Background and Objectives: The United States has seen an evolving perspective on the medical use of cannabis in recent years. Although a majority of states have enacted medical cannabis programs, physicians practicing in these states report a lack of knowledge, lingering concerns, and a need for more training regarding medical cannabis. This study provides a current snapshot of medical cannabis education in an academic family medicine department in a state with a medical cannabis program.
Methods: An electronic survey was sent to all 134 faculty physicians and residents within a family medicine department to assess current knowledge and attitudes regarding medical cannabis. Study authors performed descriptive statistical analysis of the survey data.
Results: Of the 61 individuals to complete the survey, 34 were residents and 27 were faculty. Overall, respondents displayed poor understanding of the state’s medical cannabis program as well as cannabis regulations. A majority of both faculty and residents reported low self-rated competency levels for medical cannabis efficacy, adverse effects, and safety using Likert scales (1 to 5; 1=low competency, 5=high competency). A majority of faculty (56%) expressed that they did not intend to certify patients for medical cannabis compared to only 33% of residents. Residents were statistically more likely to think of a patient who might benefit from medical cannabis compared to faculty (39% vs 11%, P=.004, chi-square).
Conclusions: Increasingly, family physicians will be called on to provide informed patient counseling regarding medical cannabis. These results highlight a knowledge gap for family medicine learners in a changing practice landscape.
Over the past 20 years, the United States has seen an evolving perspective on the medical use of cannabis. Although classified as a Schedule I substance under the federal Controlled Substance Act, 28 states and the District of Columbia have enacted laws allowing medical cannabis use for specific medical conditions as of 2017.1,2 Many of these state programs require physician involvement in the documentation of eligible conditions or in counseling patients regarding medical cannabis use.
While federal regulations have limited large-scale research on medical cannabis, a growing body of evidence has suggested some effectiveness for specific medical conditions.2-7 However, physicians practicing in states with medical cannabis programs acknowledge a lack of comfort with medical cannabis. Surveys of physicians in Colorado and Washington state revealed that a majority had lingering concerns about the medical benefits and potential risks of cannabis use. Nearly all survey respondents stressed the need for medical education and formal training in medical cannabis.8,9
Given this perspective, we chose to assess attitudes and knowledge regarding medical cannabis in an academic family medicine department in a state with a new medical cannabis program. This study provides a snapshot of current medical cannabis education among future family physicians likely to practice in a state with legalized medical cannabis. This is the first known study assessing attitudes and knowledge of medical cannabis in academic family medicine.
The Minnesota Medical Cannabis Program (MMCP) began services on July 1, 2015 for nine medical conditions for which there is at least limited evidence for efficacy. In order to identify pertinent clinical and educational issues related to the MMCP, the University of Minnesota Department of Family Medicine and Community Health convened a multidisciplinary work group to conduct an assessment of existing knowledge and perceptions related to medical cannabis and the new state program. To this end, a 15-question electronic survey was developed using REDCap.10 An email link to the anonymous survey was distributed to all faculty physicians and residents within the department on July 30, 2015. A reminder email to complete the survey was sent 2 weeks after the initial invitation.
Members of the work group performed descriptive statistical analysis of the survey data using SAS software version 9.4 (SAS Institute Inc., Cary, NC). The University of Minnesota Institutional Review Board approved all study activities.
Of the 134 participants invited to participate in the survey, 61 individuals (46%) completed it. Of the respondents, 34 (56%) were residents and 27 (44%) were faculty. Overall, survey respondents demonstrated poor understanding of logistical details of the MMCP. Respondents also demonstrated a lack of knowledge surrounding federal classification of cannabis, with only 52% correctly identifying cannabis as a Schedule I controlled substance. Additionally, 95% of the residents and faculty reported no prior continuing medical education activities on medical cannabis.
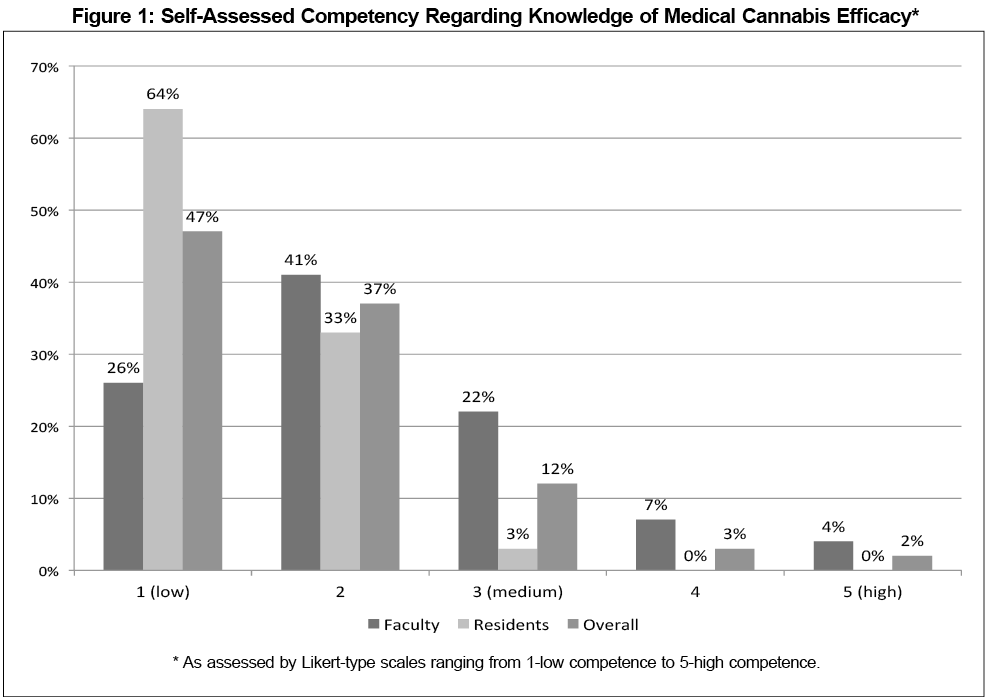
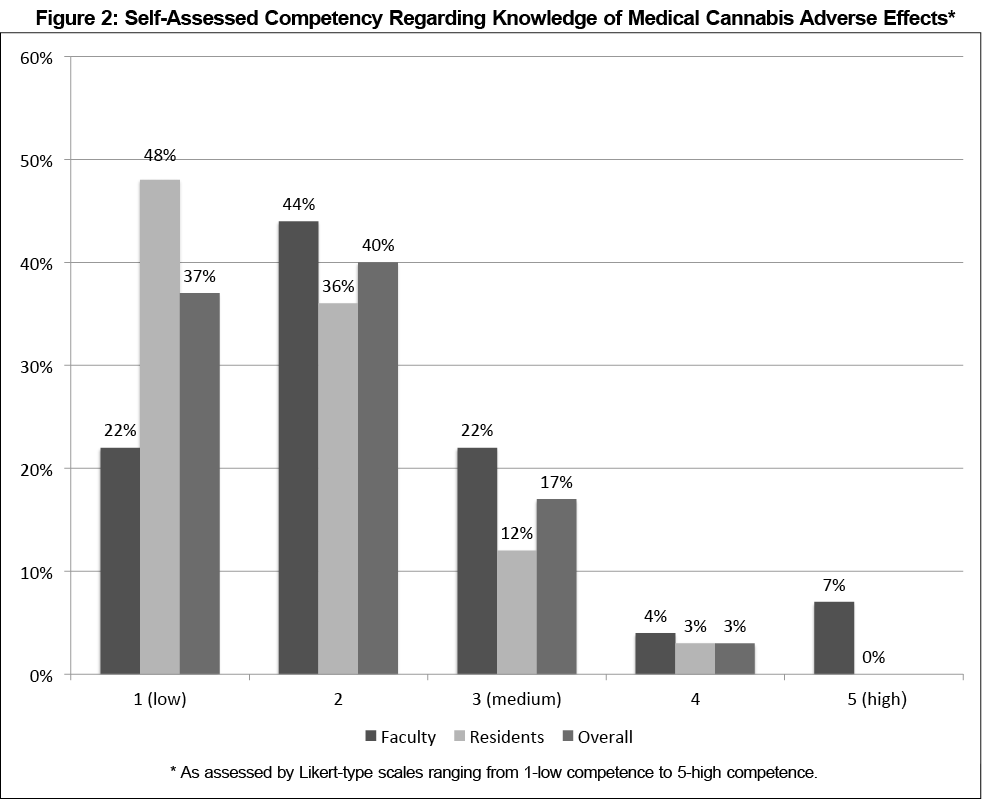
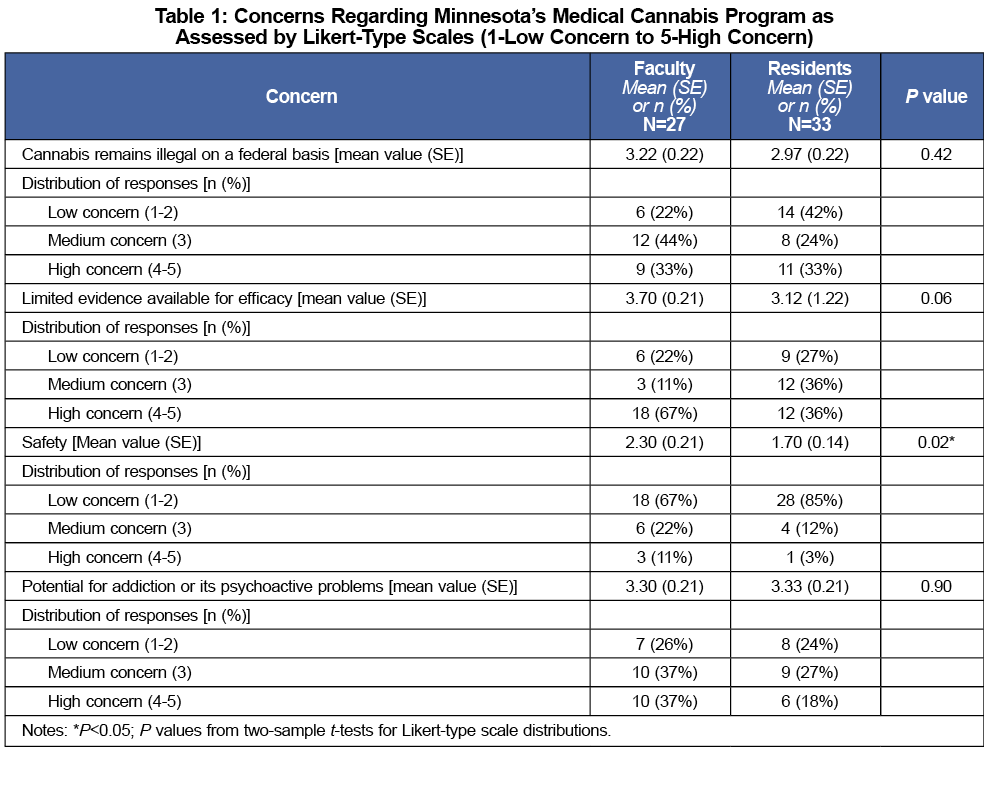
Survey participants rated their competency levels using a Likert scale (1 to 5; 1=low competency, 5=high competency) for knowledge regarding medical cannabis efficacy and adverse effects. Overall, respondents had low self-rated competency for both topics, although faculty rated themselves higher in comparison to residents (Figures 1 and 2). Respondents also rated their concerns regarding various aspects of medical cannabis (Table 1). A majority of faculty and residents had moderate concern regarding federal regulations. Fewer respondents were as concerned about safety, with residents statistically less so than faculty (P=0.02). Most faculty were very concerned about the limited evidence for medical cannabis. With regard to the potential for addiction and psychoactive effects, respondents were overall moderately concerned.
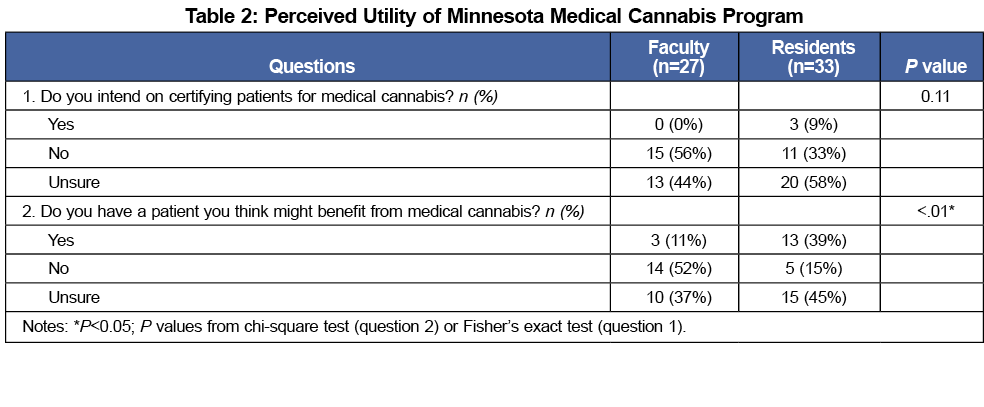
A majority of participants were hesitant to participate in the state program, with faculty seemingly more hesitant. Fifty six percent of faculty did not intend to certify patients for medical cannabis, whereas only 33% of residents made the same distinction. Only three participants, all residents, stated they intended to certify patients for medical cannabis (Table 2). When asked if they could think of one patient who might benefit from medical cannabis, a majority of faculty (52%) responded “no”, while only 11% said “yes.” By contrast, 39% of residents answered “yes” to this question, while only 15% said “no”, representing a statistically significant difference from faculty (P=.004, Table 2).
Similar to previously published findings among practicing physicians in states with legalized medical cannabis, the survey respondents in this study acknowledged a lack of knowledge surrounding the evidence for medical cannabis. 8,9,11 Also, consistent with previous research, a majority of respondents reported being moderately to very concerned about aspects of medical cannabis including efficacy, safety, legal issues, and the potential for addiction.8,9,11
Within the context of a lack of knowledge and lingering concerns surrounding medical cannabis, a majority of faculty stated that they would not participate in the state program. By contrast, residents seemed more open to this idea. Similarly, residents were significantly more likely than faculty to have a patient in mind that might benefit from medical cannabis. This distinction by role potentially represents a generational shift in openness to considering medical cannabis as a legitimate treatment for some patients, despite similar levels of knowledge deficits and concerns about cannabis effects. This study has several limitations. The sample was limited to a single academic family medicine department, and the survey response rate was suboptimal. Given the primary objective of a departmental needs assessment, power calculations were not done to determine sample size.
Given that over half of the states in the United States now have medical cannabis programs, an increasing number of family physicians will care for patients who might have questions about medical cannabis as a possible treatment option. Currently, the workforce is unprepared to engage patients effectively in informed, shared decision-making regarding medical cannabis.8,9 This survey illustrates a knowledge deficit among the next generation of family physicians. More importantly, these results suggest that the faculty responsible for training family medicine learners are currently not equipped with the necessary knowledge and skills to discuss the nuanced issues surrounding the risks and benefits of medical cannabis. These results highlight a curricular gap for family medicine learners in a changing practice landscape. While stigma, safety, and legal questions are potential obstacles to discussing medical cannabis, our patients as well as the next generation of family medicine physicians will be best served when educators begin to critically appraise and present the available evidence for and against the medical use of cannabis.
Acknowledgments
Presented at the STFM Annual Spring Conference, Minneapolis, MN; May 1, 2016.
References
- Office of National Drug Control Policy. Marijuana Resource Center: State Laws Related to Marijuana. https://www.whitehouse.gov/ondcp/state-laws-related-to-marijuana. Accessed March 8, 2016.
- Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: A systematic review and meta-analysis. JAMA. 2015;313(24):2456-2473.
https://doi.org/10.1001/jama.2015.6358.
- Aggarwal SK. Cannabinergic pain medicine: a concise clinical primer and survey of randomized-controlled trial results. Clin J Pain. 2013;29(2):162-171.
https://doi.org/10.1097/AJP.0b013e31824c5e4c.
- National Academies of Sciences, Engineering, and Medicine. 2017. The health effects of cannabis and cannabinoids: The current state of evidence and recommendations for research. Washington, DC: The National Academies Press.
- Boychuk DG, Goddard G, Mauro G, Orellana MF. The effectiveness of cannabinoids in the management of chronic nonmalignant neuropathic pain: a systematic review. J Oral Facial Pain Headache. 2015;29(1):7-14.
https://doi.org/10.11607/ofph.1274.
- Carter GT, Javaher SP, Nguyen MH, Garret S, Carlini BH. Re-branding cannabis: the next generation of chronic pain medicine? Pain Manag. 2015;5(1):13-21.
https://doi.org/10.2217/pmt.14.49.
- Hill KP. Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: A clinical review. JAMA. 2015;313(24):2474-2483.
https://doi.org/10.1001/jama.2015.6199.
- Kondrad E, Reid A. Colorado family physicians’ attitudes toward medical marijuana. J Am Board Fam Med. 2013;26(1):52-60.
https://doi.org/10.3122/jabfm.2013.01.120089.
- Carlini BH, Garrett SB, Carter GT. Medicinal cannabis: A survey among health care providers in Washington state. Am J Hosp Palliat Care. 2015.
https://doi.org/10.1177/1049909115604669.
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381.
https://doi.org/10.1016/j.jbi.2008.08.010.
- Moeller KE, Woods B. Pharmacy students’ knowledge and attitudes regarding medical marijuana. Am J Pharm Educ. 2015;79(6):85.
https://doi.org/10.5688/ajpe79685.



There are no comments for this article.