Introduction: Lack of health equity ultimately leads to unequal treatment of diverse patients and contributes to the growing disparities seen in national health. Academic medical centers should consider providing health care providers and biomedical researchers training on how to identify and address health disparities.
Methods: The authors led an introductory health disparities course for graduate students and research and clinical fellows at an academic medical center in the Midwest. We compared pre/postcourse assessments to determine changes in learners’ perceptions and knowledge of health disparities using an unpaired analysis to permit inclusion of responses provided only at baseline.
Results: Sixty-two learners completed preassessment, with 56 completing the postassessment (90%). In the postcourse assessment, learners reported an increase in knowledge of disparities and had changes in their perceptions of health disparities linked to treatment of different patient groups based on demographic characteristics. There was a statistically significant difference in learners’ perceptions of how patients are treated based on gender identity (P=0.02) and sexual orientation (P=0.04).
Conclusions: The results detail how an academic medical center can provide training on health disparities for diverse learners. This study underscores the influence of health disparities from the perspective of learners who conduct biomedical research and patient care. This course serves a model for introductory-level health disparities courses.
Race, ethnicity, age, gender, sexual orientation, geographic location, and socioeconomic status are used to identify health disparities globally. The National Academy of Medicine, National Commission for Health Education Credentialing, Center for Disease Control and Prevention, Academy Health, Association of American Medical Colleges, and Accreditation Council for Graduate Medical Education are committed to reducing health disparities in their workforce, recommending academic medical centers and other institutions provide didactic training to their learners.
The importance of creating the best curricula to produce the best outcomes is pivotal to development of health disparities curriculum for diverse learners at academic medical centers. Traditionally, curricula in academic medical centers focused on health professions; there is not a unified model for curriculum delivery to health professionals.1 To address this gap, we created a standardized curriculum that considers health disparities routinely seen by health providers who are committed to eliminating heath inequalities.2,3 The purpose of this paper is to provide context around teaching a one-credit health disparities course to diverse graduate learners at an academic medical center and evaluate the self-reported impact of the course on learners’ understanding of disparities in the health care setting.
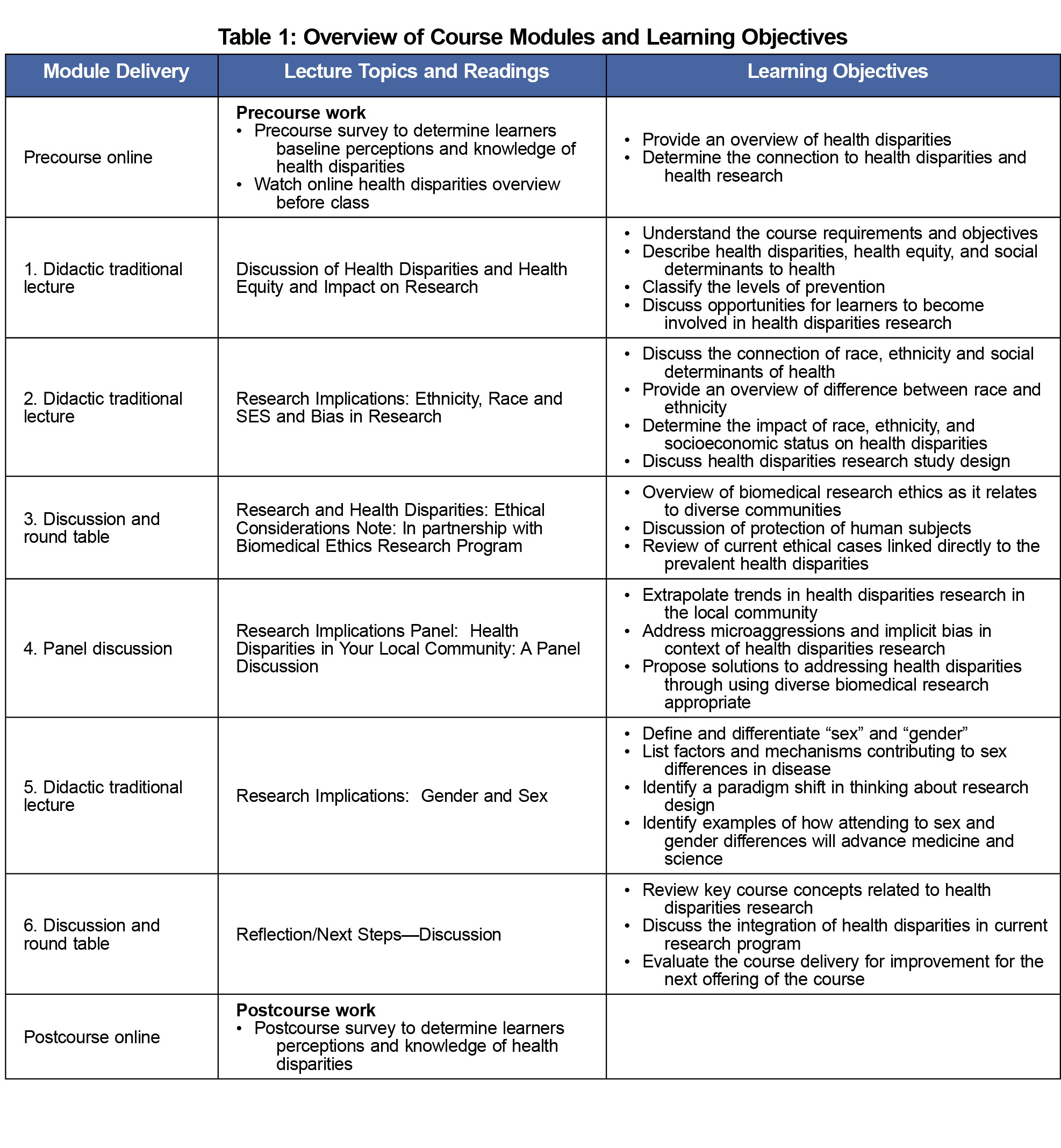
The Mayo Clinic Graduate School of Biomedical Sciences created a 6-week graduate course titled “Introduction to Health Disparities.” Table 1 is an overview of the modules’ content. The blended learning course used an online learning management system for lecture materials and communication with learners. Each class period lasted 90 minutes. The course learning objectives were: (1) define and identify health disparities and health equity commonly experienced in diverse communities; (2) identify and discuss how demographic characteristics influence study design, implementation, and dissemination; and (3) critique health disparities literature by responding with a letter to the editor and leading a class discussion of the selected course material.
A combination of didactic lectures with guest speakers provided the foundation for presenting content with a round table used to spark dialogue with the learners. A variety of andragogical teaching techniques like think-pair-share and carousel activities provoked discussion among learners, the course directors, and guest speakers about complex topics like discrimination, racism, and genderism as they relate to patient care and research. Learners consisted of students enrolled in a doctoral, master’s, or certificate program in biomedical science.
Survey Design
Learners completed a pre/postcourse assessment on their knowledge and perceptions of health disparities. The assessment contained items from the National Physician Survey (NPS) that determined physicians’ perceptions of disparities in the community.4 The NPS survey had face validity with few details provided on the reliability and validity of the survey. For this study, we analyzed eight items that evaluated perceptions of how the health care system treats patients based on their individual demographics. Learners used a 4-point Likert scale (0=never to 4=very often) to rate items. One-tenth of the course grade was earned by completing the pre/postcourse survey. The Mayo Clinic Institutional Review Board determined the study was exempt.
The course content covered the definition of health disparities and their impact on the local community. Learners examined the literature and discussed the ramifications of patient demographics linked directly to discrimination, health care reform, and access to care. Additionally, learners categorized health disparities in their research areas and medical specialties.
We compared pre/postcourse assessments to determine changes in learners’ perceptions and knowledge of health disparities, using an unpaired analysis to permit inclusion of responses provided only at baseline. Because of the ordinal nature of the items, a test for trend was used for each item in a separate logistic regression model. Analyses were performed in Stata statistical software version 11 (College Station, TX) with two-sided 5% type I error used to determine statistical significance.
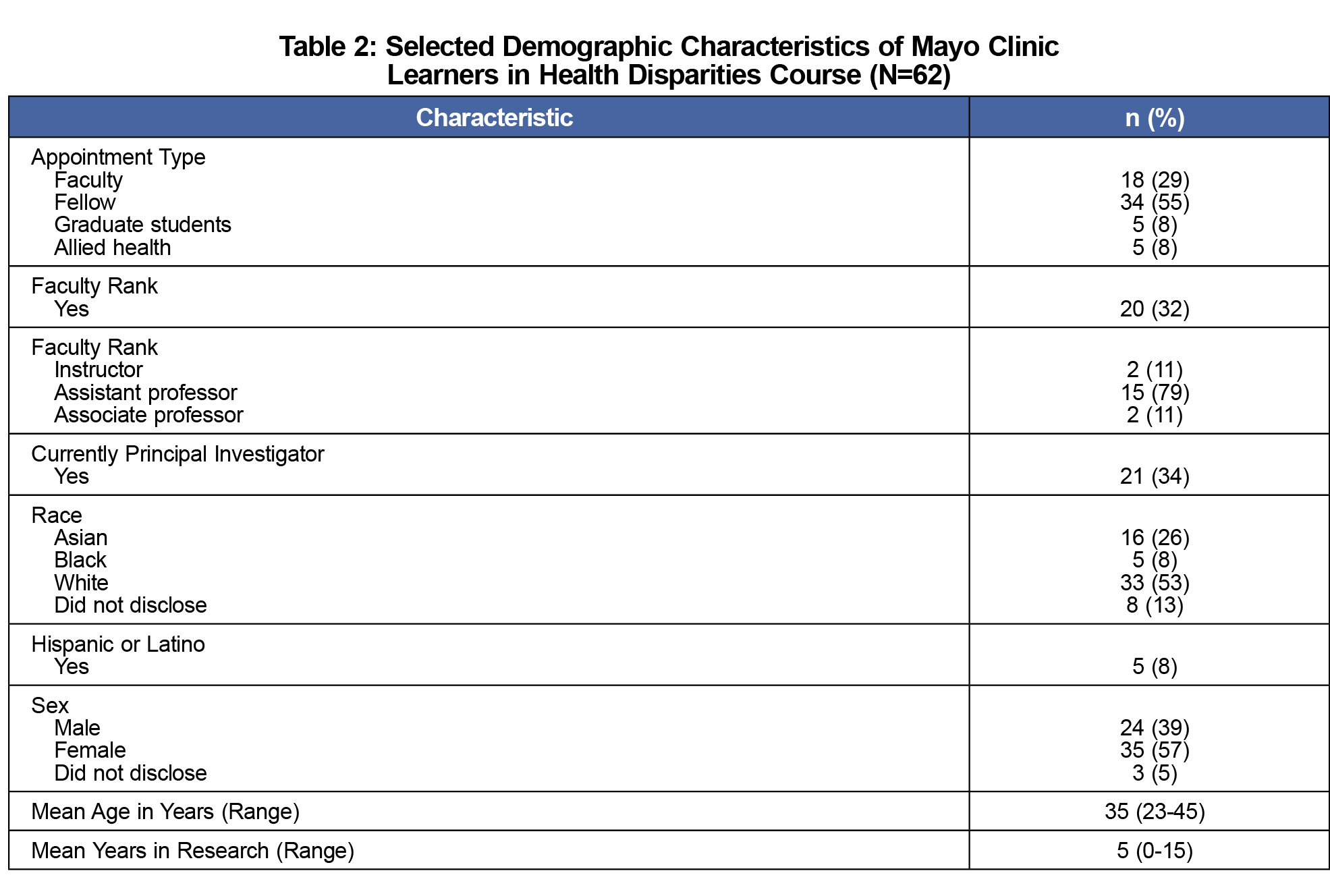
Over half of the learners were fellows (n=34, 55%) with the remaining identifying as faculty, graduate student, or allied health staff (Table 2). A total of 56 (90%) learners completed both assessments. Learners averaged 5 years of experience in research (range: 0-15 years); the mean age of learners was 35 years (range: 23-45 years).
We compared the pre/postassessment of learners (Table 3). There was a statistically significant difference in learners’ perceptions of how patients are treated based on gender identity (P=0.02) and sexual orientation (P=0.04). A marginal effect was noted on learners’ perceptions of how patients are treated based on whether or not a patient had a physical disability (P=0.06).
Academic medical centers are responsible for providing training that increases learners’ knowledge of health disparities. Our curriculum focused on the prevalence of health disparities related to patient demographics such as race, ethnicity, age, gender, sexual orientation, geographic location, and socioeconomic status. We also took into account the complexity of social determinants of health, and biases that impact equity in health care.5-10 After completing the course, learners’ perceptions of health disparities changed overall. This increased knowledge has the potential to reduce health-related disparities, resulting in better care for patients. Our course serves as a model for an introductory-level course to increase awareness of health disparities in context of patient care and research.
A limitation of the course is that it was only 6 weeks in duration, with a small sample size. During online data collection, we noted a problem and switched from online to paper survey. Another limitation is pre/poststudy design because maturation effect and temporally concurrent factors were not considered. Notably, the unpaired analysis permitted us to include all learners, so no individuals were excluded due to having data only at the pretest. An unpaired analysis is considered statistically conservative, because it is less likely to achieve statistical significance than the paired analysis in which each person serves as his or her own control.
Our next steps are to shorten our assessment and to change questions based on updated health disparities literature. Another step is evaluating learners’ use of the information over an extended period beyond the course in clerkships. We may also compare learners to a cohort not enrolled in the course to determine the impact on application of the course material.
Acknowledgments
The authors express their appreciation to the Center for Clinical and Translational Science Educational Resources for the support with curriculum design and administration of the pre/postassessments. Additional thanks to Kimberly Kinnoin for editorial support for the submission of this manuscript.
Financial Support: This publication was made possible by Clinical and Translational Science Awards Grant Number UL1 TR000135 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the NIH.
Presentations: Presented at the 13th Research Centers in Minority Institutions International Symposium on Health Disparities, San Juan, PR, December 10-13, 2012.
References
- Hasnain M, Massengale L, Dykens A, Figueroa E. Health disparities training in residency programs in the United States. Fam Med. 2014;46(3):186-191.
- Greene EL, Thomas CR Jr. Minority health and disparities-related issues: part II. Med Clin (Barc). 2005;89(5):xi-xii.
- Smith WR, Betancourt JR, Wynia MK, et al. Recommendations for teaching about racial and ethnic disparities in health and health care. Ann Intern Med. 2007;147(9):654-665. https://doi.org/10.7326/0003-4819-147-9-200711060-00010
- Henry J. Kaiser Family Foundation. National Survey of Physicians. 2002.
- Bolnick DA. Combating racial health disparities through medical education: the need for anthropological and genetic perspectives in medical training. Hum Biol. 2015;87(4):361-371. https://doi.org/10.13110/humanbiology.87.4.0361
- Drobac P, Morse M. Medical education and global health equity. AMA J Ethics. 2016;18(7):702-709. https://doi.org/10.1001/journalofethics.2016.18.7.medu1-1607
- Kelly R. Kelly Report: Health Disparities in America. Braintrust CBCH, ed. Washington, DC: United States Congress; 2015.
- Maldonado ME, Fried ED, DuBose TD, Nelson C, Breida M. The role that graduate medical education must play in ensuring health equity and eliminating health care disparities. Ann Am Thorac Soc. 2014;11(4):603-607. https://doi.org/10.1513/AnnalsATS.201402-068PS
- Patow C, Bryan D, Johnson G, et al. Who’s in our neighborhood? Healthcare disparities experiential education for residents. Ochsner J. 2016;16(1):41-44.
- Powell T, Garcia KA, Lopez A, Bailey J, Willies-Jacobo L. University of California San Diego’s Program in Medical Education-Health Equity (PRIME-HEq): Training future physicians to care for underserved communities. J Health Care Poor Underserved. 2016;27(3):937-946. https://doi.org/10.1353/hpu.2016.0109




There are no comments for this article.