Background and Objectives: Limited knowledge is present regarding how fellowship training correlates with graduate outcomes and whether current residents desire an additional year of residency training. The aim of this study is to examine trends in fellowship training and compare residency and practice outcomes between those interested and those not interested in fellowship training as well as the proportion of residents desiring an additional year of residency training.
Methods: We compared data from the American Board of Family Medicine Initial Certification Questionnaire (2017–2019) to the National Graduate Survey (NGS; 2020–2022). We used bivariate analysis and ꭓ2 tests to assess for changes over time and to determine whether an association exists between those likely to pursue a fellowship and those interested in an additional year of residency training.
Results: The final sample included 4,930 residency graduates with NGS data (response rate 46.8%). Overall, most (71.0%) respondents were not interested in any type of additional training. We found no differences in interest in a fellowship based on in-training examination (ITE), certification scores, or milestones attainment. Respondents without interest in a fellowship were more likely to provide continuity of care in practice, while respondents with interest in a fellowship were more likely to be faculty and less likely to have symptoms of burnout.
Conclusions: Intention for fellowship training is associated with future faculty members and lower rates of symptoms of burnout and continuity practice. A majority of responding family medicine residents (>70%) do not favor an additional year of residency training.
The length of time needed to adequately train a family physician (FP) has been a subject of investigation and debate for years. While adding a year to current requirements for residency training has been proposed, many FPs seek fellowship positions following completion of their residency training as a means to increase the length of formal training, though in a specific topic area.
A wide variety of fellowship programs for FPs are available, with sports medicine, geriatrics, maternity care, and faculty development among the most common. 1 Previous studies have reported conflicting data regarding the numbers of FPs seeking and completing such training: one showed a decrease in graduates who pursued fellowships that lead to Certificates of Added Qualifications; another showed an increase in fellowship completion. 2, 3 No recent studies examining FPs seeking fellowship training are available. The reasons for seeking fellowship training differ among candidates and may include an extension of formal training to better prepare for independent practice, acquire a subset of knowledge and skills, or increase earning potential.
While many FP residency graduates reported feeling adequately trained in general, less than 20% of them felt that training adequately prepared them for practice in specific procedural skills, including uterine aspiration, pregnancy termination, musculoskeletal ultrasound, vasectomy, and osteopathic manipulative treatment. 4 As such, any additional training, whether through extended residency or fellowship, may improve this apparent deficit in training and lead to additional confidence in these and other areas. Interestingly, fellowship trained FPs (n=50) had scores on various well-being scales that were higher than the general FP population (n=203) studied. 5
Limited data are available on the proportion of family medicine residency graduates who intend to pursue fellowship training, whether this proportion has changed over time, and whether fellows disproportionately feel that another year of residency training is warranted compared to physicians who do not do fellowships. An initial study found a disconnect between fellowship intention and desire for another year of residency training. 1 Desire for fellowship may be more about obtaining specific skills, expertise, or additional certifications, and less about being prepared for general practice in family medicine.
Additional study is needed regarding family medicine residents and their thoughts on fellowship training or extension of training through an additional year of residency. The specific aim of this study was to examine trends in interest in fellowship training or an additional year of residency training by family medicine residents. Furthermore, we compared residency outcomes, in-training examination (ITE) scores, perceived preparation for practice, certification examination scores, milestones assessments, and practice patterns between those interested and those not interested in additional training.
We used data from the American Board of Family Medicine (ABFM) Initial Certification Questionnaire (ICQ) from 2017 through 2019 linked to outcomes data on the same FPs 3 years later, 2020 through 2022, from the National Graduate Survey (NGS). The ICQ is completed when residents register for the Family Medicine Certification Exam, usually in December through February of their final year of residency. Questionnaire items ask about future employment, practice type, and intention to perform procedures and provide various clinical activities. The NGS is a nonmandatory survey administered to all ABFM-certified diplomates 3 years after graduation from residency training. 6, 7 This survey asks questions regarding scope of practice, practice location and organization, preparation for practice in residency, burnout and satisfaction, and faculty status. We obtained the postgraduate year 3 training ITE score, certification examination score, and milestones ratings from ABFM databases. We obtained basic demographics (age, gender, ethnicity) from ABFM administrative data.
We limited our sample to residents in 3-year programs who completed residency in 3 years. For some analyses focused solely on outcomes collected on the ICQ, we used all FPs. For analyses using practice outcomes, we created a longitudinal cohort of residency graduates from 2017 to 2019 with NGS data from 2020 to 2022.
We focused on two items from the ICQ: “Are you planning on completing a fellowship after residency?” (yes/no/unsure), including a follow-up asking what type of fellowship if responding yes; and “Would you pursue an additional year of residency training if it were available at your program?” (yes/no). For the question on interest in fellowship, we removed the “unsure” group to obtain a clear comparison between those with a definite preference. To assess faculty-rated competence, we created two measures from milestones assessments: We defined meeting expectations as a rating of 4 on the final milestone assessment; and then we created a summary measure for the percentage of milestones met within the medical knowledge and patient care competencies. Practice location from the NGS was geocoded and rurality assigned using the Rural-Urban Continuum Codes. From the NGS data, we calculated the scope of practice score, which ranges from 0 to 30, with a higher number indicating a broader scope of practice. 8 We defined burnout as a response of “once a week” or more frequently to either the emotional exhaustion or depersonalization item. 9 Race and ethnicity were both self-reported by the physician on the ICQ in response to a “select best” single-response item. The respondent selects among presented categories, including “other.”
We used descriptive statistics to characterize our sample. We assessed the representativeness of the longitudinal sample by comparing characteristics of NGS responders and nonresponders. We used bivariate analysis to assess for changes over time in the relationship between interest in fellowship and in additional training. We assessed for changes over time in interest in fellowship and type of fellowship for the linked ICQ-NGS cohort. We used ꭓ2 tests to determine the association between the likelihood of pursuing a fellowship and interest in an additional year of training. We conducted two binary logistic regression analyses to identify characteristics (age, degree type, race, ethnicity, ITE and certification examination scores) associated with interest in pursuing a fellowship or interest in another year of training. This study was approved by the American Academy of Family Physicians Institutional Review Board. SAS Version 9.4 (SAS Institute) was used for all analyses.
The final sample included 4,930 residency graduates with NGS data (response rate 46.6%; Table 1). Small differences between respondents for the ICQ versus ICQ-NGS were noted in the gender and international medical graduate (IMG) categories, with a higher percentage of females and non-IMGs participating in the NGS.
|
|
ICQ,
n (%)
|
ICQ-NGS
longitudinal,
n (%)
|
P
|
|
Survey year
|
|
2017/2020
|
3,369 (31.9)
|
1,636 (33.2)
|
.1830
|
|
2018/2021
|
3,533 (33.4)
|
1,586 (32.2)
|
|
2019/2022
|
3,667 (34.7)
|
1,708 (34.6)
|
|
Total
|
10,569 (100.0)
|
4,930 (100.0)
|
|
|
Age in years at time of ICQ, Mean (SD)
|
|
|
32.27 (4.11)
|
32.34 (4.05)
|
.0757
|
|
Gender
|
|
Female
|
5,739 (54.3)
|
2,751 (55.8)
|
.0114
|
|
Male
|
4,815 (45.6)
|
2,173 (44.1)
|
|
|
Degree type
|
|
DO
|
2,301 (21.8)
|
1,050 (21.3)
|
.3036
|
|
MD
|
8,268 (78.2)
|
3,880 (78.7)
|
|
|
International medical graduate
|
|
Yes
|
3,298 (31.2)
|
1,473 (29.9)
|
.0114
|
|
No
|
7,271 (68.8)
|
3,457 (70.1)
|
|
|
Practice rurality at NGS
|
|
Metropolitan
|
|
3,888 (84.9)
|
|
|
Nonmetropolitan
|
|
694 (15.1)
|
|
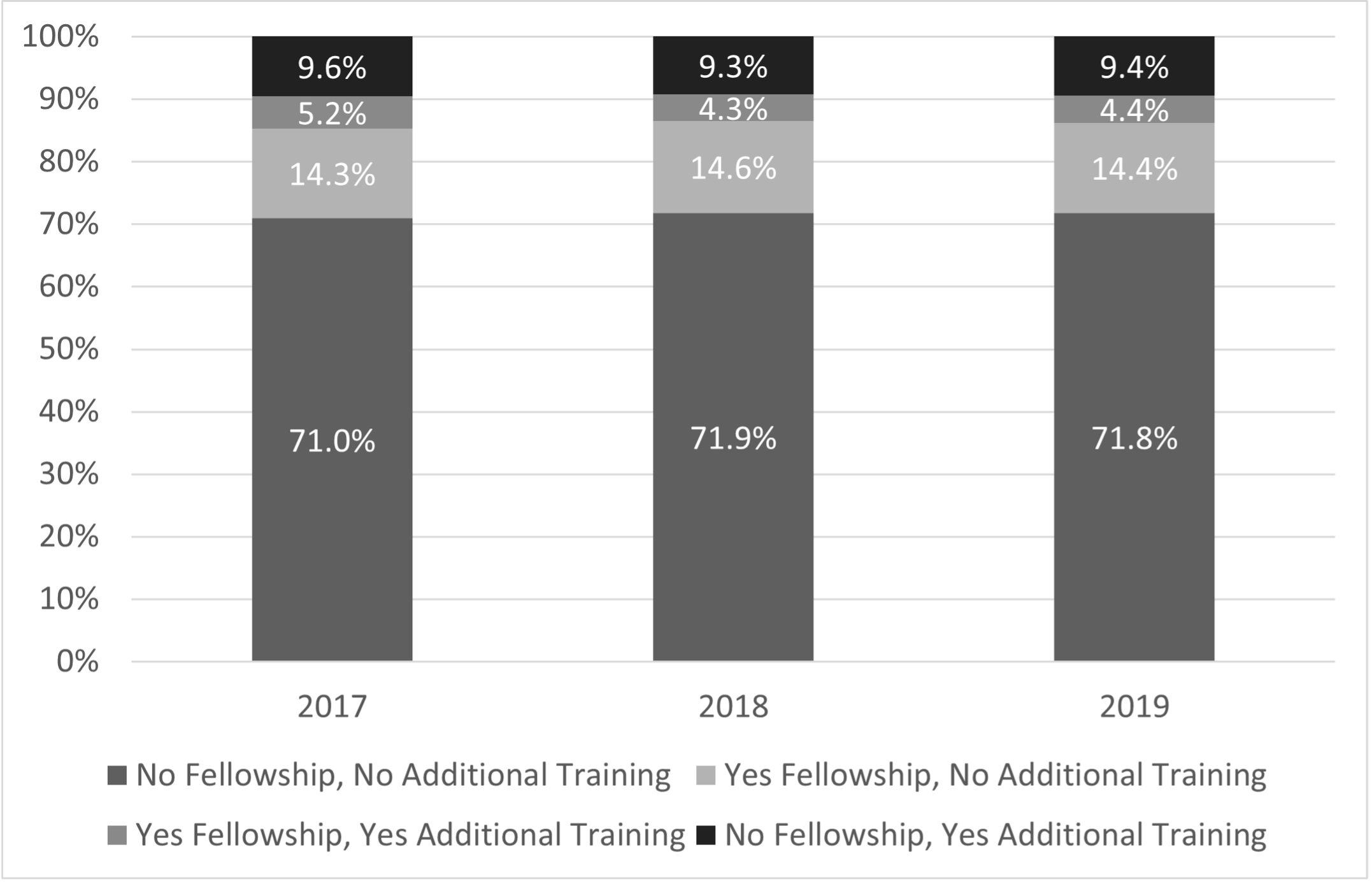
During each year of the study period, about 71% of residents were not interested in either fellowship or additional residency training (Figure 1). About 14% were interested in an additional year of residency training, and similarly, about 14% were interested in a fellowship without additional residency training.
From 2017 to 2019, interest in any fellowship training remained stagnant, as did interest in specific fellowships (Table 2). The most popular choices for intended fellowship were sports medicine (32%–36%), maternity care/OB (11%–16%), and geriatrics (10%–13%). Clinical informatics, HIV care, and rural health, on average, had interest by two or fewer residents per year.
|
|
2017–2020, n (%)
|
2018–2021, n (%)
|
2019–2022, n (%)
|
|
Addiction medicine
|
2 (0.7)
|
4 (1.4)
|
7 (2.3)
|
|
Adolescent medicine
|
3 (1.1)
|
|
1 (0.3)
|
|
Behavioral medicine
|
1 (0.4)
|
1 (0.4)
|
1 (0.3)
|
|
Clinical informatics
|
1 (0.4)
|
2 (0.7)
|
|
|
Emergency medicine
|
18 (6.3)
|
16 (5.6)
|
17 (5.7)
|
|
Faculty or academic development
|
6 (2.1)
|
8 (2.8)
|
6 (2.0)
|
|
Geriatrics
|
37 (13.0)
|
34 (12.0)
|
31 (10.4)
|
|
HIV care
|
1 (0.4)
|
2 (0.7)
|
|
|
Hospice and palliative medicine
|
23 (8.1)
|
22 (7.7)
|
30 (10.1)
|
|
Hospital medicine
|
4 (1.4)
|
7 (2.5)
|
9 (3.0)
|
|
Integrative medicine
|
8 (2.8)
|
8 (2.8)
|
10 (3.4)
|
|
International/global health
|
8 (2.8)
|
5 (1.8)
|
6 (2.0)
|
|
Maternity care/OB
|
35 (12.3)
|
33 (11.6)
|
49 (16.4)
|
|
Other
|
24 (8.5)
|
20 (7.0)
|
15 (5.0)
|
|
Pain management
|
|
1 (0.4)
|
3 (1.0)
|
|
Preventive medicine
|
2 (0.7)
|
1 (0.4)
|
2 (0.7)
|
|
Research
|
4 (1.4)
|
6 (2.1)
|
6 (2.0)
|
|
Rural health
|
|
1 (0.4)
|
|
|
Sleep medicine
|
7 (2.5)
|
6 (2.1)
|
7 (2.3)
|
|
Sports medicine
|
95 (33.5)
|
104 (36.6)
|
95 (31.9)
|
|
Women’s health
|
5 (1.8)
|
3 (1.1)
|
3 (1.0)
|
|
Total participant interest
|
289 (17.7)
|
284 (17.9)
|
298 (17.4)
|
|
Total participants
|
1,636
|
1,586
|
1,708
|
Restricting the analysis to those with matching practice outcome data from the NGS, we found significant differences in terms of respondent intention to apply for fellowship training by age of respondent and degree type (Appendix Table 1). In addition, we found no differences in ITE, certification scores, or milestones attainment by interest in a fellowship (Appendix Table 1). Respondents without interest in a fellowship were more likely to provide continuity of care in practice. Respondents with interest in a fellowship were more likely to be faculty and less likely to have symptoms of burnout (Appendix Table 2).
Based on regression analysis controlling for all other variables shown in Table 3 , respondents who were Hispanic had significantly lower odds of desiring an additional year of residency training (AOR=0.68, 95% CI 0.52,0.89). In contrast, respondents who were younger (<35 yrs of age), were DO, and were from the Midwest compared to those from the West had significantly higher odds of desiring an additional year of residency training (AOR=1.32, 95% CI 1.07,1.62; AOR=1.29, 95% CI 1.03,1.16; and AOR=1.48, 95% CI 1.15, 1.90 respectively). Finally, respondents from the Northeast when compared to the West had significantly lower odds of interest in pursuing a fellowship (AOR=0.75, 95% CI 0.57,0.99). No other significant relationships were found.
|
|
Interest in another year of residency training, AOR (95% CI)
|
Interest in fellowship, AOR (95% CI)
|
|
Physician characteristics
|
|
Age
|
|
|
|
<35 years
|
1.32 (1.07, 1.62)
|
0.91 (0.72, 1.13)
|
|
≥35 years
|
REF
|
REF
|
|
Degree type
|
|
|
|
MD
|
REF
|
REF
|
|
DO
|
1.29 (1.03, 1.62)
|
0.94 (0.77, 1.16)
|
|
Race
|
|
|
|
Asian
|
0.91 (0.76, 1.20)
|
1.08 (0.86, 1.36)
|
|
Black or African American
|
0.91 (0.65, 1.28)
|
0.97 (0.68, 1.38)
|
|
Other
|
0.93 (0.68, 1.28)
|
0.90 (0.66, 1.24)
|
|
White
|
REF
|
REF
|
|
Ethnicity
|
|
|
|
Hispanic or Latino
|
0.68 (0.52, 0.89)
|
0.87 (0.66, 1.17)
|
|
Not Hispanic or Latino
|
REF
|
REF
|
|
PGY-3 in-training exam score
|
|
|
|
Low
|
0.89 (0.69, 1.15)
|
0.86 (0.67, 1.10)
|
|
Medium
|
REF
|
REF
|
|
High
|
0.92 (0.75, 1.13)
|
1.02 (0.84, 1.25)
|
|
ABFM certification exam score
|
|
|
|
Low
|
0.41 (0.14, 1.20)
|
1.85 (0.40, 8.56)
|
|
Medium
|
REF
|
REF
|
|
High
|
0.92 (0.76, 1.12)
|
1.02 (0.84, 1.23)
|
|
Milestones ratings
|
|
|
|
Met patient care milestones
|
0.86 (0.70, 1.06)
|
0.88 (0.72, 1.08)
|
|
Met medical knowledge milestones
|
0.86 (0.69, 1.07)
|
0.93 (0.75, 1.16)
|
|
Graduate practice characteristics
|
|
Rural practice
|
|
|
|
Yes
|
0.66 (0.42, 1.04)
|
0.67 (0.42, 1.04)
|
|
No
|
REF
|
REF
|
|
Practice location
|
|
|
|
Midwest
|
1.48 (1.15, 1.90)
|
1.25 (0.97, 1.61)
|
|
Northeast
|
0.99 (0.75, 1.31)
|
0.75 (0.57, 0.99)
|
|
South
|
1.11 (0.76, 1.20)
|
1.03 (0.82, 1.29)
|
|
West
|
REF
|
REF
|
Our study represents the largest examination of interest in fellowship or an additional year of training among family medicine residents. As noted, intention to participate in fellowship training is present in about 19% of family medicine residents. The differences based on degree type, gender, and life stages may be attributed to previous educational experiences, expectations regarding anticipated knowledge and skills for future practice, and unique characteristics of individuals within these groups. This finding requires further study.
Despite an interest in fellowship training, most family medicine residents do not favor an additional year of residency training. Interestingly, academic achievement as demonstrated by results of standardized testing or whether successful attainment of milestones occurred does not predict desire for more training. As such, one should question whether a fourth year of residency training in family medicine is desired.
While some respondents are interested in additional training beyond residency, the desired training appears focused on attaining additional knowledge and skills in specific areas such as sports medicine, geriatrics, and maternity care. Conceivably, this additional knowledge and experience in a specific area or skill could be obtained in residency training through changes in curricula, as some have suggested. 10 Most respondents desired to have this additional training confined to fellowships. In contrast, many family medicine leaders and residency programs favor an additional year of residency training. 11, 12 While a fourth year of residency training may be beneficial, the lack of interest by recent graduates is notable. Recent changes to Accreditation Council for Graduate Medical Education (ACGME) program requirements have increased the number of required elective experiences; and several programs have implemented track systems or areas of interest that may impact residents’ desire to pursue additional training through fellowships. 13 Future studies assessing programs with affiliated tracks and outcomes of their graduates could further explore how focused curricula influence future practice.
Furthermore, several additional findings should be noted. Not unexpectedly, younger respondents (<35 yrs of age) had greater odds of favoring additional years of training, which may be related to overall experiences and differing phases of life. A similar finding was based on degree type and may be related to experiences during medical school. Respondents with interest in a fellowship were less likely to have symptoms of burnout. For individuals at higher risk, this additional training may have a protective effect. Finally, the interest in pursuing additional training varied by region of residency training. This finding may reflect differing educational experiences and opportunities based on location of training.
Our study was subject to multiple limitations. First, the response rate was less than 50%. Data on actual fellowship completion to evaluate all practice outcomes was lacking, and only two data points were used—residency graduation and 3 years into practice. The risk of bias is reduced because a past study found a 70% agreement between intention to pursue an ACGME-accredited fellowship and completing it. 1 Not all questions included well-delineated definitions of terms such as continuity of care. Additionally, biases may impact results. For instance, only residents who selected a 3-year program were surveyed, and the initial survey was conducted during the participants’ final year of residency training. Residents who initially selected a 3-year training program, after nearly completing training and gaining a better understanding regarding the many facets of being a family physician, may or may not have gained a different perspective. Finally, many of our analyses are cross-sectional, and we cannot infer causality.
In conclusion, intention to pursue fellowship training is associated with future faculty members and lower rates of symptoms of burnout and continuity practice. The interest of responding residents in an additional year of training was low. These findings support the conclusion that extension of residency training is likely unpopular among current residents, and fellowship opportunities remain an important option for those searching for focused training outside their primary residency training. As curriculum requirements change and offer more opportunities for individualized training, further studies assessing fellowship preference and practice outcomes should be considered.
References
-
Sairenji T, Dai M, Eden AR, Peterson LE, Mainous AG III. Fellowship or further training for family medicine residents? Fam Med. 2017;49(8):618-621.
-
Ringdahl E, Delzell JE Jr, Kruse RL. Changing practice patterns of family medicine graduates: a comparison of alumni surveys from 1998 to 2004.
J Am Board Fam Med. 2006;19(4):404-412.
doi:10.3122/jabfm.19.4.404
-
Carek PJ, Diaz V, Dickerson LM, Peterson L, Johnson S. Preparation for practice in family medicine: before and after duty hours. Fam Med. 2012;44(8):539-544.
-
Peterson LE, Fang B, Puffer JC, Bazemore AW. Wide gap between preparation and scope of practice of early career family physicians.
J Am Board Fam Med. 2018;31(2):181-182.
doi:10.3122/jabfm.2018.02.170359
-
Duffrin C, Larsen L. The effect of primary care fellowship training on career satisfaction, happiness and perceived stress.
Postgrad Med J. 2014;90(1,065):377-382.
doi:10.1136/postgradmedj-2012-131512
-
Mitchell KB, Maxwell L, Miller T. The national graduate survey for family medicine.
Ann Fam Med. 2015;13(6):595-596.
doi:10.1370/afm.1874
-
Peterson LE. Using the family medicine national graduate survey to improve residency education by monitoring training outcomes.
Fam Med. 2021;53(7):622-625.
doi:10.22454/FamMed.2021.719992
-
O’Neill T, Peabody MR, Blackburn BE, Peterson LE. Creating the individual scope of practice (I-SOP) scale. J Appl Meas. 2014;15(3):227-239.
-
West CP, Dyrbye LN, Sloan JA, Shanafelt TD. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals.
J Gen Intern Med. 2009;24(12):1,318-1,321.
doi:10.1007/s11606-009-1129-z
-
Carek PJ, Mainous AG III. Are we preparing residents for their actual practices?
J Grad Med Educ. 2022;14(3):251-253.
doi:10.4300/JGME-D-22-00310.1
-
Carney PA, Eiff MP, Waller E, Jones SM, Green LA. Redesigning residency training: summary findings from the preparing the personal physician for practice (P4) project.
Fam Med. 2018;50(7):503-517.
doi:10.22454/FamMed.2018.829131
-
Douglass AB, Barr WB, Skariah JM, et al. Financing the fourth year: experience of required 4-year family medicine residency programs.
Fam Med. 2021;53(3):195-199.
doi:10.22454/FamMed.2021.249809
-
Roskos SE, Barreto TW, Phillips JP, King VJ, Eidson-Ton WS, Eden AR. Maternity care tracks at US family medicine residency programs.
Fam Med. 2021;53(10):857-863.
doi:10.22454/FamMed.2021.237852



There are no comments for this article.