Background and Objectives: Despite the widespread adoption of the holistic review initiative in medical school admissions, admissions committees continue to struggle with identifying applicant attributes that predict future practice location. This challenge has significant practical implications, particularly for institutions committed to addressing regional health care shortages.
Methods: We analyzed eight cohorts of applicants who matriculated between 2006 and 2013 and then completed residency. We used univariate and multiple regression models to identify applicant objective attributes linked to later in-state practice. Objective data available in applications included high school location, legal state of residence, Medical College Admissions Test (MCAT) scores, grade point average, college details, graduate school, race/ethnicity, and gender; these were compared by posttraining practice location.
Results: Of 509 graduates in practice, 212 (41.7%) were in-state. In-state graduates were older (P<.001), predominately underrepresented in medicine (42% vs 33%, P<.01), graduated from urban high schools (28% vs 18%, P<.05), attended in-state colleges (66% vs 55%, P<.05), and had lower MCAT scores (56th vs 67th percentile, P<.001). Regression analysis revealed that only age, urban high school, and MCAT score significantly contributed to the model (R 2=0.064, P=.004).
Conclusions: This study shows the limited value of applicant objective data to admissions committees in predicting future in-state practice. The findings emphasize the importance of a holistic admissions process and the value of considering subjective applicant data in efforts to predict future practice location. Additional research may help identify which subjective aspects of an applicant can assist admissions committees in this effort.
Medical school admissions committees commonly struggle to identify which applicants are most likely to practice in-state following training. This struggle is of particular interest for institutions committed to addressing regional health care shortages and for specialties that serve in areas of health care shortage, such as family medicine. Although research exists on predicting academic performance in medical school applicants using cognitive and noncognitive variables, 1-4 research concerning applicant variables affecting future practice location is sparse.
Studies have reported that residency training location is a stronger predictor than medical school of future practice location. 5-8 Reportedly, 52.9% of residents practice in the state of residency training. 9 Another study reported that ties to the state and primary care residency are associated with in-state practice. 10 Pipeline programs also play a role in shaping graduates’ career choices and increasing the likelihood of pursuing primary care or practicing in-state.11-13 One other study showed that rural origin and intent to practice in rural areas and/or family medicine were strongly correlated with rural practice, but did not address the question of in-state practice. 14
The University of New Mexico School of Medicine (UNM SOM) was established to address the critical shortage of medical care across the state and is strongly committed to admitting students from New Mexico. Through a holistic review process, the UNM SOM admissions committee considers objective data, personal attributes, goals, and experiences, aiming to assess the likelihood of an applicant’s future in-state practice and thereby advance the school’s mission.15 This holistic review process complements other UNM SOM programs similarly aimed at enhancing future in-state practice, such as pipeline programs aimed at groups underrepresented in medicine (URiM) and/or from rural backgrounds. 11, 13
This study evaluated whether objective applicant data (ie, academic, geographic, demographic, and educational) are associated with future in-state practice.
This study examined applicant objective data of eight medical student cohorts between 2006 and 2013 (N=617) that graduated between 2010 and 2017 and completed graduate medical education by the time of analysis. Individuals who withdrew from medical school (n=24) or residency (n=8) do not have a current medical license (n=5, including 2 deceased) and current students (n=2), residents (n=36) or fellows (n=33) were excluded. The final dataset consisted of 509 practicing physicians.
Data Sources
Applicant objective data included high school location (rural or urban), Medical College Admissions Test (MCAT) percentile, grade point average (GPA), college location, college major, graduate school concentration, race/ethnicity, and gender. In-state versus out-of-state practice locations were identified using public information from the Centers for Medicare & Medicaid Services National Plan and Provider Enumeration System National Provider Identifier registry, state medical boards, and additional online resources.
Data Analysis
Initial data analysis was done using χ2 for proportions or t test of means to compare practice groups (in-state vs out-of-state). Next, using variables for which a statistically significant difference in the univariate analysis existed, path modeling using multiple regression was performed.
Step 1: Univariate Group Comparison
Table 1 shows that of the 509 graduates, 212 (41.7%) practice in New Mexico. Average age at the time of application differed by 1 year, in-state practicing physicians being older (P<.001). One-hundred (47%) graduates practicing in New Mexico identified as URiM compared to 98 practicing out-of-state (33%, P<.01). In addition, graduation from a rural high school significantly differed as 40 (19%) practicing in-state attended rural high schools, while 83 (28%) practicing out-of-state attended rural high schools (P<.05). Attending a New Mexico institution of higher education (NMIHE) was more frequent for in-state practicing MD graduates: 140 (66%) versus 163 (55%) out-of-state, (P<.05). Finally, mean MCAT percentiles differed, in-state 56th percentile versus 67th percentile for out-of-state (P<.001). No significant differences were found for gender, undergraduate major, graduate school area of concentration, or GPA.
|
|
Number (%) of applicants by practice location, N=509
|
|
|
Characteristic*
|
In state
|
Out of state
|
P value
|
|
Total
|
212 (42)
|
297 (58)
|
|
|
Average age at admission
|
25
|
24
|
<.001
|
|
Female
|
121 (57)
|
154 (52)
|
ns
|
|
URiM
|
100 (47)
|
98 (33)
|
<.01
|
|
In-state HS
|
180 (85)
|
247 (83)
|
ns
|
|
Rural HS
|
40 (19)
|
83 (28)
|
<.05
|
|
In-state IHE
|
140 (66)
|
163 (55)
|
<.05
|
|
Rural IHE
|
15 (7)
|
24 (8)
|
ns
|
|
STEM major/grad work
|
167 (79)
|
229 (77)
|
ns
|
|
Premed major (bio/health)
|
157 (74)
|
220 (74)
|
ns
|
|
Average GPA
|
3.58
|
3.63
|
ns
|
|
Average MCAT
|
56 %tile
|
67 %tile
|
<.001
|
|
>BA/BS degree
|
25 (12)
|
28 (10)
|
ns
|
Step 2: Multiple Regression
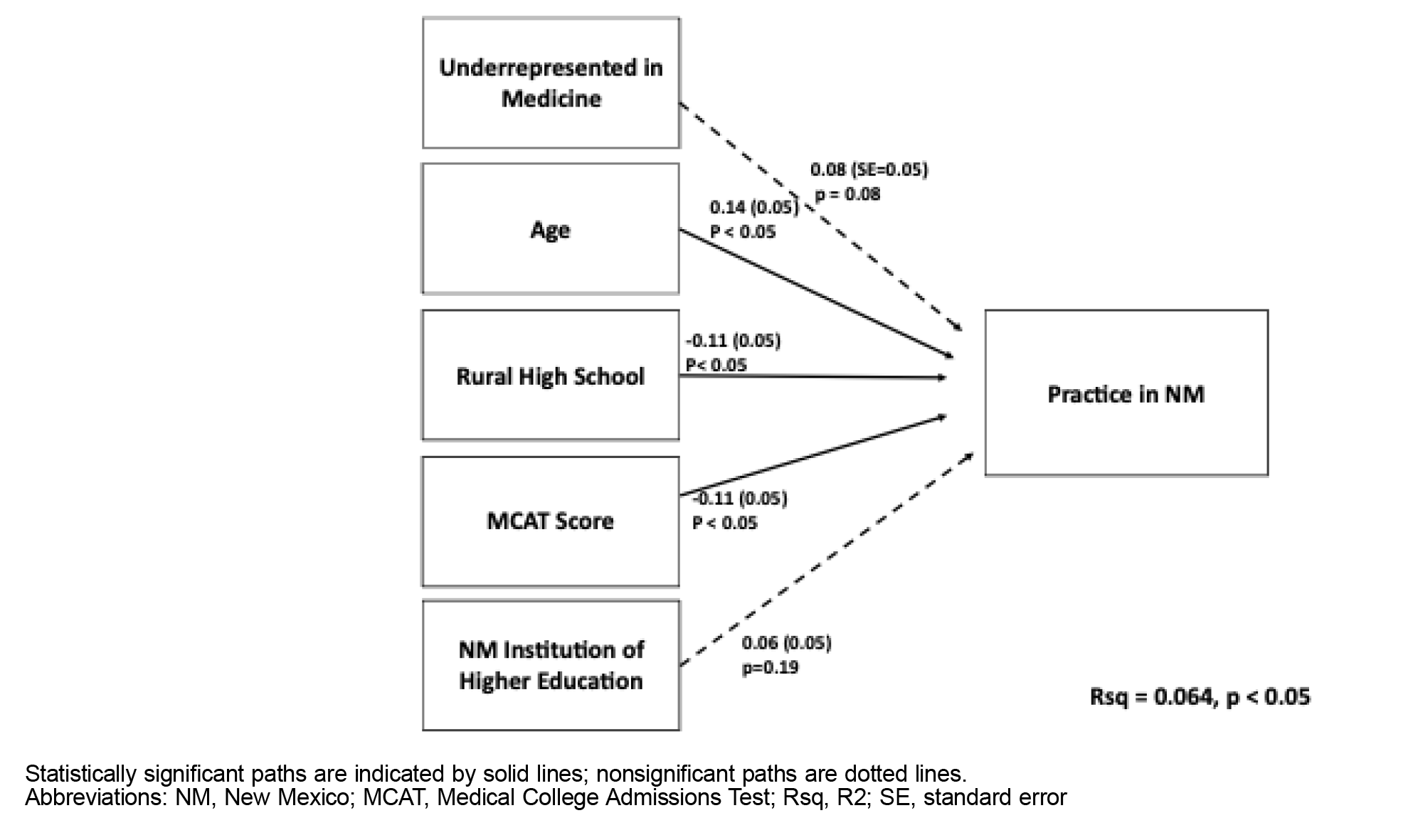
A multiple regression was done to determine independent effects of statistically significant predictors from univariate analysis. Figure 1 illustrates the path model of statistically significant applicant characteristics (URiM status, age, rural high school, MCAT score percentile, and NMIHE). Relationships as indicated by the coefficients and model R
2 are standardized estimates with significant relationships indicated by solid arrows and nonsignificant by dotted arrows. Of the five relationships, three were significant: age (0.14, P<.05), graduating from a rural high school (-0.11, P=.02), and MCAT percentile (-0.11, P<=.05). These data indicated, holding all other variables constant, the following: As age increases by 0.14 years, in-state practice increases 1%; as proportion graduating from rural high school decreases 0.011, in-state practice increases by 1%; and as MCAT percentile decreases by 0.011%, in-state practice increases by 1%. URiM and NMIHE drop out of statistical significance in the multiple regression.
The R
2 is significant (P<.05) with an estimate of 0.064; this model explains 6.4% of the variance. Considering the substantial number of characteristics that could explain practicing in NM, this R
2 provides some, but limited, insight.
Univariate analysis of applicant objective data that would predict applicants’ likelihood of practicing in-state in the future revealed that older, minority, urban high school or in-state institution of higher education graduates, or those with lower MCAT percentiles were more likely to practice in-state. However, multiple regression modeling showed that only age, not attending a rural high school and MCAT percentile, was associated with future in-state practice. Identifying as URiM and graduating from a NMIHE were not.
Age being significantly associated with future in-state practice may suggest that older applicants have different personal or professional motivations. Explanations for associations between lower MCAT percentile and urban high school with future in-state practice are not evident.
The most important conclusion is the limited value of applicant objective attributes predicting future in-state practice. Multiple regression modeling explained only 6.4% of variance, indicating the existence of factors not captured in our analysis. These findings suggest a holistic approach to admissions may aid in predicting future in-state practice by considering applicant experiences, values, goals, motivations, and lifestyle preferences.
Although the study focused on informing admissions committees, important to acknowledge is that factors evolve throughout subsequent training years (ie, health care policies, financial and workforce incentives, family circumstances, partner and family priorities, personal priorities, economic conditions), influencing choice of practice location by reinforcing or diminishing the importance of preexisting factors. While these factors may impact graduate physicians’ practice location, this future information is not available to admissions committees.
Limitations
These applicant objective data do not include the subjective elements (ie, narrative responses, community service, and interview data), which may offer greater value to admissions committees regarding future practice location. Additionally, the absence of data on specialty choices and in-state practice is also a limitation. Specialty information could clarify the alignment between admissions data, future specialty choice, and practice location. Further, although the use of eight cohorts is a strength of the analysis, generalizability is limited because they represented a single state.
These findings underscore challenges admissions committees face in predicting applicants most likely to practice in-state. Further research might explore the value of specific subjective applicant data in this role. Incorporating specialty data could provide deeper insights into how admissions data may be associated with meeting in-state needs. Identifying applicants likely to practice in-state and to address health care needs is clearly an important goal for many admissions committees. Nevertheless, committees are limited in judging future practice location from the snapshot presented in applications. Applicant objective data alone does not appear to effectively predict practice location.
References
-
Tamimi A, Hassuneh M, Tamimi I, et al. Admission criteria and academic performance in medical school.
BMC Med Educ. 2023;23(1):273.
doi:10.1186/s12909-023-04251-y
-
Almarabheh A, Shehata MH, Ismaeel A, Atwa H, Jaradat A. Predictive validity of admission criteria in predicting academic performance of medical students: a retrospective cohort study.
Front Med (Lausanne). 2022;9:971926.
doi:10.3389/fmed.2022.971926
-
Davies TA, Miller MB, Moore VA, Kaye EA. Predicting professional school performance with a unique lens: are there other cognitive predictors?
BMC Med Educ. 2020;20(1):14.
doi:10.1186/s12909-020-1930-2
-
Mwandigha LM, Tiffin PA, Paton LW, Kasim AS, Böhnke JR. What is the effect of secondary (high) schooling on subsequent medical school performance? a national, UK-based, cohort study.
BMJ Open. 2018;8(5):e020291.
doi:10.1136/bmjopen-2017-020291
-
Owen JA, Conaway MR, Bailey BA, Hayden GF. Predicting rural practice using different definitions to classify medical school applicants as having a rural upbringing.
J Rural Health. 2007;23(2):133-140.
doi:10.1111/j.1748-0361.2007.00080.x
-
Pretorius RW, Lichter MI, Okazaki G, Sellick JA Jr. Where do they come from and where do they go: implications of geographic origins of medical students.
Acad Med. 2010;85(10):S17-S20.
doi:10.1097/ACM.0b013e3181ed3e78
-
Owen JA, Hayden GF, Bowman RC. Influence of places of birth, medical education, and residency training on the eventual practice locations of family physicians: recent experience in Virginia. South Med J. 2005;98(6):674-675.
-
Wendling AL, Shipman SA, Jones K, Kovar-Gough I, Phillips J. Defining rural: the predictive value of medical school applicants’ rural characteristics on intent to practice in a rural community. Acad Med. 2019;94(11S Association of American Medical Colleges Learn Serve Lead: Proceedings of the 58th Annual Research in Medical Education Sessions):S14-S20.
-
-
Koehler TJ, Goodfellow J, Davis AT, Spybrook J, vanSchagen JE, Schuh L. Predicting in-state workforce retention after graduate medical education training.
J Grad Med Educ. 2017;9(1):73-78.
doi:10.4300/JGME-D-16-00278.1
-
Ballejos MP, Shane N, Romero-Leggott V, Sapién RE. Combined baccalaureate/medical degree students match into family medicine residencies more than similar peers: a matched case-control study.
Fam Med. 2019;51(10):854-857.
doi:10.22454/FamMed.2019.110812
-
Reilly JM, Greenberg I. An 8-year review of match outcomes from a primary care pipeline program.
Fam Med. 2023;55(10):646-652.
doi:10.22454/FamMed.2023.297644
-
Knottenbelt SZ, Ballejos MP, Torrez D, et al. Evolution of a combined baccalaureate/medical degree program as a pipeline to primary care: retention strategies and lessons learned.
Fam Pract. 2025;42(2):cmae066.
doi:10.1093/fampra/cmae066
-
Rabinowitz HK, Diamond JJ, Markham FW, Santana AJ. The relationship between entering medical students’ backgrounds and career plans and their rural practice outcomes three decades later.
Acad Med. 2012;87(4):493-497.
doi:10.1097/ACM.0b013e3182488c06
-
Addams AN, Bletzinger RB, Sondheimer HM, White SE, Johnson LM. Roadmap to Diversity: Integrating Holistic Review Practices Into Medical School Admission Processes. Association of American Medical Colleges; 2010.



There are no comments for this article.