Background and Objectives: Reproductive Health Education In Family Medicine(RHEDI) supports family medicine residency programs to establish a required rotation in sexual and reproductive health (SRH), including abortion. We evaluated long-term training effects by examining the practice patterns of family physicians 2 to 6 years after residency graduation, to determine whether and how the practices and abortion provision of those with enhanced SRH training differ from those who did not receive this training.
Methods: We invited 1,949 family physicians who completed residency training between 2010 and 2018 to complete an anonymous online survey about residency training and current provision of SRH services.
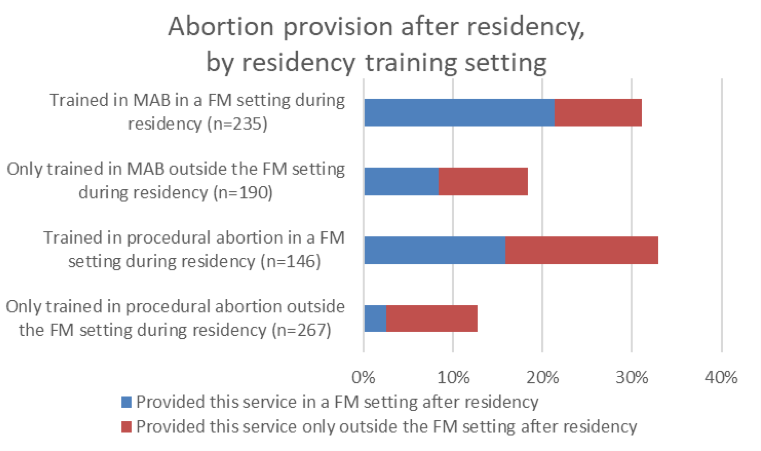
Results: We received 714 completed surveys, a 36.6% response rate. Of those who received routine abortion training during residency (n=445), 24% had provided abortion after graduation, significantly more than the 13% providing abortion who had not received routine training during residency, and much higher than the 3% provision rate found in a recent representative study. Abortion-trained respondents were also more likely than the comparison group to have provided other SRH care. For both medication and procedural abortion, respondents who trained in the family medicine setting were significantly more likely to have provided abortion after residency than those who trained only in dedicated abortion clinics (31% vs 18%, and 33% vs 13%, respectively).
Conclusions: Abortion training during family medicine residency is strongly linked to postresidency abortion provision, and is crucial in preparing family physicians to meet the full range of their patients’ reproductive health care needs.
Family physicians provide a range of sexual and reproductive health care (SRH), including contraception, diagnosis of pregnancy, prenatal care, and miscarriage management. Because of this, they are well-positioned to provide early abortion care to their patients in the primary care setting. Abortion provision in the context of primary care enhances continuity of care, and studies have found that it is acceptable to patients, with many stating they would prefer to seek abortion care with their primary care physicians rather than at a dedicated abortion clinic. 1-3 Abortion provision within the family medicine setting also has the potential to increase access for patients, because family physicians are well represented in rural areas and regions where other abortion-providing facilities are limited. 4, 5 In order to increase abortion provision within family medicine, some family medicine residency programs have integrated training in early abortion care into the residency curriculum.
Studies have found that the inclusion of abortion training in family medicine programs has a positive impact on residents’ knowledge, skills, and attitudes regarding abortion. 6-9 When residents were surveyed before and after routine abortion training, both interpersonal and technical skills related to abortion had improved, 7 as had related reproductive health skills in long-acting reversible contraception (LARC) insertion and miscarriage management. 8
There is less research, however, that examines the longer-term effects of routine integrated abortion training during residency on postresidency practice patterns. Two small studies both found that 27% of family medicine residents who had received comprehensive reproductive health training in residency had gone on to provide abortion, measured in one study at 5 years 10 and in the other between 1 and 6 years 11 after residency graduation. These findings are promising, compared in particular to the results of a large study of board-certified family physicians who graduated residency between 2013 and 2016, which found that only 3% of those respondents had provided abortion after residency. 12 A third study, focused on the US Northwest, compared abortion provision rates among graduates of residency programs with and without abortion training, but it found no difference in the rate of provision (6% and 7%, respectively). 13 Therefore, more research is needed to better understand the impact of including routine abortion training in family medicine residency programs.
Reproductive Health Education in Family Medicine (RHEDI), was founded in 2004 to advance abortion training within family medicine residency programs. To date, RHEDI has supported 36 residency programs in 17 states to enable them to establish and maintain a required rotation in SRH care, including abortion and contraception. This retrospective cohort study aims to assess RHEDI-trained physicians’ postresidency provision of SRH services, particularly abortion care. Our primary research question examines whether the provision patterns of family physicians with enhanced SRH training during residency (intervention group) differ from those of physicians from similar residency programs that did not include such training (comparison group). In addition, we aimed to learn more about the impact of training setting on subsequent abortion provision.
Study Design, Participants, and Instrument
For this study, we recruited two groups of currently practicing family physicians, all of whom graduated from family medicine residency programs between 2010 and 2018. Respondents in the intervention group graduated from residency programs receiving funding and technical assistance from RHEDI to include enhanced, integrated opt-out training in abortion and SRH care as part of standard residency training (“RHEDI programs”). To maximize similarities in institutional cultures and SRH training priorities, we drew the comparison group from residency programs that became RHEDI programs after the study participants completed residency. Physicians in the comparison group either received no training in abortion or found external elective abortion training opportunities during or after residency.
In order to assess graduates’ practice patterns, we sent a recuritment email to a national sample of 1,949 potential respondents (1,418 who graduated from RHEDI programs and 531 in the comparison group) that included the web-based survey link. The survey, which was pretested with a small group of RHEDI program alumni who completed residency prior to 2015, asked about training during residency, demographics, and current provision of SRH care services, including abortion, LARC, miscarriage management, and reproductive health counseling and referrals.
Recruitment
In addition to the initial survey invitation, reminder emails were sent at 2-week intervals. Recruitment and data collection took place in two waves: during the summer of 2017 for physicians who graduated residency from 2010 through 2014, and during the fall of 2020 for those who graduated residency from 2015 through 2018. Over the course of each of the 12-week recruitment periods, we also conducted supplemental recruitment via postal mail and text messages, when possible. All participants consented to the survey; the consent statement was included in the introduction to the survey and stated that consent was implied by its completion. Upon completing the survey, study participants received a gift card via email ($20 in 2017, and $40 in 2020, raised in an effort to increase the response rate) to compensate them for their time. The Montefiore Medical Center Institutional Review Board approved this study.
Analysis
We exported data from the secure Key Survey website into SPSS v27 software (STATA Corp, College Station, TX) for analysis. As the survey instrument and results were nearly identical across the two waves of data collection,* we combined the data sets to allow for a larger sample size and a more robust analysis. We first assessed differences between the RHEDI program physicians and the comparison group in demographics, abortion training, and abortion and SRH provision, and then aimed to identify factors that may correlate with current abortion provision. We used χ2 tests to examine differences in outcome variables between RHEDI program and comparison group physicians, and we used binary logistic regression for multivariate analysis. For the multivariate regression, we chose to include those variables in our model that previous research led us to hypothesize would have a relationship with abortion provision, and/or those associated with provision on a bivariate level. Statistical significance was set at 2-sided α=0.05.
Response Rates
The overall study response rate was 36.6%, with 714 total respondents. Twenty respondents were not eligible, as they had not provided clinical care in the United States in the past year or provided incomplete or contradictory information about their abortion training and provision. This left us with 694 eligible respondents: 508 who had trained at RHEDI programs and 186 who had not. Response rates did not differ significantly between the RHEDI-trained and comparison groups.
Demographics
The RHEDI-trained and comparison groups provided similar responses to demographic questions. Most respondents across both groups self-identified as cisgender women and practiced primarily in a family medicine setting, a category which includes federally qualified health centers, community health centers, and private practice (Table 1). The majority responded between 2 and 4 years after residency graduation, and over one-third were faculty at a residency program. While the largest proportion of respondents were based in the West, this location was significantly more common among the intervention group. However, this was not unexpected, as many family medicine programs with routine abortion training are located in the West and over half of physicians remain in the state where they completed residency,14 while the residency programs that the comparison group was drawn from are disproportionally based in the Midwest and South. In addition, the majority of the comparison group were recruited in the first wave of data collection due to logistical constraints.**
|
|
RHEDI Program Graduates, n=508 , % (n)
|
Comparison, n=186 ,
% (n)
|
Total,
N=694, % (n)
|
P Value
|
|
Data Collection Period
Wave 1, summer 2017
Wave 2, fall 2020
|
...
44.1 (224)
55.9 (284)
|
...
78.5 (146)
21.5 (40)
|
...
53.3 (370)
46.7 (324)
|
<.001
|
|
Gender
Cisgender male
Cisgender female
Transgender and nonbinary
|
...
26.2 (133)
72.6 (369)
1.2 (6)
|
...
28 (52)
71.5 (133)
.5 (1)
|
...
26.7 (185)
72.3 (502)
1 (7)
|
.689
|
|
Current Region of Practice (n=686) a
Northeast
Midwest
South
West
|
(n=500)
21.8 (109)
9.2 (46)
9 (45)
60 (300)
|
...
18.3 (34)
18.3 (34)
19.4 (36)
44.1 (82)
|
...
20.8 (143)
11.7 (80)
11.8 (81)
55.7 (382)
|
<.001
|
|
Years Between Survey and Residency Graduation
2 to 4 years
5 to 7 years
|
...
61.6 (313)
38.4 (195)
|
...
45.7 (85)
54.3 (101)
|
...
57.3 (398)
42.7 (296)
|
<.001
|
|
Location of Primary Practice Setting
Urban
Suburban
Rural
|
...
49.4 (251)
35.8 (182)
14.8 (75)
|
...
43.5 (81)
32.8 (61)
23.7 (44)
|
...
47.8 (332)
35 (243)
17.1 (119)
|
.022
|
|
Faculty at a Residency Program
|
39.6 (201)
|
34.9 (65)
|
38.3 (266)
|
.267
|
|
Primary Practice Setting
Family medicine clinic (not FQHC)
Community health center (eg, FQHC)
Private practice
Inpatient hospital care
Dedicated abortion clinic
All other
|
...
40.4 (205)
33.1 (168)
6.7 (34)
4.7 (24)
1.2 (6) 14 (71)
|
...
46.2 (86)
23.7 (44)
9.7 (18)
5.4 (10)
15.1 (28)
|
...
41.9 (291)
30.5 (212)
7.5 (52)
4.9 (34) .
9 (6)
14.3 (99)
|
.104
|
|
Secondary Practice Setting
No secondary practice setting
Family medicine clinic (not FQHC)
Community Health Center (eg, FQHC)
Private practice
Inpatient hospital care
Dedicated abortion clinic
All other
|
...
62.4 (317)
3.1 (16)
4.3 (22)
.4 (2)
17.9 (91)
5.9 (30)
5.9 (30)
|
...
60.8 (113)
.5 (1)
4.3 (8)
1.1 (2)
25.3 (47)
1.6 (3)
6.5 (12)
|
...
62 (430)
2.4 (17)
4.3 (30)
.6 (4)
19.9 (138)
4.8 (33)
6.1 (42)
|
.03
|
|
Was a Member of Medical Students for Choice in Medical School
|
22 (112)
|
20.4 (38)
|
21.6 (150)
|
.647
|
|
Definitely Intended to Provide Abortion at Medical School Graduation
|
20.5 (104)
|
11.3 (21)
|
18.0 (125)
|
.005
|
Abortion and Other Sexual and Reproductive Health Training and
Post
residency
Provision
We began by comparing differences in abortion training patterns during residency between the two groups. RHEDI-trained respondents were significantly more likely than the comparison group to have received training in all types of abortion; the most dramatic differences were seen with manual vacuum aspiration (MVA), where they were more than four times more likely to have been trained (79% vs 17%; Table 2).
|
Service Training or Provision
|
RHEDI Program Graduates , n=508,
% (n)
|
Comparison, n=186 ,
% (n)
|
Total, N=694 ,
% (n)
|
P Value (χ 2 )
|
|
Reproductive Health Training During Residency a
|
|
Medication abortion (MAB)
|
83.8 (425)
|
29.2 (54)
|
69.2 (479)
|
<.001
|
|
Manual vacuum aspiration (MVA)
|
78.9 (400)
|
17.3 (32)
|
62.4 (432)
|
<.001
|
|
Electric vacuum aspiration (EVA)
|
65.4 (329)
|
16.8 (31)
|
52.3 (360)
|
<.001
|
|
Reproductive Health Provision After Residency
|
|
Any abortion
|
23.6 (120)
|
12.9 (24)
|
20.7 (144)
|
.002
|
|
Medication abortion
|
22.6 (115)
|
12.9 (24)
|
20 (139)
|
.005
|
|
Procedural abortion
|
16.1 (82)
|
7 (13)
|
13.7 (95)
|
.002
|
|
Medical management of miscarriage
|
40.7 (207)
|
35.5 (66)
|
39.3 (273)
|
.209
|
|
Aspiration management of miscarriage
|
21.5 (109)
|
14 (26)
|
19.5 (135)
|
.027
|
|
Abortion methods options counselingb
|
79.3 (403)
|
69.4 (129)
|
76.7 (532)
|
.006
|
|
Abortion referral
|
81.3 (413)
|
75.3 (140)
|
79.7 (553)
|
.08
|
These differences were borne out in an examination of abortion provision after residency graduation. Here, there were significant differences between the two groups in all categories, with the RHEDI-trained physicians more likely than their peers to have provided any medication abortion (MAB), any procedural abortion, and any abortion after residency. This was also true for any abortion provision in the past year, where 16% of RHEDI program graduates had provided in the past year, as compared to 6.5% of those in the comparison group (P<.001; data not shown).
We also examined the reproductive health practice patterns of the two groups. There were significant differences between the groups in aspiration for miscarriage and abortion methods options counseling (Table 2), with RHEDI program graduates significantly more likely to have provided both services after residency.
In bivariate analysis, we examined the associations between various demographic factors and abortion provision after residency (Table 3). As discussed above, having trained at a RHEDI program during residency was strongly associated with abortion provision after residency. Significant associations were also found between abortion provision and gender, with cisgender women and trans/gender nonconforming people much more likely to provide abortion than cisgender men. Urban respondents, as well as those who were faculty at residency programs, were far more likely to provide abortion after residency. Finally, membership in Medical Students for Choice (MSFC) and recalled intention to provide abortion at medical school graduation were also significantly associated with abortion provision after residency. It is worth noting, however, that routine training can also engage residents without preexisting interest in abortion; 27% of the abortion-providing graduates from RHEDI programs reported that they did not certainly intend to provide abortion at medical school graduation (data not shown).
|
|
Percent of Each Subgroup That Provided Abortions After Residency, (n/N)
|
P Value
|
|
RHEDI Training
RHEDI program graduates
Comparison group
|
...
23.6 (120/508)
12.9 (24/186)
|
.002
|
|
Data Collection Period
Wave 1, summer 2017
Wave 2, fall 2020
|
...
18.1 (67/370)
23.8 (77/324)
|
.067
|
|
Gender
Cisgender men
Cisgender women
Transgender and nonbinary respondents
|
...
13.5 (25/185)
23.1 (116/502)
42.9 (3/7)
|
.008
|
|
Region of Practice a
Northeast
Midwest
South
West
|
...
16.8 (24/143)
17.5 (14/80)
24.7 (20/81)
21.5 (82/382)
|
.432
|
|
Years Between Survey and Residency Graduation
2 to 4 years
5 to 7 years
|
...
18.8 (75/398)
23.3 (69/296)
|
.151
|
|
Location of Primary Practice Setting
Urban
Suburban
Rural
|
...
28.6 (95/332)
13.6 (33/243)
13.4 (16/119)
|
<.001
|
|
Faculty Status
Faculty at a residency program
Not faculty at a residency program
|
...
34.6 (92/266)
12.1 (52/428)
|
<.001
|
|
Primary Practice Setting b (n=688)
Family medicine/primary care, not FQHC
Family medicine/community health center, eg, FQHC
Private practice
Inpatient hospital
Other
|
...
19.2 (56/291)
22.6 (48/212)
11.5 (6/52)
23.5 (8/34)
20.2 (20/99)
|
<.480
|
|
Medical Students for Choice Member in Medical School
Yes
No
|
...
42.0 (63/150)
14.9 (81/544)
|
<.001
|
|
Recalled Intention at Medical School Graduation
Certainly intended to provide abortion at MS graduation
Did not certainly intend to provide abortion at MS graduation
|
...
37.6 (47/125)
17 (97/569)
|
<.001
|
Multivariate Analysis
In adjusted analysis, RHEDI-trained respondents were twice as likely as their non-RHEDI trained peers to provide abortion after residency (P=.009, Table 4). In this model, respondents practicing in urban settings, those who were residency faculty, those who were members of MSFC, and those who certainly intended to provide at medical school graduation were also significantly more likely to have provided abortion after residency graduation.
|
Characteristic
|
Reference Category
|
OR
|
Confidence Interval (.95)
|
P Value
|
|
RHEDI-trained
|
Comparison group
|
1.99
|
1.19–3.34
|
.009
|
|
Cisgender women and trans/GNC
|
Cisgender men
|
1.37
|
.82–2.30
|
.224
|
|
Urban
|
Suburban or rurala
|
2.07
|
1.36–3.15
|
<.001
|
|
Faculty at a residency program
|
Was not residency faculty
|
3.33
|
2.19–4.99
|
<.001
|
|
Medical Students for Choice member in medical school
|
Was not a member of MSFC in medical school
|
3.08
|
1.91–4.93
|
<.001
|
|
Certainly intended to provide abortion at medical school graduation
|
Did not certainly intend to provide abortion at medical school graduation
|
1.75
|
1.06–2.91
|
.029
|
This model was robust when testing alternate and additional variables of interest, such as region and years since residency graduation, but these variables did not ultimately contribute to the overall strength of the model. Since practice setting ceased to be significantly associated with abortion provision on a bivariate level once we excluded respondents whose primary practice settings were abortion clinics in a stratified analysis, practice setting was not included in the multivariate model.
Setting of Abortion Training and Subsequent Provision of Abortion Care Among RHEDI Graduates
Setting of postresidency provision varied by abortion type. Of RHEDI-trained respondents who provided medication abortion, 61% had done so in the family medicine setting. In contrast, only 37% of those who provided procedural abortion had done so in the family medicine setting.
We also examined the effect of abortion training setting among RHEDI graduates trained in abortion. For some respondents, either medication or procedural abortion training or both took place in the family medicine setting, while for other respondents, training took place only in a high-volume abortion clinic setting.
As Figure 1 demonstrates, those respondents who trained in a given abortion method in the family medicine setting were significantly more likely to provide abortions of that type after residency. Of the residents who trained in MAB in the family medicine setting, 31% provided this service after residency, compared to 18% of those who trained in MAB in a non-family medicine setting (P=.001). Similarly, of the residents who trained in procedural abortion in the family medicine setting, 33% went on to provide it after residency, compared to 13% of those who trained in procedural abortion only in a non-family medicine setting (P<.001.)
In addition, those who trained in the family medicine setting were significantly more likely to go on to provide that type of abortion in the family medicine setting, rather than in other practice settings. Of those residents who trained in MAB within a FM setting and went on to provide this service after residency, 68% provided MAB within the FM setting, as compared to 45% of those who did their MAB training only outside of the FM setting (P=.004). Of the residents who trained in procedural abortion within an FM setting and went on to provide this service after residency, 48% did so within the FM setting, as compared to 20% of their peers who had procedural abortion training only outside of family medicine (P<.001).
In this study, we examined the SRH practice patterns of two groups of family physicians. The first group had received routine opt-out abortion training during residency at RHEDI-supported residency programs, while the second group had not trained in abortion unless they sought out elective training. Our results show that the physicians who graduated from the RHEDI programs had significantly higher rates of abortion provision after graduation. This was particularly true for procedural abortion and abortion provision in the past year. We also found higher rates of aspiration for miscarriage and abortion methods options counseling among those physicians who had received routine abortion training. In adjusted analysis, RHEDI training held up as a strong predictor of postresidency abortion provision, with RHEDI graduates twice as likely to provide abortion as the comparison group. In addition, working as faculty at a residency program, living in an urban area, previous membership in Medical Students for Choice, and intention to provide at medical school graduation were also strong predictors of provision.
More physicians in our sample provided medication abortion than procedural abortion. In addition, respondents were more likely to offer medication abortion than procedural abortion within the family medicine setting. This finding confirms other recent research, which found that family physicians felt medication abortion was much easier to integrate into primary care than procedural abortion, 15 and that physicians who had hands-on medication abortion training were twice as likely as their peers to go on to provide any abortions after graduation. 16 This argues for emphasizing medication abortion training for family medicine residents as a strategy to more efficiently expand abortion access within primary care.
Interestingly, we did not find a significant correlation between region of practice and abortion provision, despite abortion provision (both generally and within family medicine) being far more restricted in the South and Midwest. 17 We theorize that the expected regional differences in provision may have been muted due to both a saturation of abortion providers in the Northeast and West, as well as by motivated RHEDI graduates responding to the need for abortion services in the South and Midwest. However, particularly with the additional restrictions on abortion services and training taking effect after the 2022 Dobbs v Jackson Womens Health Organization Supreme Court decision, we expect regional differences to become more stark moving forward.
Our data also show that training within a family medicine setting is correlated with both abortion provision after residency graduation, and provision within a family medicine setting. Ensuring that abortion training includes provision in a family medicine setting, precepted by family physicians, could help increase the likelihood of subsequent provision, as graduates would be able to draw on experiences with abortion provision integrated into a continuity practice. This parallels findings from research on pregnancy care in family medicine training, where increased integration of continuity prenatal patients into a routine resident panel, precepting of delivery care by family medicine faculty, and mentorship by family physicians providing pregnancy care, were found to be predictive of graduates providing this care in their posttraining careers. 18-20
One limitation to our study is response bias. While our 36.6% response rate is in the typical range for online surveys of physicians, it is possible that those respondents with stronger opinions on abortion, whether positive or negative, were more likely to respond, and that abortion providers are overrepresented or underrepresented in our sample. However, our findings are similar to those of two other studies on abortion training and postresidency provision. 10, 11 Also, as we did not ask participants about their race and ethnicity until the 2020 wave of data collection, we were unable to include these factors in this analysis, although examinations of the 2020 data show lower rates of abortion provision among physicians underrepresented in medicine. 21
Another limitation is that medical students with pre-existing interest in abortion care may well have self-selected into RHEDI programs for residency, thus making the comparison group an imperfect one for those at RHEDI programs and potentially overstating the effects of training at a RHEDI program. However, as we drew comparison group respondents from programs that initiated additional SRH and/or abortion training soon after these participants graduated residency, their programs also likely emphasized reproductive health and may have drawn a group that was also disproportionally interested in SRH. The fact that equivalent proportions of the two groups were members of Medical Students for Choice supports this hypothesis. This may be why postresidency abortion provision in the comparison group, at 13%, was also well above the 3% rate of abortion provision found in a large study of family physicians, 12 which may be more typical of family physicians overall. In addition to seeking a comparison group that was more interested in SRH than the general family physician pool, we also took a conservative approach to the analysis by not excluding the 63 respondents who trained at RHEDI programs but opted out of abortion training within the RHEDI program group.
Routine abortion training in family medicine residency programs is associated with more abortion provision after residency. Furthermore, routine exposure to abortion care appears to build providers’ related reproductive health skills, shifts attitudes, and prepares them to better counsel and refer patients seeking abortion if they are unable or unwilling to provide abortion care themselves. 8, 22 Since many family physicians provide care in areas without access to high-volume abortion clinics, 4, 5 integrating routine abortion training into residency in those states that allow abortion care and training is a crucial component in preserving patients’ access to this essential service.
Footnotes
.....*While some survey items in the 2017 survey instrument were modified or omitted in the 2020 instrument, and a few new questions were added, all of the survey items analyzed in this study remained the same between the two surveys, with no differences in the phrasing of these questions.
.....**This was due to the fact that more residency programs initiated RHEDI training in the period around 2014, creating a larger pool of eligible graduates for the comparison group, then did so in the period around 2018.
References
-
Wu JP, Godfrey EM, Prine L, Andersen KL, MacNaughton H, Gold M. Women’s satisfaction with abortion care in academic family medicine centers. Fam Med. 2015;47(2):98-106.
-
Summit AK, Casey LM, Bennett AH, Karasz A, Gold M. “I Don’t Want to Go Anywhere Else”: Patient Experiences of Abortion in Family Medicine. Fam Med. 2016;48(1):30-34.
-
Godfrey EM, Rubin SE, Smith EJ, Khare MM, Gold M. Women’s preference for receiving abortion in primary care settings.
J Womens Health (Larchmt). 2010;19(3):547-553.
doi:10.1089/jwh.2009.1454
-
Petterson S MR, Klink K, Meyers D, Bazemore A. The State of Primary Care in the United States: A Chartbook of Facts and Statistics. 2018.
-
Cartwright AF, Karunaratne M, Barr-Walker J, Johns NE, Upadhyay UD. Identifying National Availability of Abortion Care and Distance From Major US Cities: Systematic Online Search.
J Med Internet Res. 2018;20(5):e186.
doi:10.2196/jmir.9717
-
Bennett I, Johnson M, Wu JP, et al. A family medicine training collaborative in early abortion. Fam Med. 2007;39(3):164-166.
-
Nothnagle M. Benefits of a learner-centred abortion curriculum for family medicine residents.
J Fam Plann Reprod Health Care. 2008;34(2):107-110.
doi:10.1783/jfp.34.2.107
-
Summit AK, Gold M. The Effects of Abortion Training on Family Medicine Residents’ Clinical Experience. Fam Med. 2017;49(1):22-27.
-
Steinauer JE, Turk JK, Pomerantz T, Simonson K, Learman LA, Landy U. Abortion training in US obstetrics and gynecology residency programs. Am J Obstet Gynecol. Jul 2018;219(1):86 e1-86 e6. doi:10.1016/j.ajog.2018.04.011
-
Srinivasulu S, Maldonado L, Prine L, Rubin SE. Intention to provide abortion upon completing family medicine residency and subsequent abortion provision: a 5-year follow-up survey. Contraception. 2019;100(3):188-192. doi:10.1016/j.contraception.2019.05.011
-
Goodman S, Shih G, Hawkins M, et al. A long-term evaluation of a required reproductive health training rotation with opt-out provisions for family medicine residents. Fam Med. 2013;45(3):180-186.
-
Patel P, Narayana S, Summit A, et al. Abortion Provision Among Recently Graduated Family Physicians.
Fam Med. 2020;52(10):724-729.
doi:10.22454/FamMed.2020.300682
-
Weidner A, Stevens N, Shih G. Associations Between Program-Level Abortion Training and Graduate Preparation for and Provision of Reproductive Care.
Fam Med. 2019;51(9):750-755.
doi:10.22454/FamMed.2019.219951
-
-
Greenberg S, Nothnagle M. An “Invaluable Skill”: Reflections on Abortion Training and Postresidency Practice.
Fam Med. 2018;50(9):691-693.
doi:10.22454/FamMed.2018.529396
-
Stulberg DB, Monast K, Dahlquist IH, Palmer K. Provision of abortion and other reproductive health services among former Midwest Access Project trainees.
Contraception. 2018;97(4):341-345.
doi:10.1016/j.contraception.2018.01.002
-
-
Sutter MB, Prasad R, Roberts MB, Magee SR. Teaching maternity care in family medicine residencies: what factors predict graduate continuation of obstetrics? A 2013 CERA program directors study. Fam Med. 2015;47(6):459-465.
-
Coonrod RA, Kelly BF, Ellert W, Loeliger SF, Rodney WM, Deutchman M. Tiered maternity care training in family medicine. Fam Med. 2011;43(9):631-637.
-
Hansen ER, Eden AR, Peterson LE. A qualitative study of trainee experiences in Family Medicine-Obstetrics fellowships. Birth. 2019;46(1):90-96. doi:10.1111/birt.12388
-
Summit AK, Carvajal DN. Abortion training and provision among family physicians underrepresented in medicine. Presented at: Society for the Teachers of Family Medicine; 2022; Indianapolis, IN.
-
Kumar V, Herbitter C, Karasz A, Gold M. Being in the room: reflections on pregnancy options counseling during abortion training. Fam Med. 2010;42(1):41-46..



There are no comments for this article.