Background and Objectives: Inadequate resources have led to family medicine research divisions at varying stages of development. The purpose of this analysis was to identify the factors that family medicine research “bright spot” departments perceive to be crucial to their success.
Methods: In this qualitative analysis, we identified bright spot dimensions and used a snowball sampling approach to identify medical school-based departments considered to be research bright spots. With 16 leaders from eight departments, we conducted semistructured interviews, covering historical events, leadership, partnerships, mentors, faculty selection, and training. We recorded and transcribed interviews and used a template-driven approach to data analysis, iteratively defining and modifying codes. At least two reviewers independently coded each interview, and coding discrepancies were discussed until consensus was reached.
Results: We identified the following themes: (1) Leadership was committed to research; (2) Research was built around teams of researchers; (3) Interdisciplinary teams facilitated by partnerships allowed the department to tackle complex problems; (4) The convergence of researchers and clinicians ensured that the research was relevant to family medicine; (5) Departments had cultures that engendered trust, leading to effective collaboration; (6) These teams were composed of intrinsically motivated individuals supported by mentorship and resources; (7) When deciding which questions to pursue, departments balanced the question’s alignment with the individual researcher’s passion, relevance to family medicine, and fundability.
Conclusions: A commitment to research from an engaged chair, partnerships, integrating front-line clinicians, and supporting intrinsically motivated individuals were important for bright spots. Applying these concepts may be an important strategy for generating knowledge.
The family medicine research enterprise suffers from a gap between the haves and the have-nots.1-3 According to an Association of Departments of Family Medicine (ADFM) survey, 43% of departments had no or minimal research capacity compared to 22% with significant or extensive capacity. This disparity is reflected in National Institutes of Health (NIH) funding for family medicine, which is simultaneously small and concentrated at three departments.4,5 Participation in NIH Clinical Translational Science Awards (CTSAs) has been similarly inconsistent, even though family medicine research aligns with the program’s focus on community engagement and practice-based research. While family medicine faculty held leadership positions in a third of CTSAs, a majority of departments were not involved either because their institution lacked a CTSA or the department lacked expertise.6,7
The barriers to enhanced research in family medicine are numerous. Brocato and Mavis found that 80% of family medicine faculty spend a half day or less on research and, on average, published less than once per year.8 Others have cited inadequate infrastructure, the high cost of launching investigators, weak culture, insufficient funding, and scarce research training across residents, fellows, and faculty.9-11 Two recent initiatives have been launched to address these barriers. The Building Research Capacity program—an initiative between the ADFM and the North American Primary Care Research Group (NAPCRG)—provides capacity building assistance to all family medicine departments and residency programs.1 Similarly, the Family Medicine for America’s Health (FMAHealth) Research Tactic Team aimed to galvanize the research community.12
Scholars have sought to identify characteristics and develop models that describe productive research organizations. Using surveys and interviews of faculty at the University of Minnesota, Carole Bland developed a model built on individual, institutional, and leadership characteristics.13,14 This research describes the “integration and interplay” of individual and institutional features with a synthesis that is dependent on effective leaders.14 Bland writes about individuals with passion who have been aided by formal mentoring and protected time. At the institutional level, productivity was facilitated by a safe culture built to test new ideas, a high degree of cooperation, and a vibrant network of colleagues. An ADFM project capturing lessons from successful family medicine departments identified similar themes and concluded that chair leadership, chair investment, team development, and network opportunities were critical for productive departments.11 Our objective was to determine the extent to which the Bland model applied to family medicine and identify the factors that family medicine research bright spots perceive to be crucial to their success with the hope that these lessons can be applied across the discipline to stimulate research activity.
In this qualitative analysis, we conducted 30-minute, semistructured interviews with leaders at family medicine research bright spots. To define bright spots, we consulted content experts, including department chairs, the FMAHealth Research Tactic Team, the Robert Graham Center Research Team, the American Board of Family Medicine Research Team, the Society of Teachers of Family Medicine’s Research Committee, the NAPCRG Research Advocacy Committee, and the ADFM Research Development Committee. Based on their input, we identified dimensions of family medicine research bright spots, which experts described as having high impact (outside of family medicine, in the popular press, or changes policy) and conducting research that is aligned with family medicine principles. These bright spots have high productivity or high and sustained grant funding with a diversity of funding streams and researchers. They draw from a robust network of partners, including practice-based research networks. They are exemplars in training researchers, mentoring productive faculty for their own departments and the discipline as a whole. Experts also described idea bright spots that have seeded the discipline with important methods or ideas and genealogical bright spots, which were historically important for the discipline.
Data Sources
Starting from these experts and applying the above dimensions, we used snowball sampling to identify medical school-based departments they considered bright spots and interviewed two key informants (typically a current or former chair and a research director) from eight departments (Table 1). These interviews were recorded and transcribed. We used questions adapted from Carol Bland’s work, The Research-Productive Department, specifically asking about historical events, leadership, partnerships, mentoring, faculty selection, and training.13
Analytic Plan
We used a template-driven approach to analysis. Using a priori hypotheses, we started with the three categories and codes (individual, institutional, and leadership) embedded within Bland’s model. During the coding process, these codes were modified and refined in an iterative fashion, and emergent codes were added. All of the authors participated in the coding process and agreed on the codes and code definitions in the initial and final codebooks. At least two reviewers independently coded each interview, and coding discrepancies were discussed until consensus was reached. Themes arising from codes and subcodes were similarly reviewed by two reviewers with discrepancies discussed until consensus was reached.
The American Academy of Family Physicians Institutional Review Board approved this protocol.
Interviewees discussed successful research endeavors at system, institutional, departmental, and individual levels, which sometimes overlapped or were interdependent. At the department level, participants reflected on the importance of peer-to-peer interactions, selection of personnel, funding, and clinical integration. Additionally, these leaders discussed concepts that spanned multiple levels, such as leadership, mentorship, investment, partnership, pipeline, and the extent to which the research aligned with family medicine.
Leadership
Our respondents identified department leadership as a factor critical to success. Specifically, bright spot departments had leaders that value research and committed resources to support it (Table 2 identifies codes related to leadership and provides illustrative quotes). The chairs did not need to be researchers, but needed to understand the research process, potential sources of revenue, and infrastructure. They viewed challenges and crises within the department and institution as opportunities to conduct research. For example, one chair was asked by the institution to assume control over a failing network of primary care clinics; in addition to turning the clinics around financially, the department used the opportunity to study practice transformation. Bright spot chairs and research directors were proactive in cultivating partnerships and asking outside experts for technical assistance. While these leaders took action to support research, luck also played a role. Several acknowledged that they benefited from fortuitous circumstances, such as the chance relocation of researchers to their states and the hiring of young researchers who developed into highly productive scholars and in the process changed the trajectory of their departments and the specialty.
Teams
Bright spots understood the importance of teams to research success (Table 3 provides codes and illustrative quotes regarding the influence of teams), with respondents saying that members of teams have something “more together” than they do “separately” and that “research…is a team enterprise.” Citing the complexity of problems addressed in primary care, multiple leaders said that researchers needed connections to other researchers, preferably those with different skills and research backgrounds. The most successful researchers had extensive networks of partners within the department, within the institution, and nationally. Individuals without connections tended to have greater difficulty remaining funded. These departments were strategic about developing partnerships and identified collaborators who “have things [the department doesn’t] have.” Specifically, these partners can provide funding for researchers, technical expertise, and access to patients. Several respondents discussed nontraditional partners, such as lawyers, designers, engineers, and journalists, with one chair declaring that “family medicine is going to succeed on the strength of its partnerships and the stranger the better.” Ultimately, research success elevated the status of the department within the institution, with other departments viewing family medicine researchers as content and methods experts, seeking assistance with projects, and proposing new partnerships.
With respect to the balance between physicians and PhD researchers, there was not a consensus, with some lamenting the resources needed to train physicians to conduct research and others saying that PhDs lack frontline clinical experience. Similarly, there was disagreement about whether these teams should be built around department-level research foci, including chronic disease prevention and management, women’s health, disability research, population health, mixed methods, and practice transformation. While some respondents indicated that having a focus facilitated collaboration and mentorship, others were more cautious, citing a failed department experiment decades ago that mandated a singular research focus.
To ensure that the research was relevant to family medicine, bright spots brought together researchers and clinicians (Table 3). Rather than just “getting on the funding hamster wheel,” these departments were concerned about how the work informs the practice of family medicine. One leader indicated that the important job as the chair was “forcing the research and clinical faculty into small spaces and not letting them away from each other.” Clinics were seen as critical “laboratories” for innovations, and some reported that funding from clinics made the research possible. This interplay was important for the relevance of the questions pursued by researchers while simultaneously developing the research skills of the clinicians. Some departments were developing programs to tap into the scholarly potential of all faculty, though there is an inherent tension. While critically important, the questions developed by clinical faculty often need refinement, are not easily funded by external sources, and draw resources away from career researchers.
The tension among fundability, relevance to family medicine, and personal passion was discussed by several respondents (Figure 1). While many acknowledged the importance of a question’s fundability for the sustainability of the research enterprise, several discussed that the defining questions for family medicine were “almost unfundable.” An additional factor was the interests of junior researchers who were often trained to pursue fundable questions in areas related to their mentors’ research. One respondent lamented that this approach may unintentionally suppress innovative, groundbreaking new ideas coming from younger researchers.
To be effective, respondents indicated that teams needed to meet a minimum size threshold and have quality peer interactions (Table 3). Given the team-based nature of research, multiple leaders said that having a critical mass was important. Similar to efforts to converge clinicians and researchers, bright spots sought to encourage interactions between researchers by physically locating them adjacent to one another, having opportunities for researchers to share their work, and creating organizational charts that encouraged collaboration.
Within this milieu, the department sought to actively build cultures that valued collaboration. Respondents mentioned that researchers that did not place value on “getting along” were less likely to be successful. The quality of interactions between team members was important because it allowed researchers to support, be held accountable to, and provide honest feedback to one another. Bright spots facilitated these interactions by building a foundation of trust. One department had retreats where researchers immersed themselves in work but also set aside time for members to “get to know each other” as people.
Identifying and Supporting Researchers
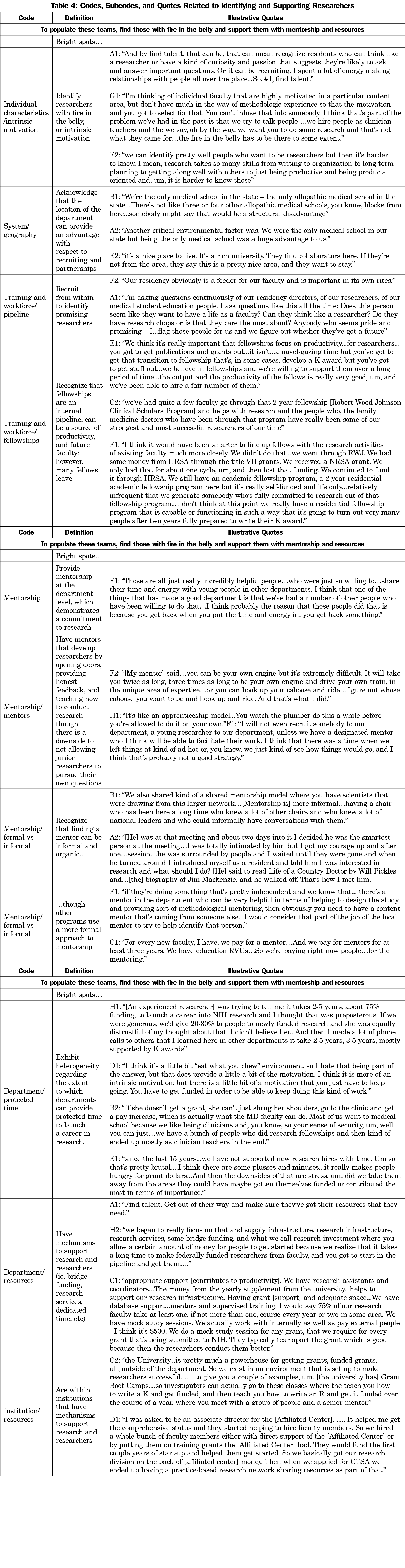
To compose these teams, bright spot departments identified passionate researchers and provided them with resources (Table 4). Bright spot leaders reported that they spent a lot of time finding talent. Specifically, they sought individuals with “fire in the belly,” which they described as intrinsic motivation, “curiosity,” and “passion.” One interviewee said that trying to transform talented faculty members into researchers was less likely to be successful without “fire in the belly.” While intrinsic motivation was important, leaders also indicated that it was insufficient in isolation without resources and further training. Once again, respondents cited luck as a factor in recruitment, specifically for those departments that were the only medical schools in their states or were in geographically desirable locations. To identify these individuals, bright spots often hired from within. There was disagreement with respect to the effectiveness of department fellowships to serve this purpose. Some found fellowships incredibly important, with one saying that the Robert Wood Johnson Clinical Scholars Program developed some of the “strongest and most successful researchers.” Others said that the fellowships infrequently generated “somebody who’s fully committed to research,” more often created “clinician teachers,” and sometimes produced faculty that left for other schools.
While every department saw mentorship as critical to faculty development, their approaches differed. Some bright spots had formal mentorship programs, assigning junior faculty to senior researchers, not hiring younger faculty without an identified mentor, and paying mentors for time spent working with junior faculty. These more formal relationships facilitated an apprenticeship model where junior faculty learned by working on the projects of their mentors. Other bright spots had more organic mentoring programs, which involved providing junior faculty with opportunities to meet and learn from national networks of senior faculty. There was also disagreement with respect to protected time to write grants. One department acknowledged that it took 2 to 5 years and 75% funding to launch an NIH research career, and multiple commented that this is the predominant model in academia. Several bright spots reported that they could not afford to provide this time; instead, the lack of a safety net helped identify those researchers with passion and motivated researchers to find and secure funding. Respondents noted that, in contrast to nonclinician researchers, clinician researchers had the ability to increase clinical effort to fund their time.
In this qualitative analysis, we found that bright spots excelled at leveraging a commitment to research from an engaged chair, cultivating partnerships, integrating frontline clinicians, developing a trusting culture among team members, and identifying and supporting intrinsically motivated individuals. While these themes were common across our sample, the approaches to attaining them were heterogeneous, suggesting the existence of multiple paths to the same destination.
Our findings both confirm and deviate from Bland’s model.13 Within our sample of family medicine bright spots, we also found that motivation at the individual level, collaborative culture at the institutional level, and a research orientation at the leadership level were all important for success. While Bland’s model does discuss interdisciplinary collaboration as an institutional feature, team-based research is not a pillar. In contrast, family medicine departments are largely built around teams of researchers. Though this study did not assess whether teams are central to non-family medicine departments, we hypothesize that team-based research has flourished in family medicine due to the pluralistic and generalist perspective of family medicine and the complexity of the problems faced in primary care. At one time, scientific discovery had been dominated by solitary scholars like Isaac Newton and Albert Einstein. A shift to teamwork has been documented across disciplines. A National Academy of Medicine report observed that 90% of all science and engineering publications have two or more authors.15 The mean number of authors increased from less than two in 1960 to three and a half in 2000.16 There was a similar increase in the percentage of papers authored by teams that spanned multiple institutions. This shift in the scientific process mirrors the shift occurring in the delivery of care and in education, where team-based care and interprofessional education have gained wider acceptance.17,18
Charged with assessing and galvanizing the family medicine research enterprise, the FMAHealth Research Tactic Team has sought to identify strategies to stimulate research across the discipline. Our findings have important lessons for all departments interested in enhancing inquiry. For example, all bright spots have non-family medicine departments that can serve as potential partners. Many of these bright spots found ways to collaborate with pediatric, obstetric/gynecology, and surgical departments. One chair said that the first step he made to enhance research was to meet researchers at other departments, find out about their questions, methods, and needs, and identify potential areas of collaboration. Second, we found that chairs within departments had tremendous influence over research capacity even if they were not researchers. Departments are often undergoing transitions and experiencing crises. The chairs at bright spots embraced these challenges as opportunities to study the impact of what they did next. Finally, departments are filled with intellectually curious, passionate educators and clinicians who have the potential to play pivotal roles in developing research capacity. Bright spots systematically identified internal scholars and connected them with training opportunities within the institution.
There are several limitations that should be considered when interpreting our findings. First, we only included bright spot departments; our findings may differ if we had interviewed additional schools. We did not include residencies or policy centers not affiliated with academic institutions, though we believe that enhancing scholarship within residencies is critical to building research capacity across the discipline. Some of these lessons may be applicable to residencies, though we hypothesize that residencies have unique challenges and opportunities. Because our definition of bright spots included research productivity and funding, our bright spots were successful at obtaining NIH funding. Excluding this dimension from the definition may have led us to interview a different set of schools and lead to different conclusions. Finally, our interviews lasted 30 minutes. Longer interviews may have allowed us to explore additional facets to these research enterprises, including financing, retention, training of senior faculty, and faculty diversity.
In summary, leveraging a commitment to research from an engaged chair, building partnerships, integrating frontline clinicians, developing a trusting culture among team members, and supporting intrinsically motivated individuals were critical factors to the development of research bright spots. These lessons can used by all family medicine departments to enhance research.
Acknowledgments
The authors thank the bright spot participants for their time and insights and members of the FMAHealth Research Tactic Team for their support and feedback.
Funding: This work was funded by a grant from Family Medicine for America’s Health.
Prior presentations: Society of Teachers of Family Medicine Annual Spring Conference, May 5-9, Washington, DC.
References
- Ewigman B, Davis A, Vansaghi T, et al. Building research and scholarship capacity in departments of family medicine: a new joint ADFM-NAPCRG initiative. Ann Fam Med. 2016;14(1):82-83. https://doi.org/10.1370/afm.1901
- Post RE, Weese TJ, Mainous AG III, Weiss BD. Publication productivity by family medicine faculty: 1999 to 2009. Fam Med. 2012;44(5):312-317.
- Bowman MA, Lucan SC, Rosenthal TC, Mainous AG III, James PA. Family medicine research in the United States from the late 1960s into the future. Fam Med. 2017;49(4):289-295.
- Cameron BJ, Bazemore AW, Morley CP. Federal research funding for family medicine: highly concentrated, with decreasing new investigator awards. J Am Board Fam Med. 2016;29(5):531-532. https://doi.org/10.3122/jabfm.2016.05.160076
- Cameron BJ, Bazemore AW, Morley CP. Lost in translation: NIH funding for family medicine research remains limited. J Am Board Fam Med. 2016;29(5):528-530. https://doi.org/10.3122/jabfm.2016.05.160063
- Ewigman B; North American Primary Care Research Group. CTSAs and family medicine research—time to get connected. Ann Fam Med. 2008;6(2):181-182. https://doi.org/10.1370/afm.828
- Ewigman B, Johnson MS, Davis A, et al; CTSA Strike Force Members of the CTSA Strike Force. An update on family medicine participation in clinical and translational science awards (CTSAs). Ann Fam Med. 2009;7(3):275-276. https://doi.org/10.1370/afm.1011
- Brocato JJ, Mavis B. The research productivity of faculty in family medicine departments at U.S. medical schools: a national study. Acad Med. 2005;80(3):244-252. https://doi.org/10.1097/00001888-200503000-00008
- Bolon SK, Phillips RL Jr. Building the research culture of family medicine with fellowship training. Fam Med. 2010;42(7):481-487.
- Lucan SC, Barg FK, Bazemore AW, Phillips RL Jr. Family medicine, the NIH, and the medical-research roadmap: perspectives from inside the NIH. Fam Med. 2009;41(3):188-196.
- Kuzel A, James P; Association of Departments of Family Medicine (ADFM). Research development stories from 7 departments of family medicine: 7 lessons for all departments. Ann Fam Med. 2011;9(4):373-374. https://doi.org/10.1370/afm.1281
- Family Medicine for America’s Health. Research Tactic Team. Family Medicine for America’s Health. https://fmahealth.org/research-tactic-team/. Accessed May 6, 2018.
- Bland CJ, Weber-Main AM, Lund SM, Finstad DA. The Research-Productive Department. Hoboken, NJ: John Wiley & Sons; 2005.
- Bland CJ, Center BA, Finstad DA, Risbey KR, Staples JG. A theoretical, practical, predictive model of faculty and department research productivity. Acad Med. 2005;80(3):225-237. https://doi.org/10.1097/00001888-200503000-00006
- National Research Council (US), Cooke NJ, Hilton ML, eds. Enhancing the Effectiveness of Team Science. Washington, DC: The National Academies Press; 2015.
- Wuchty S, Jones BF, Uzzi B. The increasing dominance of teams in production of knowledge. Science. 2007;316(5827):1036-1039. https://doi.org/10.1126/science.1136099
- Mitchell P, Wynia M, Golden R, et al. Core principles and values of effective team-based Health Care. Washington, DC: The National Academies Press; 2012. https://doi.org/10.31478/201210c
- Committee on Measuring the Impact of Interprofessional Education on Collaborative Practice and Patient Outcomes, Board on Global Health, Institute of Medicine. Measuring the Impact of Interprofessional Education on Collaborative Practice and Patient Outcomes. Washington, DC: National Academies Press; 2015. https://doi.org/10.17226/21726



There are no comments for this article.