-539. doi:10.1370/afm.752



There are no comments for this article.