Background and Objectives: Despite the increasing number of sexual and gender minority (SGM) patients in the United States and designation by the National Institutes of Health as a population with health disparities, available tools are lacking to train medical students on appropriate care for this population. Therefore, we developed and implemented a novel, self-directed, 2-week online elective for undergraduate medical students. The objective of our study was to evaluate the effectiveness of this course in increasing medical students’ competency and confidence in caring for SGM patients.
Methods: We developed the curriculum using Kern’s six-step model for curriculum development. We created anonymous pre- and postcourse surveys using the standardized Lesbian, Gay, Bisexual, Transgender Development of Clinical Skills Survey (LGBT-DOCSS) questionnaire to assess cultural competence, as well as a 5-point Likert-scored survey to assess self-perceived confidence in the care of SGM patients. We tested the statistical significance in pre- and postsurvey scores via paired sample t tests in R (R Project for Statistical Computing).
Results: We found statistically significant increases in the LGBT-DOCSS categories of clinical preparedness (P<.001), basic knowledge (P<.001), overall competency (P<.001), and self-perceived confidence in caring for SGM patients (P<.001, N=33).
Conclusions: The course represents an effective solution for increasing medical students’ self-perceived competence and confidence in caring for SGM patients. The flexibility and ease of the online format may be appealing to both students and institutions, and ultimately can serve to increase access to crucial content that is largely absent from current undergraduate medical education. Future evaluation efforts will be required to determine whether the course impacts long-term behavioral changes and outcomes.
The sexual and gender minority (SGM) community is a growing proportion of the US population, with 7.1% of US adults and one in five Generation Z adults identifying as lesbian, gay, bisexual, transgender, queer or questioning, intersex, asexual, or other (LGBTQIA+) and 9.2% of high school students identifying as gender diverse. 1, 2 Despite this demographic growth, health disparities, such as the number of adverse childhood events, 3 within SGM populations have worsened across generations, suggesting that SGM health may be declining. The urgency of these disparities is supported by the National Institutes of Health’s formal recognition of SGMs as a population with health disparities. 4 While the field of SGM health has grown in recent decades, a significant need remains to improve health outcomes in this population.
Of particular concern is the need to improve the quality of health care provided to the SGM community. SGMs often face discrimination and stigma in the health care setting from practitioners and other staff, which creates barriers to receiving quality care. 4 Minority stress theory has posited that stressors faced by SGMs, including stigma in health care, contribute to chronic stress and adverse health outcomes. 5 Intersectional biopsychosocial frameworks have suggested that overlapping identities can intensify exposure to chronic stress, and individuals who identify both as Black, Indigenous, or People of Color and SGM have been found to have more adverse health outcomes and suboptimal health care access. 6, 7
Health care providers, however, do not currently receive adequate training on how to provide high-quality, comprehensive care for SGMs. 4 Despite evidence that medical students with SGM clinical experience (compared to those without) provide higher quality care to SGM patients, students in the United States receive only 5 hours of training specific to SGM health care. 8 Evidence has suggested that medical students may require as many as 35 hours of SGM-focused didactic hours to achieve high cultural competency. 9 However, many medical schools fall well below this benchmark. 8 Some medical schools have implemented a one-time session on SGM health in residency preparation courses or have created a longitudinal track for students focused on SGM health. 10, 11 While these efforts are valuable, a single session is limited in its ability to be comprehensive, and a longitudinal track targets only students already interested in SGM health. To prepare future physicians, especially primary care providers, to care for a diverse patient population, incorporating more robust and widely accessible SGM content into undergraduate medical education is essential.
To address this need, we created and implemented a novel, comprehensive, 2-week online elective for undergraduate medical students focused on SGM health. The objective of this study was to evaluate how this course impacted the self-perceived confidence and competence of undergraduate medical students regarding the care of SGM patients.
A self-directed, 2-week online elective, Introduction to LGBTQIA+ Health, was developed by students and faculty using Kern’s six-step approach to curriculum development to address the need for SGM health education. 12 The course was offered to third- and fourth-year undergraduate medical students at the University of Michigan as an elective that counted toward nonclinical graduation requirements, with voluntary enrollment throughout the year. The course contains 10 modules that build from basic foundational concepts to specialty-specific care using a combination of written content, multimedia, and prerecorded expert lectures. Each module concludes with a 10-question quiz requiring a passing grade of 80%. To receive educational credit, all students are required to complete pre-and postsurveys. As part of these surveys, we used the 18-item, 7-point Likert Lesbian, Gay, Bisexual, Transgender Development of Clinical Skills Survey (LGBT-DOCSS; Appendix A) to assess cultural competency with an overall mean score in three specific domains: attitudinal awareness, basic knowledge, and clinical preparedness. 13 Higher scores indicate higher levels of knowledge and preparedness in caring for SGM individuals. Scores of 6 and above are defined as high competency, 5 to 6 as moderate competency, and lower than 5 as low competency. 9 We also assessed self-perceived confidence in the care of SGM patients via a 5-point Likert retrospective pre–post survey (Appendix B). Paired sample t tests were conducted in R to assess differences in pre- and postscores. This research was granted exemption by the University of Michigan Institutional Review Board (HUM00217485).
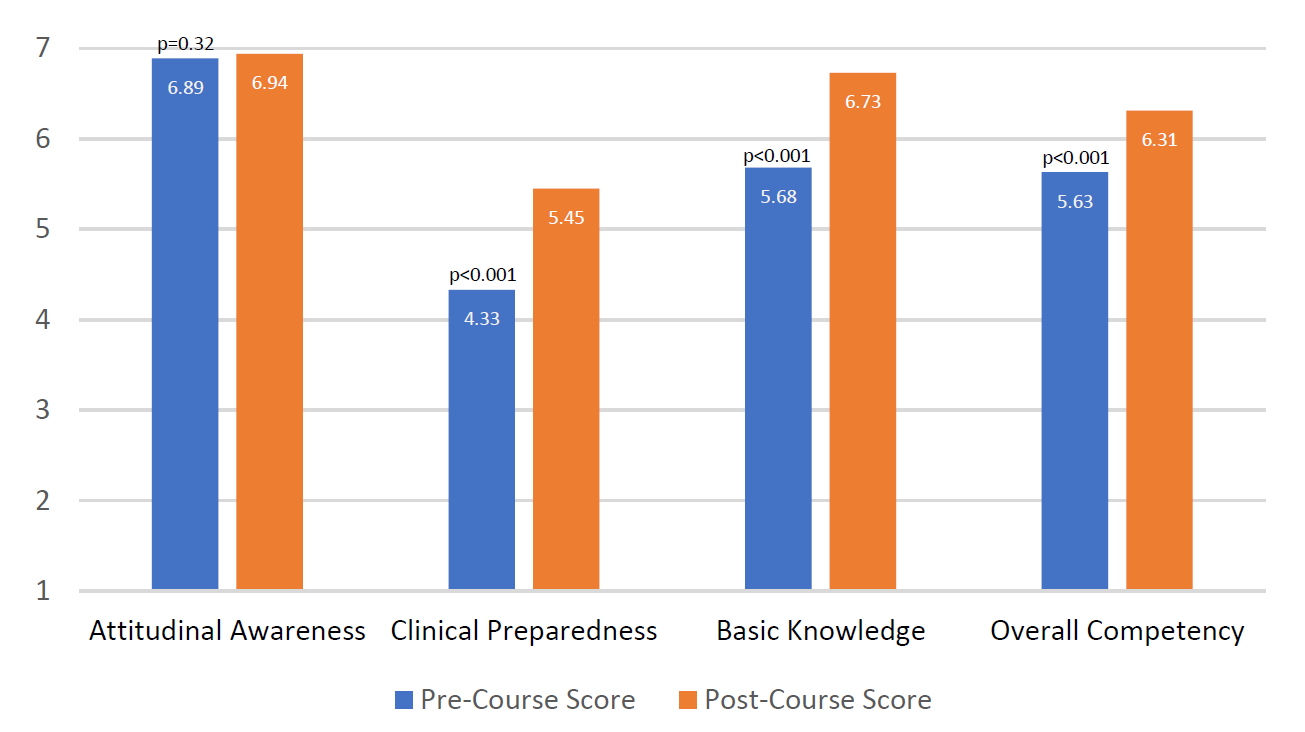
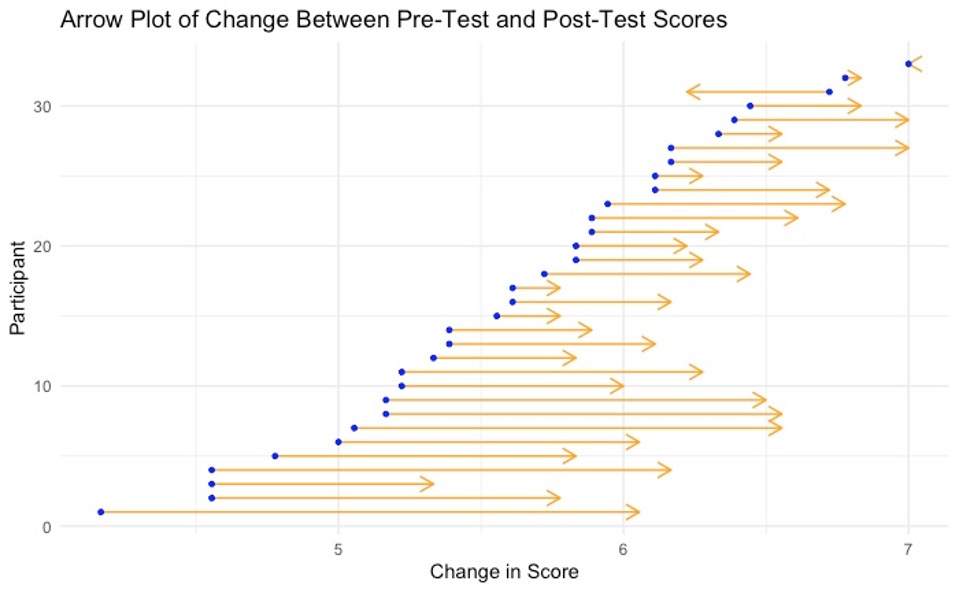
Thirty-three students completed the course at the time of analysis. Prior to the course, students on average had high attitudinal awareness (6.89), low clinical preparedness (4.33), moderate basic knowledge (5.68), and moderate overall competency (5.63) on a 7-point Likert scale (Table 1, Figure 1). Improvement in all LGBT-DOCSS items was observed with significant increases in clinical preparedness (from low to moderate, 5.45, P<.001), basic knowledge (from moderate to high, 6.73, P<.001), and overall competency (from moderate to high, 6.31, P<.001; Figure 1, Figure 2). Regarding the 5-point Likert self-perceived confidence scale, students reported low confidence in caring for lesbian, gay, and bisexual (LGB) patients (2.76) as well as transgender and gender diverse patients (2.33) prior to the course (Table 1 ). After completion of the course, students showed significantly improved confidence in caring for LGB patients (3.76, P<.001) and transgender and gender-diverse patients (3.52, P<.001).
|
|
Item
|
Precourse score M (SD)
|
Postcourse score M (SD)
|
Mean difference (95% CI)
|
P c
|
|
LGBT-DOCSSa
|
Attitudinal awarenessd
|
6.89 (0.24)
|
6.94 (0.2)
|
0.05 (-0.05 to 0.14)
|
.32
|
|
Clinical preparednesse
|
4.33 (1.48)
|
5.45 (1)
|
1.12 (0.77 to 1.48)
|
<.001
|
|
Basic knowledgef 4
|
5.68 (0.97)
|
6.73 (0.34)
|
1.05 (0.72 to 1.37)
|
<.001
|
|
Overall competency
|
5.63 (0.7)
|
6.31 (0.42)
|
0.69 (0.51 to 0.87)
|
<.001
|
|
Confidence scoreb
|
Caring for LGB patients
|
2.76 (1.09)
|
3.76 (0.83)
|
1.00 (0.72 to 1.28)
|
<.001
|
|
Caring for trans and gender-diverse patients
|
2.33 (1.27)
|
3.52 (0.91)
|
1.18 (0.84 to 1.52)
|
<.001
|
DISCUSSION AND CONCLUSIONS
This research shows that the Introduction to LGBTQIA+ Health course significantly increased the self-perceived competence and confidence of undergraduate medical students in caring for SGM patients. Students were found to have significant improvement in self-rated clinical preparedness, basic knowledge, overall competency, and confidence in treating SGM patients. These findings indicate that this curriculum has the potential to help prepare future physicians to care for this patient population. As far as we are aware, this is the most comprehensive online, asynchronous course on SGM health designed specifically for undergraduate medical education. Given the current paucity of SGM health in medical education, this course provides an example for other programs looking to similarly expand their own curricula. 4, 14 The hope is that increased provider knowledge and competency leads to higher quality care and decreased stigmatization to ultimately improve outcomes. 4, 5, 15
This study had several limitations. Students self-selected to participate in this course, which may indicate prior interest and/or knowledge related to SGM health and may have contributed to the high attitudinal awareness scores in precourse surveys. Additionally, given the small number of students who have taken the course thus far, the limited sample size prevented the use of more complex analyses, such as a fixed-effects model. Also, students included in this analysis were limited to a single institution, and different institutions may have SGM health education already included in their curricula, which may affect outcomes. Another limitation is that, while the LGBT-DOCSS survey tool is a validated instrument, its measures were all self-perceived. Finally, because no simulated clinical practice or longitudinal data exists, we cannot comment on whether the course has changed behaviors or patient outcomes.
Future efforts include transforming this course into a massive online open course (MOOC) available to trainees at other institutions. 16 Of note, the course is now available to residents and physicians at the University of Michigan due to high levels of interest, and we will continue to collect data from participants. We also are continuously adding modules on additional topics. It is noteworthy that such a significant change was seen with only a 2-week, online course, prompting consideration of whether further improvement could be achieved with more interactive curricular components, such as shadowing clinical providers or standardized patient interactions, which are widely used in medical education. 17 With the addition of in-person clinical experiences and assessments, we may better achieve and evaluate student growth in clinical skills. We are considering collecting longitudinal, postintervention data to evaluate how the course affects participants’ future clinical practice, as well.
Our hope is that the success of this SGM health curriculum will encourage other undergraduate medical institutions to similarly provide SGM education for their trainees.
References
-
-
Kidd KM, Sequeira GM, Douglas C, et al. Prevalence of gender-diverse youth in an urban school district. In:
Social Determinants of Health, Part 1: Underserved Communities. American Academy of Pediatrics; 2022:116-118.
doi:10.1542/9781610026352-part01-prevalence
-
Hughes PM, Ostrout TL, Pèrez Jolles M, Thomas KC. Adverse childhood experiences across birth generation and LGBTQ
+ identity, behavioral risk factor surveillance system, 2019.
Am J Public Health. 2022;112(4):662-670.
doi:10.2105/AJPH.2021.306642
-
White J, Sepúlveda MJ, Patterson CJ, eds. Understanding the Well-Being of LGBTQI+ Populations. National Academies Press; 2020.
-
Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence.
Psychol Bull. 2003;129(5):674-697.
doi:10.1037/0033-2909.129.5.674
-
Trinh MH, Agénor M, Austin SB, Jackson CL. Health and healthcare disparities among U.S. women and men at the intersection of sexual orientation and race/ethnicity: a nationally representative cross-sectional study.
BMC Public Health. 2017;17(1):964.
doi:10.1186/s12889-017-4937-9
-
Christian LM, Cole SW, McDade T, et al. A biopsychosocial framework for understanding sexual and gender minority health: a call for action.
Neurosci Biobehav Rev. 2021;129:107-116.
doi:10.1016/j.neubiorev.2021.06.004
-
Obedin-Maliver J, Goldsmith ES, Stewart L, et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education.
JAMA. 2011;306(9):971-977.
doi:10.1001/jama.2011.1255
-
Nowaskie DZ, Patel AU. How much is needed? Patient exposure and curricular education on medical students’ LGBT cultural competency.
BMC Med Educ. 2020;20(1):490.
doi:10.1186/s12909-020-02381-1
-
Gibson AW, Gobillot TA, Wang K, et al. A novel curriculum for medical student training in LGBTQ healthcare: a regional pathway experience.
J Med Educ Curric Dev. 2020;7:2382120520965254.
doi:10.1177/2382120520965254
-
Roth LT, Friedman S, Gordon R, Catallozzi M. Rainbows and “ready for residency”: integrating LGBTQ health into medical education.
MedEdPORTAL. 2020;16:11013.
doi:10.15766/mep_2374-8265.11013
-
Thomas PA, Kern DE, Hughes MT, Chen BY. Curriculum Development for Medical Education: A Six-Step Approach. Johns Hopkins University Press; 2015.
-
Bidell MP. The lesbian, gay, bisexual, and transgender development of clinical skills scale (LGBT-DOCSS): establishing a new interdisciplinary self-assessment for health providers.
J Homosex. 2017;64(10):1,432-1,460.
doi:10.1080/00918369.2017.1321389
-
-
-
Masters K. A brief guide to understanding MOOCs.
Int J Med Educ. 2011;1(2).
doi:10.5580/1f21
-



There are no comments for this article.