Chronic pain management in the United States is an overwhelming and urgent problem for patients, health care providers, and regulatory bodies. The 2016 National Health Interview Survey reported that 20% of US adults had chronic pain and 8% had high-impact chronic pain.1 Despite opioid prescriptions more than doubling between 2000-2010; pain metrics in the population did not decrease and overdose deaths rose by 200%.2,3 This alarming trend resulted in the US Department of Health and Human Services declaring the opioid epidemic a public health crisis in 2017. 4,5 The pronouncement of this public health crisis, the 2016 revised Opioid Guidelines by the Centers for Disease Control, and other regulatory bodies’ efforts have demonstrated a trend toward less opiate prescribing.6,7 However, this has left clinicians and patients seeking ways to manage chronic pain more effectively.3,8
ORIGINAL ARTICLES
Educating Physicians in Family Medicine Residencies About Nonpharmacologic Approaches to Pain:
Results of an Online Integrative Course
Ann Marie Chiasson, MD, MPH | Audrey J. Brooks, PhD | Mari Ricker, MD | Patricia Lebensohn, MD | Mei-Kuang Chen, PhD | Victoria Maizes, MD
Fam Med. 2020;52(3):189-197.
DOI: 10.22454/FamMed.2020.865003
Background and Objectives: Opioid misuse is at an all-time crisis level, and nationally enhanced resident and clinician education on chronic pain management is in demand. To date, broad-reaching, scalable, integrative pain management educational interventions have not been evaluated for effectiveness on learner knowledge or attitudes toward chronic pain management.
Methods: An 11-hour integrative pain management (IPM) online course was evaluated for effect on resident and faculty attitudes toward and knowledge about chronic pain. Participants were recruited from family medicine residencies participating in the integrative medicine in residency program. Twenty-two residencies participated, with 11 receiving the course and 11 serving as a control group. Evaluation included pre/post medical knowledge and validated measures of attitude toward pain patients, self-efficacy for nondrug therapies, burnout, and compassion.
Results: Forty-three participants (34.4%) completed the course. The intervention group (n=50), who received the course, improved significantly (P<.05) in medical knowledge, attitude toward pain patients, and self-efficacy to prescribe nondrug therapies while the control group (n=54) showed no improvement. There was no effect on burnout or compassion for either group. The course was positively evaluated, with 83%-94% rating the course content and delivery very high. All participants responded that they would incorporate course information into practice, and almost all thought what they learned in the course would improve patient care (98%).
Conclusions: Our findings demonstrate the feasibility of an online IPM course as an effective and scalable intervention for residents and primary care providers in response to the current opioid crisis and need for better management of chronic pain. Future directions include testing scalability in formats that lead to improved completion rates, implementation in nonacademic settings, and evaluation of clinical outcomes such as decreased opioid prescribing.
Chronic Pain and Integrative Medicine
Central to the opioid epidemic is the multifactorial nature of chronic pain that sets it apart from acute pain; central and peripheral upregulation and hypersensitization of pain receptors and pain pathways requires therapies that can address this differing etiology. Integrative medicine (IM) has an important role in chronic pain treatment and the medical literature now bears out the efficacy of many IM modalities for both acute and chronic pain management.9 Research has provided both strong and weak evidence to suggest that mind-body modalities, acupuncture, dietary supplements, and movement therapies are effective approaches for pain,10 often with equivalent or superior efficacy to current medical treatment and far fewer side effects.11-14 Further, integrative pain management has been proposed as primary prevention for opioid misuse.13 Despite evidence supporting integrative interventions for pain management, they are yet to be widely implemented. As far back as 2007, the American College of Physicians (ACP) guidelines for low back pain included integrative therapies.15 However, a 2013 survey reported that practitioners had not adopted these recommendations in their practices.8,16
Education for Chronic Pain Management
The need for increased and better education for pain management was delineated by the Institute of Medicine in 2011.17 Factors detracting from effective pain management include negative attitudes modeled by educators toward chronic pain patients.18 Medical student, resident, and clinician self-efficacy and attitudes toward chronic pain patients tend to be negative; previously characterized as part of the hidden curriculum taught in medical training.19 Core educational interventions have primarily focused on opioid education, deprescribing, and addiction management. The most effective form of educational intervention has not yet become clear. In a 2012 survey of practicing physicians, almost half reported unsatisfactory training for chronic pain management or opioid dependence.20 The mean number of hours taught in medical school on pain management is 11 (range 1-31 hours).21 A study of family medicine program directors found residencies provide an average of 33 hours of pain management education (range 2-180 hours). Greater time was associated with directors’ belief that there are effective nonopioid pain treatments.22 Five states require all or nearly all physicians to obtain continuing medical education (CME) on pain management and controlled substance prescribing. Only 22 states require at least some physicians to obtain such training.23
A successful, innovative, educational program in Canada (the Ontario Extension for Community Healthcare Outcomes) demonstrated a weekly 2-hour case-based video conference significantly increased clinician self-efficacy for chronic pain knowledge and management and opioid prescribing. Most (96%) of clinicians and allied health practitioners who completed the postsurvey stated it was a worthwhile experience.24
In Massachusetts, an online pain curriculum was evaluated for change in knowledge and attitudes with clinicians who recently treated chronic noncancer pain patients. Both the intervention (Managing Addiction and Pain in Primary Care course) and the control groups (any online CE pain course) improved significantly on pain practice behaviors and decreased in negative attitudes and reluctance to use opioids effectively when needed. This study demonstrates continuing education on pain management for clinicians is useful and effective.25 Notably, online education allows for more effective distribution and scalability.26
The Need for Integrative Pain Management Education
While these interventions make a strong case for education, very little evidence exists on the effectiveness of integrative pain management education. An Oregon survey revealed clinicians frequently feel they do not have nonmedication options for chronic pain patients, with concurrent belief that opioid medications are not effective for many patients.27 Primary care clinicians did not consider acupuncture as a first line of care despite patients’ perception that acupuncture was useful for short-term pain improvement. While some patients are resistant to acupuncture due to a fear of needles; one study found some patients are able to overcome their fear in their willingness to try anything for pain relief. In addition, physicians were able to reduce needle aversion by demonstrating painlessness or offering a simpler treatment.28
The opioid epidemic, increase in chronic pain, and lack of clinician knowledge and self-efficacy on pain management all lead to a central question: how to educate practitioners on chronic pain management, and more specifically, integrative pain management? To address this issue, we developed an 11-hour online integrative pain management curriculum for residents and practicing clinicians. The purpose of this study was to determine the effect of the course on resident and faculty knowledge and attitudes toward chronic pain management and the feasibility of delivering integrative pain education online to reach to a large group of graduate medical education institutions.
Course Description
The Integrative Pain Management (IPM) course is an 11-hour online course with a hybrid of written, video, and clinical case content. One of the first of its kind, the course was developed in 2017 by experts in integrative pain management at the Andrew Weil Center for Integrative Medicine. IPM examines current pain management, the differing pathophysiology of acute vs chronic pain, evidence-based integrative therapies, and clinical applications. The evidence for a wide variety of integrative modalities is described including nutritional approaches, mind-body therapies, manual therapies, acupuncture, cannabis, etc, as well as an hour devoted to strategies for deprescribing opiate medications. Since access to and cost of IM modalities is a concern for many patients, tools and inexpensive resources are provided. Clinicians can provide many of the therapies covered in the course. This study is the first to test the efficacy of the content and delivery of this course.
Sites and Participants
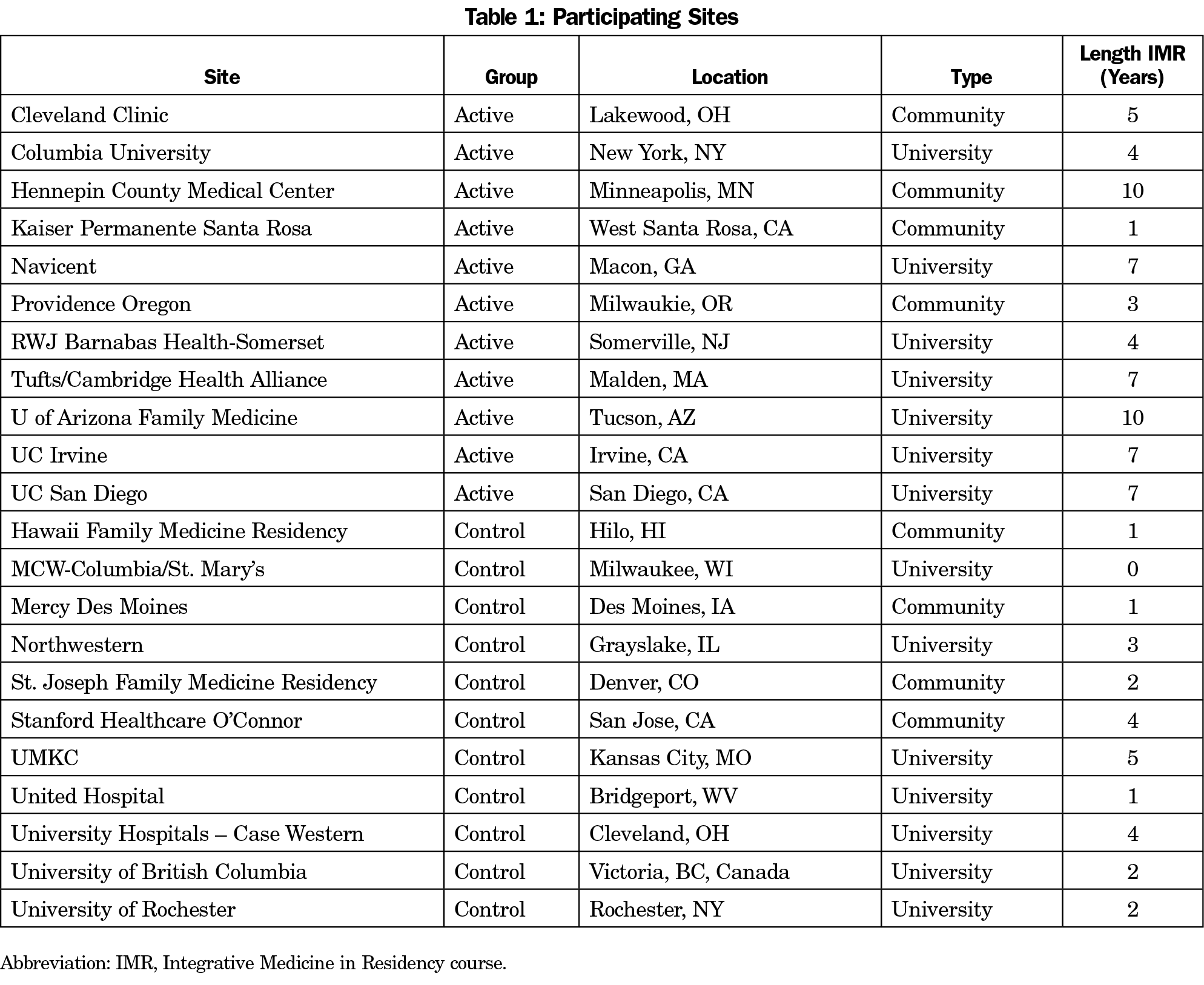
Participation in the IPM study was offered to current family medicine residencies participating in a collaborative educational program (63 sites): Integrative Medicine in Residency (IMR).29 The IMR is a 200-hour, competency-based, interactive, online IM curriculum designed for incorporation into primary care residency education. Topics include nutrition, physical activity, mind-body medicine, spirituality, botanicals, manual medicine, and other IM interventions. Active site selection was based primarily on length of time participating in IMR. Eleven of 17 sites invited agreed to participate in the study. The 11 control sites were from the remaining IMR sites, including those that declined participation as an active site. Table 1 shows site descriptions. Active sites had been participating in the IMR longer than control sites (average 6 years vs 2 years). Seven of the sites in both groups were university-based residencies; residency size30 was comparable between groups. Active sites had more learners enrolled in the IMR (average 14 learners, range 4-36) than the control sites (average 9, range 0-33). Residents, faculty, fellows and other staff were eligible to participate in the study. Participants in both groups received a $10 Amazon gift card for completing each assessment (pre/posttest). Control group participants did not receive an educational activity but completed pre- and posttest assessments in the same timeframe as active participants. The University of Arizona Institutional Review Board approved the study.
Measures
Course Completion. Course completion required completing all of the course content (30 modules) and passing a medical knowledge test with a score of at least 70%. Participants were given three attempts to pass the test.
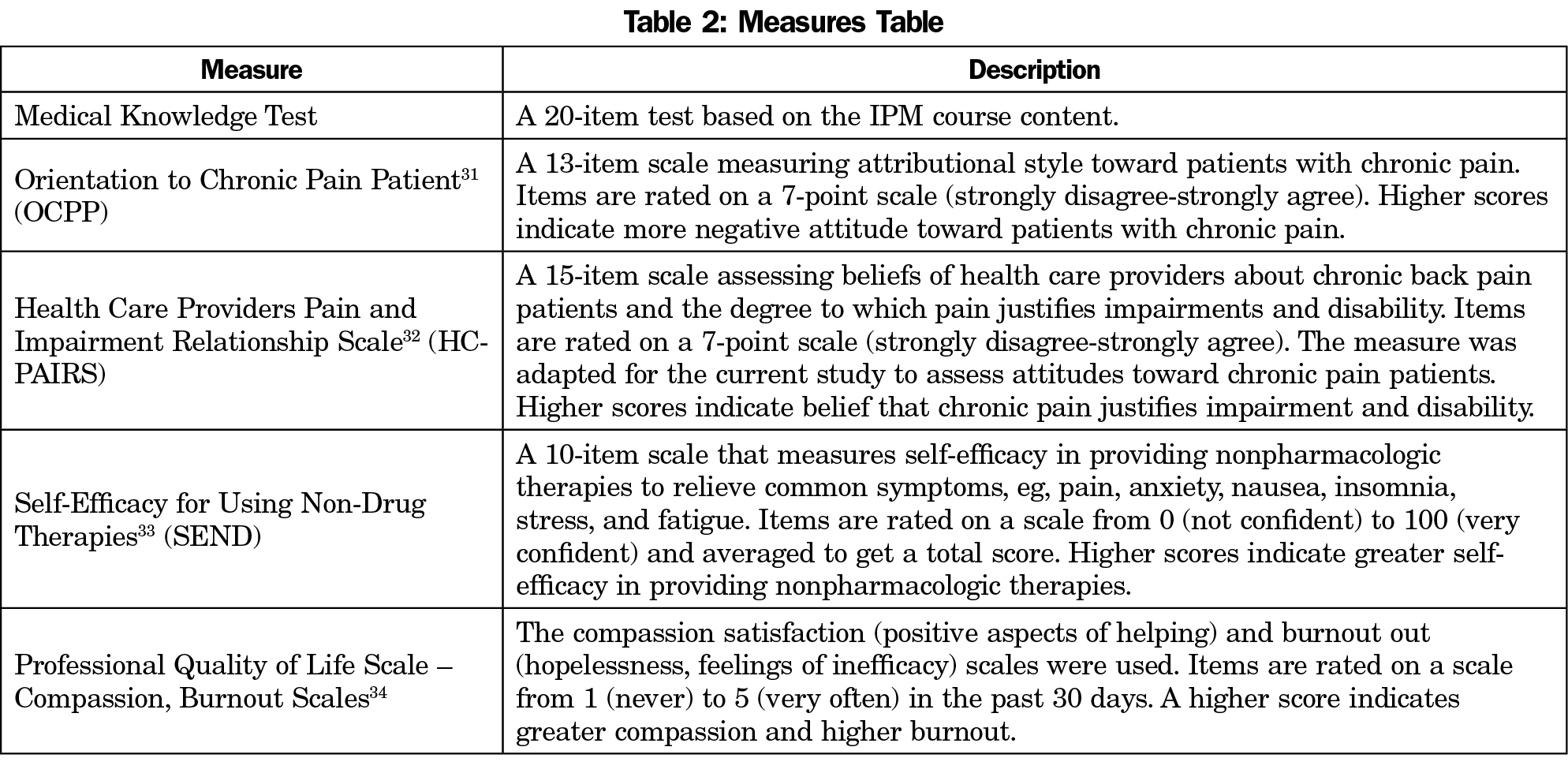
Impact on Attitudes and Knowledge. A brief survey to obtain role, credentials, and institution was administered. Clinician attitude and medical knowledge were assessed before and after the course. Table 2 describes the measures.31-34
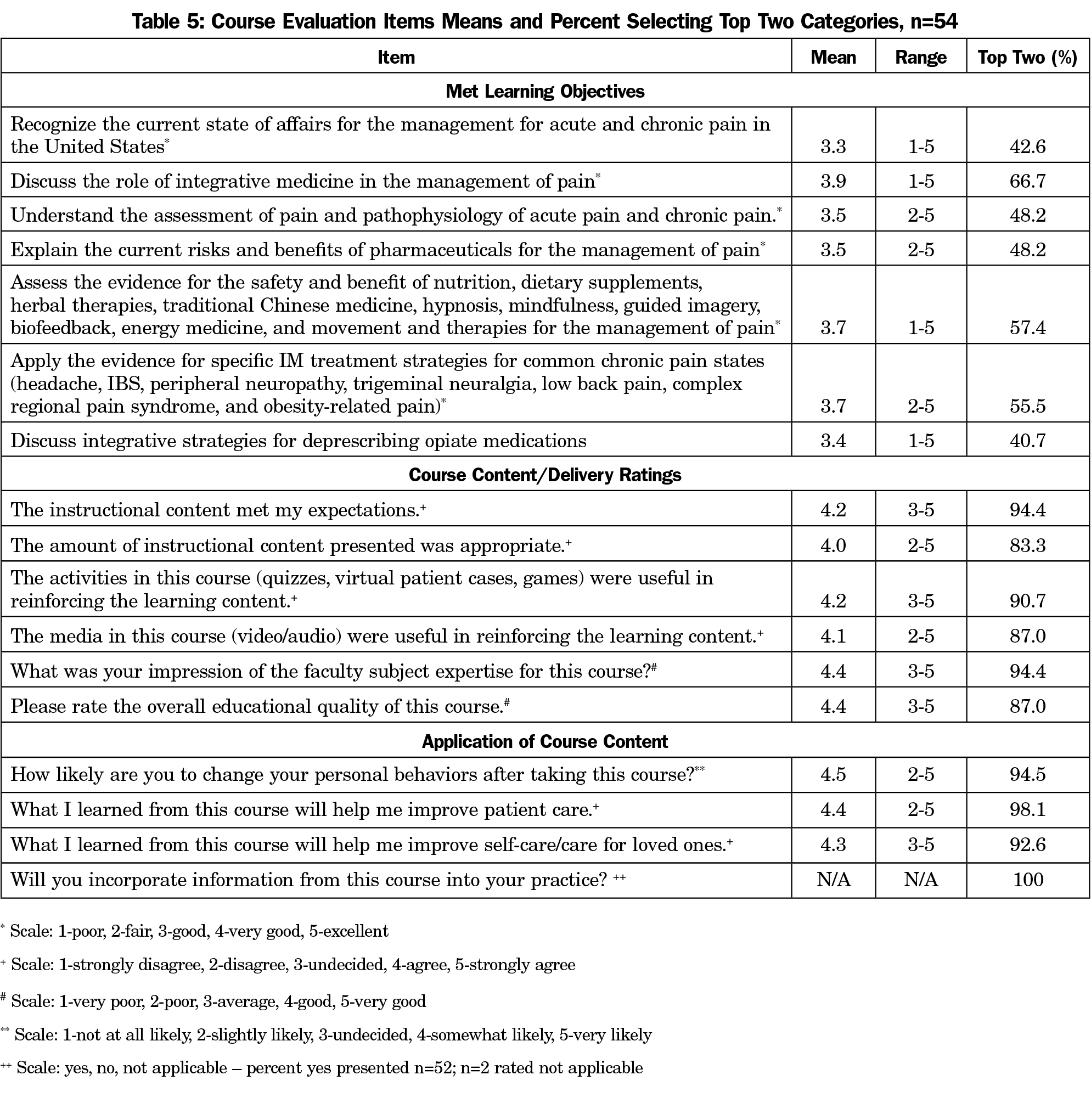
Course Evaluation. A course evaluation survey was administered upon course completion. The survey consisted of 24 items assessing reasons for taking the course, learning objectives, course content and delivery, and application to clinical practice and personal life. Items were rated on a 5-point scale from 1 (least favorable) to 5 (most favorable) and yes/no. We included three open-ended questions to query what participants found most or least useful/relevant, and how they planned to incorporate the content into practice. One item evaluated time to complete the course.
Statistical Approach
Descriptive statistics are presented for participant characteristics, completion and course evaluation results. We conducted separate χ2 analyses to examine completion by participant characteristics. To compare change in medical knowledge and attitude by group we conducted repeated measures general linear models. We conducted post hoc comparisons utilizing Bonferroni corrections on significant time by group interactions. Time (pre/post) by group (active, control) interactions indicate that change over time varies based on group membership. We used IBM SPSS Statistics Desktop V25.0 (Armonk, New York) to perform analyses.
Participants
Of the 181 IMR faculty and residents listed as potential active group participants by site leaders, 125 logged into the course. Participants (n=111 with data) were primarily residents (n=51, 46%) or faculty (n=45; 41%). The remaining participants were nurse practitioners (n=6, 5%), Fellows (n=4, 4%), or other roles (RNs [n=2], RN manager [n=1], clinician [n=1], consultant [n=1]). Almost half of the residents (n=22; 46%) were postgraduate (PG) year 2, 15 (31%) were PG year 1, and 11 (23%) PG year 3. Most participants had an MD/DO degree (n=96, 87%).
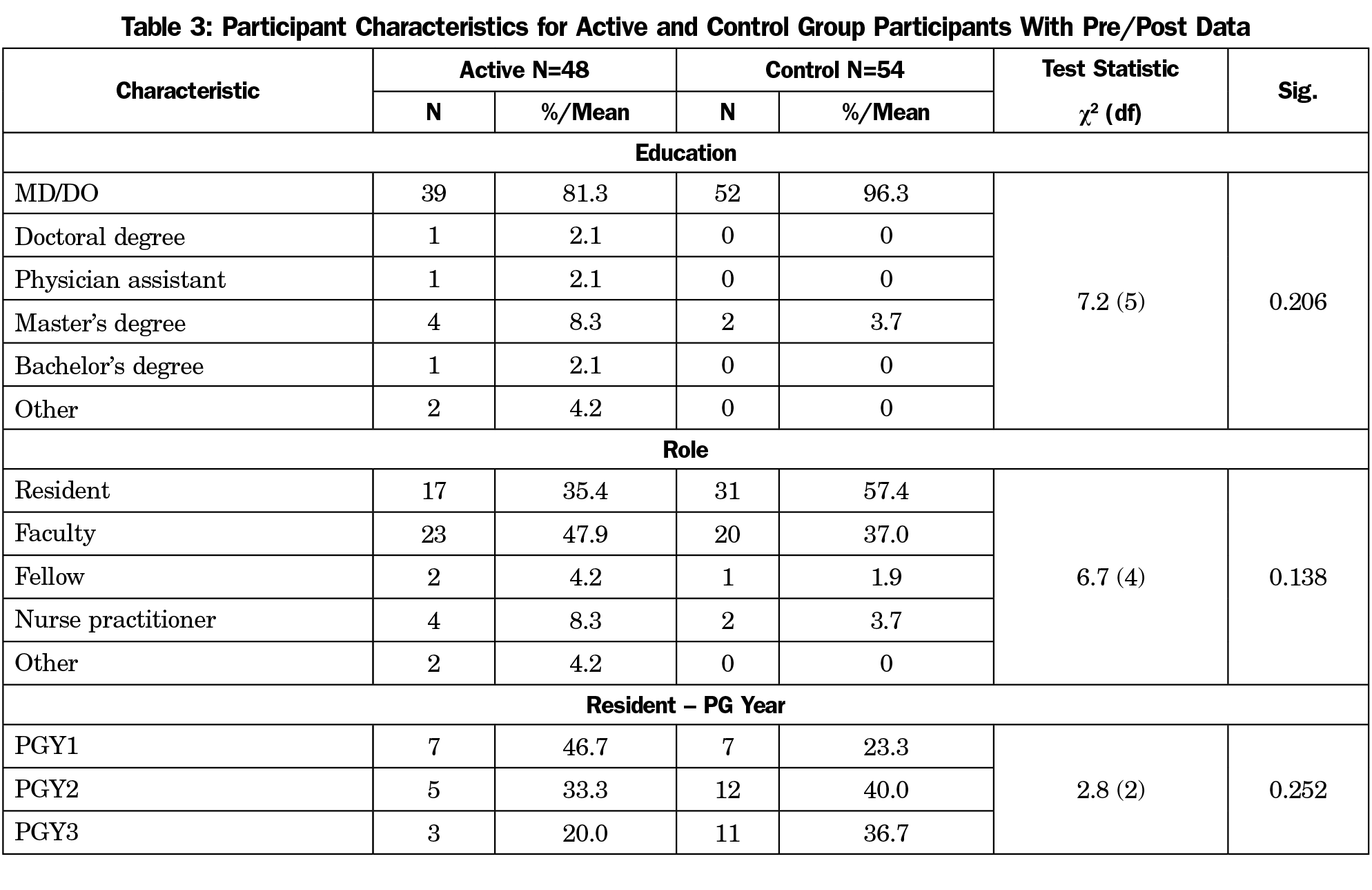
Of the potential control participants (n=193), 87 consented and 54 completed pre- and posttest assessments. Most had an MD/DO degree (n=52, 96.3%) and more than half were residents (n=31, 57.4%). There was no statistically significant difference in characteristics between participants with pretest only and those with pre- and posttest data. No difference was found in participant characteristics between active and control group participants with pre- and posttest assessments (Table 3).
Completion
Of the 125 participants who logged into the course, 34.4% (n=43) completed the it. Participants who did not complete the course completed an average of 10 of the 30 modules (range 0-29 modules). Ten participants completed 29 modules; however, they did not pass (n=7) or take the test (n=3). Faculty were more likely to complete the course than residents (χ2[1]=6.7; P=.01; faculty n=23/45; 51.1% vs residents n=13/51; 25.5%). Pre/post assessment data was available for 40 of the 43 completers and 8 noncompleters (completed at least 75% content).
Change in Medical Knowledge, Attitude, Burnout, and Compassion
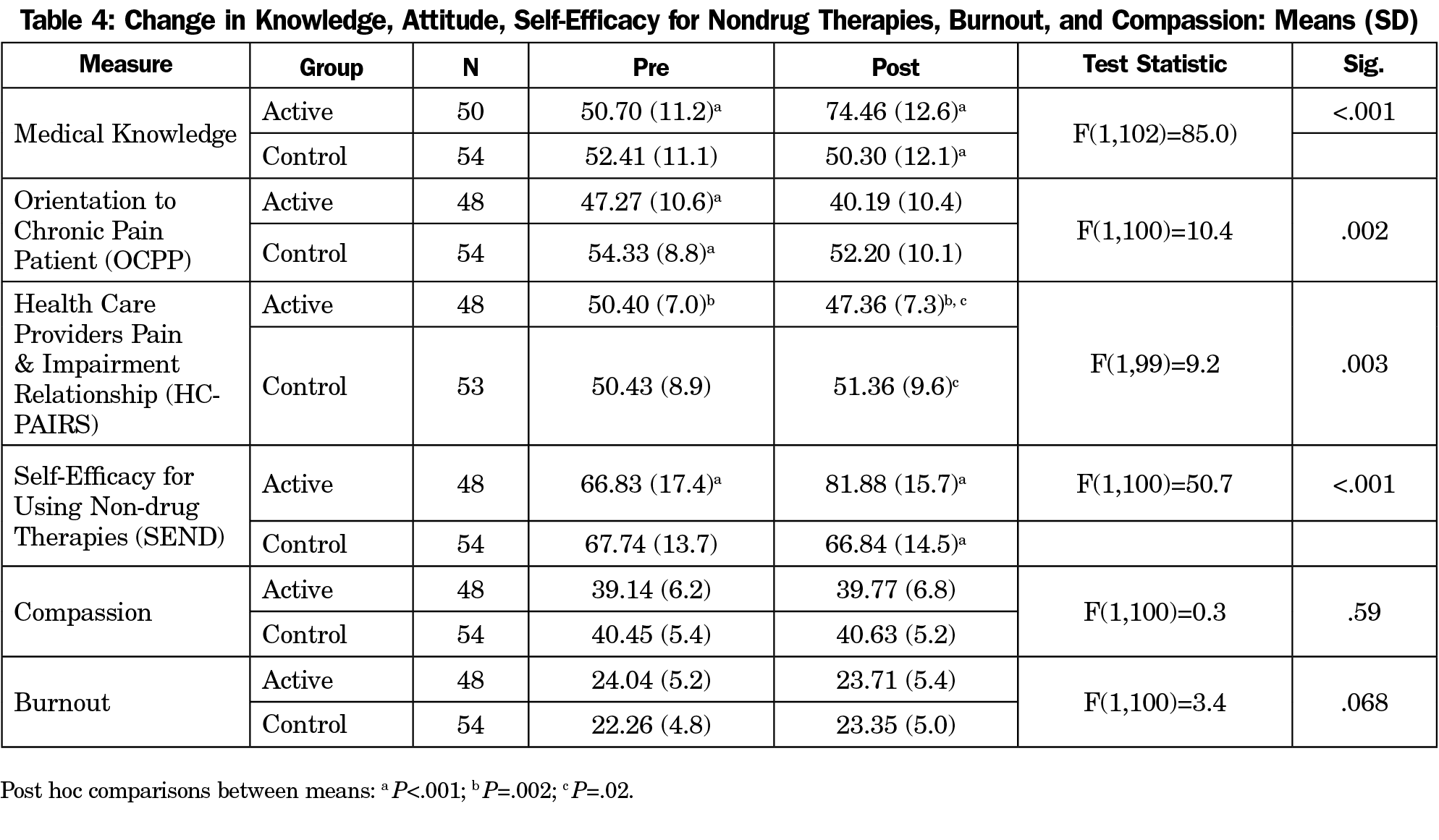
Table 4 shows the results. The time by group interaction for medical knowledge was significant (P<.001). In posthoc comparisons, the active group increased in medical knowledge from pre- to posttest, while the control group did not change from pre- to posttest. Medical knowledge was significantly higher at posttest for the active group compared to the control group. Since the active group was given three attempts to pass the posttest, active first-attempt scores (n=51) were compared to the control group posttest scores (n=57). Active residents scored significantly higher than control residents (t(106)=-7.2; P<.001; Mean±SD 67.8%±0.13 vs 49.9%±0.12). Most active participants (n=32/51, 63%) passed on the first attempt; 15 (29%) had two attempts and four (8%) had three attempts.
The time by group interaction was statistically significant for Orientation to Chronic Pain Patient (OCPP), Health Care Providers Pain and Impairment Relationship Scale (HC-PAIRS), and Self-Efficacy for Using Non-Drug Therapies (SEND) measures. The posthoc comparisons results were comparable for HC-PAIRS and SEND. A statistically significant improvement from pre- to posttest was observed for the active group but not the control group, indicating the active group improved over time while the control group did not. The active group had a significantly more positive attitude and greater self-efficacy at posttest than the control group. However, in posthoc comparisons for OCPP, a statistically significant difference between groups was found at the pretest (P<.001). Active participants had a more positive attitude toward pain patients. We conducted an analysis of covariance controlling for pretest. We found a statistically significant difference (F[1]=19.2; P<.001) between groups was found at posttest (means adjusted for pretest active=42.9, SE=1.0 vs control 49.8, SE=1.1) indicating that even when controlling for the baseline difference in attitude, the active group had a more positive attitude toward pain patients at posttest than control group participants. Burnout and compassion interactions were not significant.
Course Evaluation
Fifty-four participants completed the evaluation survey. Of these, 43 completed the course. Of the 11 who did not complete the course, 10 completed 29 modules and 1 completed 20 modules.
Reasons for Taking Course. Most participants indicated they were taking the course for personal knowledge/learning (83.3%) or to apply to clinical practice (77.8%). More than half (57.4%) indicated they were taking the course to meet continuing education requirements. Ten participants (18.5%) indicated they were taking the course due to health concerns for self or loved one.
Met Objectives. Table 5 shows the average rating and percent endorsing the top two rating categories (4-5). In terms of meeting learning objectives, the average ratings ranged from 3.3 (current state of pain management) to 3.9 (role of IM in pain management).
Course Content/Delivery. The average ratings ranged from 4.0 (instructional content amount) to 4.4 (faculty expertise, overall quality). Five participants (9.3%) felt there was bias toward a product/company, specifically, cannabinoid/marijuana recommendations and HeartMath.35 We coded open-ended responses for themes. In terms of most useful (n=44), the medical cannabis section (n=14) was mentioned most frequently, followed by nonpharmacological modalities (n=8). Nutrition recommendations (n=6), cases (n=5), and pediatric pain (n=5), were also mentioned. For the least useful comments (n=30), most frequently mentioned was the repetitiveness of some course content (n=7) across multiple diagnoses, eg, “Several sections explaining the same modalities again (hypnosis, massage, etc...).”
Time to Complete. Twenty participants (37%) completed the course in 12 hours or less, 18 (33%) reported 13-18 hours and 16 (30%) indicated the course took at least 19 hours to complete.
Application of Course Content. Participants rated the application items very highly. Ratings ranged from 4.3 (improve self-care/care for loved one) to 4.5 (change personal behaviors), with 93%-98% endorsing the top two response categories. All participants responded they would incorporate course information into their practice. Comments concerning incorporating content into practice (n=43) mentioned acquiring tools for treating pain (n=35), eg, “am more knowledgeable about the mind-body techniques, acupuncture, chiropractor, manual manipulation and will be more likely to recommend it.” Specific approaches mentioned included supplements (n=8), botanicals (n=6), mind-body (n=3), etc. Additional comments included desire to utilize nonpharmacological approaches (n=6), more confidence to recommend nonpharmacological approaches (n=4), patient education options (n=3), and knowledge of evidence-based approaches (n=3).
Results of this trial reveal that an 11-hour online course was effective in improving medical knowledge, enhancing attitudes toward chronic pain patients, and increasing sense of self-efficacy around the use of nonpharmacologic therapies. Satisfaction with course content and delivery methods was high, with 83.3%-94.4% of participants ranking the top categories. In addition, 92.6%-94.5% of participants believed the course would help them improve patient care and self-care. These results suggest that this IPM course can serve as an important component in a broad strategy to educate clinicians about nonpharmacological tools for managing chronic pain.
Course completion was 34.4% of total participants. Faculty (51.1% completion) were more likely to complete the course than residents (25.5% completion). The short study timeframe may have limited residents’ ability to complete the curriculum, given competing demands.
Medical knowledge improved by 23.8% in the experimental group and was unchanged in the controls. One participant comment regarding knowledge gained was, “I am more knowledgeable about the mind body techniques, acupuncture, chiropractor, manual manipulation and will be more likely to recommend it.” Similar comments were made concerning use of nutrition and dietary supplements. The change in learner attitudes is especially remarkable. One participant comment captured this aptly, “Mostly a wakeup call to remember compassionate care of chronic pain patients, rather than feeling burned out treating them.”
Strengths of the study include the large number of participants, the in-depth IPM education, multisite demonstration of feasibility and impact, inclusion of control sites, and use of a common curriculum for training residents and faculty.
Limitations include the 34.4% completion rate, and that the course did not have significant impact on compassion or burnout. This may have been too much to expect from an 11-hour intervention. Notably, the course took longer to complete than the estimated 11 hours for 63% of the learners. To get a better response rate amongst residents, allocating dedicated time to complete the course may help. Multiple shorter courses may improve completion rates as this would allow residents and clinicians to focus on the integrative modalities and pain syndromes that best match their practice. Although sites were not randomized, there was no difference in residency type, participant characteristics, or baseline medical knowledge. While there was a difference in attitude toward chronic pain patients at baseline, active sites showed an improvement in attitude while control sites did not. Additionally, while the course is priced comparably to other CME courses,36 the fee could limit implementation.
Future studies needs include confirming feasibility and efficacy in non-IMR residencies. An important next step is a study assessing provider prescribing practices and resulting patient satisfaction. This is critical to determining if the learners believe that implementing practice change would not be detrimental to patients’ chronic pain. That is a much more complex, although vital study.
Although the body of evidence supporting IM has grown, and acknowledgement of its value confirmed by multiple agencies, few providers are trained in IPM. This IPM course holds significance as it is delivered entirely online. The course is scalable to reach large numbers of physicians, nurses, dentists, and pharmacists to effectively train future generations of providers, especially those practicing in rural and underserved areas away from academic institutions. As states begin to require CE for chronic pain, this course could meet the needs of large numbers of learners. The course is available for CE online to residencies, health care systems, and practicing physicians.36 Ideally, this IPM course will reach residents and practicing clinicians, thereby increasing clinicians’ tools for managing chronic pain and easing the suffering of the patients they serve.
Acknowledgments
The authors thank all the residents and faculty who participated in the IPM study, and Janice Curtis for her invaluable assistance in preparing this manuscript.
Ethical Approval: The University of Arizona Institutional Review Board (IRB) granted approval for this study.
References
- Dahlhamer J, Lucas J, Zelaya C, et al. Prevalence of chronic pain and high-impact chronic pain among adults - United States, 2016. MMWR Morb Mortal Wkly Rep. 2018;67(36):1001-1006. https://doi.org/10.15585/mmwr.mm6736a2
- Sites BD, Beach ML, Davis MA. Increases in the use of prescription opioid analgesics and the lack of improvement in disability metrics among users. Reg Anesth Pain Med. 2014;39(1):6-12. https://doi.org/10.1097/AAP.0000000000000022
- Stoicea N, Costa A, Periel L, Uribe A, Weaver T, Bergese SD. Current perspectives on the opioid crisis in the US healthcare system: A comprehensive literature review. Medicine (Baltimore). 2019;98(20):e15425. https://doi.org/10.1097/MD.0000000000015425
- Rudd RA, Seth P, David F, Scholl L. Increases in Drug and Opioid-Involved Overdose Deaths - United States, 2010-2015. MMWR Morb Mortal Wkly Rep. 2016;65(50-51):1445-1452. https://doi.org/10.15585/mmwr.mm655051e1
- U.S. Department of Health and Human Services. What is the U.S. Opioid Epidemic? https://www.hhs.gov/opioids/about-the-epidemic/index.html. 2018. Accessed October 30, 2019.
- García MC, Heilig CM, Lee SH, et al. Opioid prescribing rates in nonmetropolitan and metropolitan counties among primary care providers using an electronic health record system - United States, 2014-2017. MMWR Morb Mortal Wkly Rep. 2019;68(2):25-30. https://doi.org/10.15585/mmwr.mm6802a1
- Kuehn B. Declining opioid prescriptions. JAMA. 2019;321(8):736.
- Rickert J, Devlin K, Krohn K. Comprehensive care of pain: developing systems and tools to improve patient care and resident education. Int J Psychiatry Med. 2016;51(4):337-346. https://doi.org/10.1177/0091217416659270
- Nahin RL, Boineau R, Khalsa PS, Stussman BJ, Weber WJ. Evidence-Bbased evaluation of complementary health approaches for pain management in the United States. Mayo Clin Proc. 2016;91(9):1292-1306. https://doi.org/10.1016/j.mayocp.2016.06.007
- Lin YC, Wan L, Jamison RN. Using integrative medicine in pain management: an evaluation of current evidence. [Review]. Anesth Analg. 2017;125(6):2081-2093. https://doi.org/10.1213/ANE.0000000000002579
- Tick H, Chauvin SW, Brown M, Haramati A. Core competencies in integrative pain care for entry-level primary care physicians. Pain Med. 2015;16(11):2090-2097. https://doi.org/10.1111/pme.12818
- Qaseem A, Wilt TJ, McLean RM, Forciea MA; Clinical Guidelines Committee of the American College of Physicians. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514-530. https://doi.org/10.7326/M16-2367
- Antman KH, Berman HA, Flotte TR, Flier J, Dimitri DM, Bharel M. Developing core competencies for the prevention and management of prescription drug misuse: a medical education collaboration in Massachusetts. Acad Med. 2016;91(10):1348-1351. https://doi.org/10.1097/ACM.0000000000001347
- Giannitrapani K, Holliday J, Miake-Lye I, Hempel S, Taylor SL. Synthesizing the strength of the evidence of complementary and integrative health therapies for pain. Pain Med. 2019;20(9):pnz068. https://doi.org/10.1093/pm/pnz068
- Chou R, Qaseem A, Snow V, et al; Clinical Efficacy Assessment Subcommittee of the American College of Physicians; American College of Physicians; American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478-491. https://doi.org/10.7326/0003-4819-147-7-200710020-00006
- Mafi JN, McCarthy EP, Davis RB, Landon BE. Worsening trends in the management and treatment of back pain. 2013;1(17):1573-1581. https://doi.org/10.1001/jamainternmed.2013.8992
- Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Academies Press; 2011. https://www.ncbi.nlm.nih.gov/books/NBK91497/. Accessed October 30, 2019.
- Rice K, Ryu JE, Whitehead C, Katz J, Webster F. Medical trainees’ experiences of treating people with chronic pain: a lost opportunity for medical education. Acad Med. 2018;93(5):775-780. https://doi.org/10.1097/ACM.0000000000002053
- Hafferty FW, Franks R. The hidden curriculum, ethics teaching, and the structure of medical education. Acad Med. 1994;69(11):861-871. https://doi.org/10.1097/00001888-199411000-00001
- Keller CE, Ashrafioun L, Neumann AM, Van Klein J, Fox CH, Blondell RD. Practices, perceptions, and concerns of primary care physicians about opioid dependence associated with the treatment of chronic pain. Subst Abus. 2012;33(2):103-113. https://doi.org/10.1080/08897077.2011.630944
- Mezei L, Murinson BB; Johns Hopkins Pain Curriculum Development Team. Pain education in North American medical schools. J Pain. 2011;12(12):1199-1208. https://doi.org/10.1016/j.jpain.2011.06.006 PMID:21945594
- Zoberi K, Everard KM. Teaching chronic pain in the family medicine residency. Fam Med. 2018;50(1):22-27. https://doi.org/10.22454/FamMed.2018.134727
- Davis CS, Carr D. Physician continuing education to reduce opioid misuse, abuse, and overdose: many opportunities, few requirements. Drug Alcohol Depend. 2016;163:100-107. https://doi.org/10.1016/j.drugalcdep.2016.04.002
- Furlan AD, Zhao J, Voth J, et al. Evaluation of an innovative tele-education intervention in chronic pain management for primary care clinicians practicing in underserved areas. J Telemed Telecare. 2019;25(8):484-492. https://doi.org/10.1177/1357633X18782090
- Trudeau KJ, Hildebrand C, Garg P, Chiauzzi E, Zacharoff KL. A randomized controlled trial of the effects of online pain management education on primary care providers. Pain Med. 2017;18(4):680-692.
- Dunleavy G, Nikolaou CK, Nifakos S, Atun R, Law GCY, Tudor Car L. Mobile digital education for health professions: systematic review and meta-analysis by the Digital Health Education Collaboration. J Med Internet Res. 2019;21(2):e12937. https://doi.org/10.2196/12937
- Penney LS, Ritenbaugh C, DeBar LL, Elder C, Deyo RA. Provider and patient perspectives on opioids and alternative treatments for managing chronic pain: a qualitative study. BMC Fam Pract. 2017;17(1):164. https://doi.org/10.1186/s12875-016-0566-0
- Ledford CJW, Fisher CL, Moss DA, Crawford PF III. Critical factors to practicing medical acupuncture in family medicine: patient and physician perspectives. J Am Board Fam Med. 2018;31(2):236-242. https://doi.org/10.3122/jabfm.2018.02.170381
- Lebensohn P, Kligler B, Brooks AJ, et al. Integrative medicine in residency: feasibility and effectiveness of an online program. Fam Med. 2017;49(7):514-521.
- Accreditation Council for Graduate Medical Education. ACGME Advanced Program Search. https://apps.acgme.org/ads/Public/Programs/Search. Accessed October 18, 2018.
- Weinstein SM, Laux LF, Thornby JI, et al. Medical students’ attitudes toward pain and the use of opioid analgesics: implications for changing medical school curriculum. South Med J. 2000;93(5):472-478. https://doi.org/10.1097/00007611-200093050-00006
- Rainville J, Bagnall D, Phalen L. Health care providers’ attitudes and beliefs about functional impairments and chronic back pain. Clin J Pain. 1995;11(4):287-295. https://doi.org/10.1097/00002508-199512000-00006
- Kemper KJ, Gascon G, Mahan JD. Two new scales for integrative medical education and research: confidence in providing calm, compassionate care scale (CCCS) and self-efficacy in providing non-drug therapies (SEND) to relieve common symptoms. Eur J Integr Med. 2015;7(4):389-395. https://doi.org/10.1016/j.eujim.2014.10.010
- Stamm B. The Concise ProQOL Manual. 2nd ed. Pocatello, ID: ProQOL.org; 2010. https://proqol.org/ProQOl_Test_Manuals.html. Accessed October 30, 2019.
- HeartMath. https://www.heartmath.com/. Accessed October 25, 2018.
- University of Arizona Andrew Weil Center for Integrative Medicine. Integrative Pain Management. https://integrativemedicine.arizona.edu/online_courses/pain_management.html. Accessed May 24, 2019.
Lead Author
Ann Marie Chiasson, MD, MPH
Affiliations: University of Arizona Andrew Weil Center for Integrative Medicine, Tucson, AZ
Co-Authors
Audrey J. Brooks, PhD - University of Arizona Andrew Weil Center for Integrative Medicine, Tucson, AZ
Mari Ricker, MD - University of Arizona Andrew Weil Center for Integrative Medicine, Tucson, AZ
Patricia Lebensohn, MD - University of Arizona Andrew Weil Center for Integrative Medicine, Tucson, AZ
Mei-Kuang Chen, PhD - University of Arizona Andrew Weil Center for Integrative Medicine, Tucson, AZ
Victoria Maizes, MD - University of Arizona Andrew Weil Center for Integrative Medicine, Tucson, AZ
Corresponding Author
Ann Marie Chiasson, MD, MPH
Correspondence: University of Arizona Andrew Weil Center for Integrative Medicine, PO Box 245153, Tucson, AZ 85724-5153. 520-626-3489.
Email: chiasson@email.arizona.edu
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.