Introduction: The completion of a patient’s disability assessment form (DAF) is a task expected of family and internal medicine physicians. Residency curricula rarely address this task. Thus, some residents are reluctant to conduct functional assessments because of inadequate training, the time required to conduct such an exam, and fear of jeopardizing the doctor-patient relationship. This article describes a curricular intervention to prepare residents to complete a focused functional capacity assessment during a 30-minute office visit.
Methods: Developing the curriculum for DAF completion involved a literature review, conducting needs assessment interviews, and a review of existent residency training materials. Instructional strategies included lecture, panel discussions, and demonstrations. The learner evaluation strategies were knowledge tests, direct observation of residents, and a review of disability cases with an expert panel consisting of federally certified Social Security Administration workers. This work represents information gained from four pilot tests.
Results: The residents’ knowledge scores increased significantly. Knowledge of state, federal, and employer disability programs increased as well as their ability to distinguish sedentary, light, medium, and heavy work capacity when related to patients’ medical conditions. All the residents could perform the assessment, but none of them were confident that they could complete the DAF in a 30-minute office visit. This was an expected outcome.
Conclusions: It is possible to teach family and internal medicine residents the knowledge and skills required to determine their patients’ functional capacity as it relates to a specific problem. By applying what they have learned to their patients, they will eventually be able to complete a DAF during a 30-minute office visit. Residency programs are encouraged to incorporate a functional assessment curriculum.
The completion of patients’ disability assessment forms (DAF) is a task frequently performed by family physicians.1 Each year, approximately 2.5 million new disability applications are submitted to the Social Security Administration (SSA).2 Each application requires assessment of the patient’s residual functional capacity (RFC), level of education, work experience, and age prior to determining work ability.3 An accurate RFC assessment is critical because it determines the future work and benefits available to the patient.
The SSA asks primary care physicians to complete DAFs because they represent the physician of first contact, the broad base of their training, and established doctor-patient relationship.1,3 Lack of familiarity with the process of disability determination, inadequate skills to conduct such an assessment, insufficient clinic time, and fear of jeopardizing the doctor-patient relationship make DAF completion a daunting task.4 Most primary care residency training programs do not provide structured training in determining RFC nor much information about state and federal disability programs.4-8 RFC exams include testing for a patient’s consistency of effort and strength as it relates to things like maximum voluntary effort at hand grip, rapid exchange grip, standard hand grip, and pinch strength.9 Such training is helpful in completing a DAF. When comparing information attained based on a clinical exam versus a residual functional capacity exam, the latter was found to be most helpful in disability determination.9,10 Evidence supports the utility and reliability of an RFC to provide objective data on a person’s functional capabilities in a clinical setting.9-11
A search of health professionals’ literature returned several articles addressing the importance of providing residents and practitioners with the appropriate knowledge, skills, and attitudes for working with their impaired patients.11-15 These subjects, in addition to completing DAF and RFC assessments, are prevalent amongst physical medicine and rehabilitation residency programs as well as physical therapy training programs. However, the search did not yield curricula for family or internal medicine residents (FIMR). The Association of American Medical Colleges does not list such information as necessary for completion of FIMR programs.
PGY1-3 residents of the Sparrow Hospital FIMR Programs were facing similar challenges in completing patients’ DAF. Thus, the Sparrow-Michigan State University residency faculty decided to champion a pilot curricular intervention that would better prepare their residents for completing an RFC assessment and DAF during an office visit. The overall goal of this pilot curriculum was to conduct a focused RFC assessment during a 30-minute office visit and write appropriate work restrictions. This curricular intervention is an attempt to highlight curriculum deficits as they relate to SSA disability form completion training. It may encourage others to do more trials for further development.
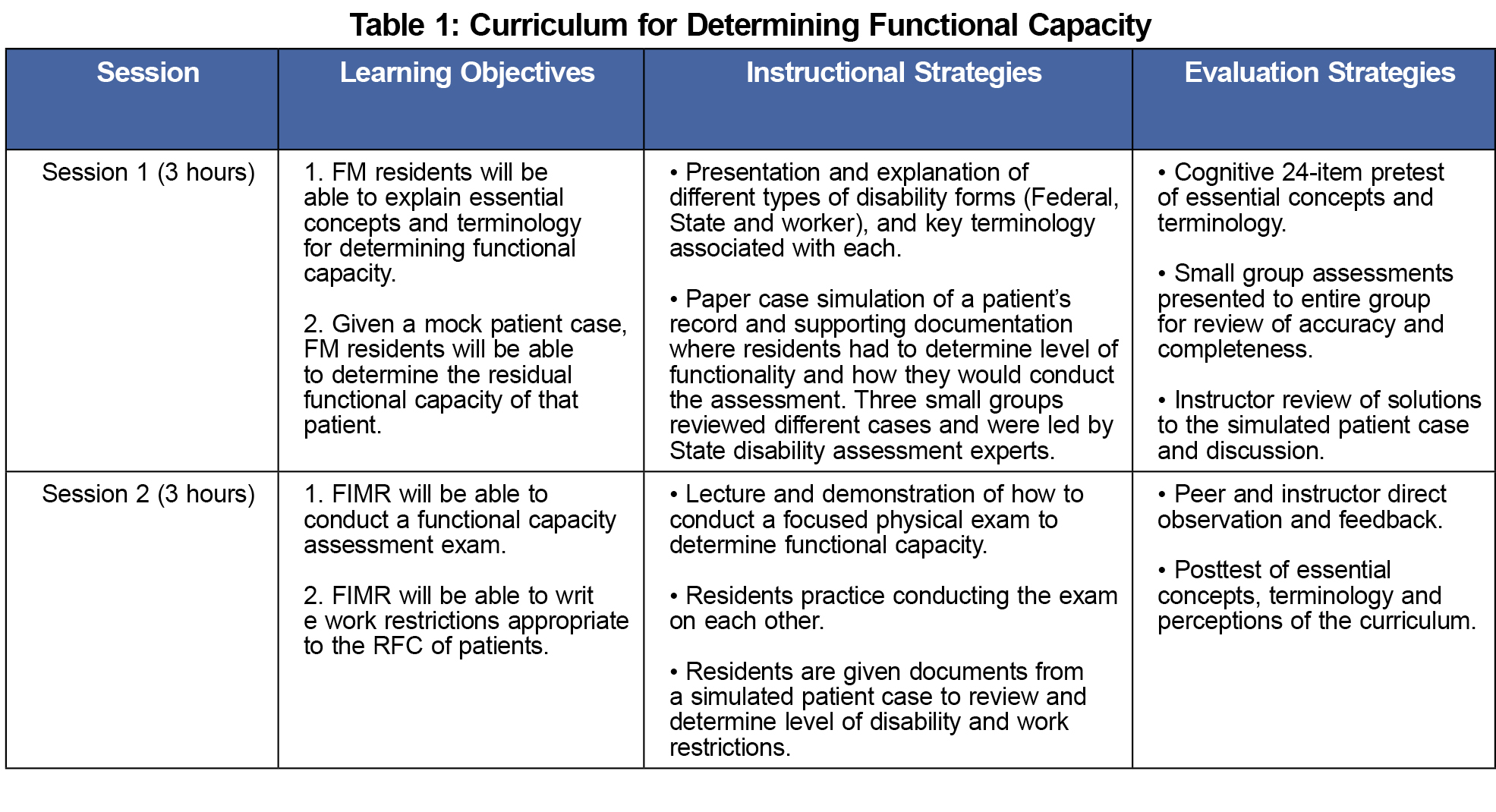
Developing the curriculum involved a PubMed and Google Scholar literature review, interviews with FIMR faculty, physical therapists’ input, and federally certified SSA workers. One researcher was trained and certified by the federal government in SSA criteria for disability. The curriculum was developed and implemented as two 3-hour sessions for each program of FIMR.19 A total of 66 FIMR participated in the pilot curriculum project from October 2013 to October 2016. Table 1 shows a summary of curriculum implementation.
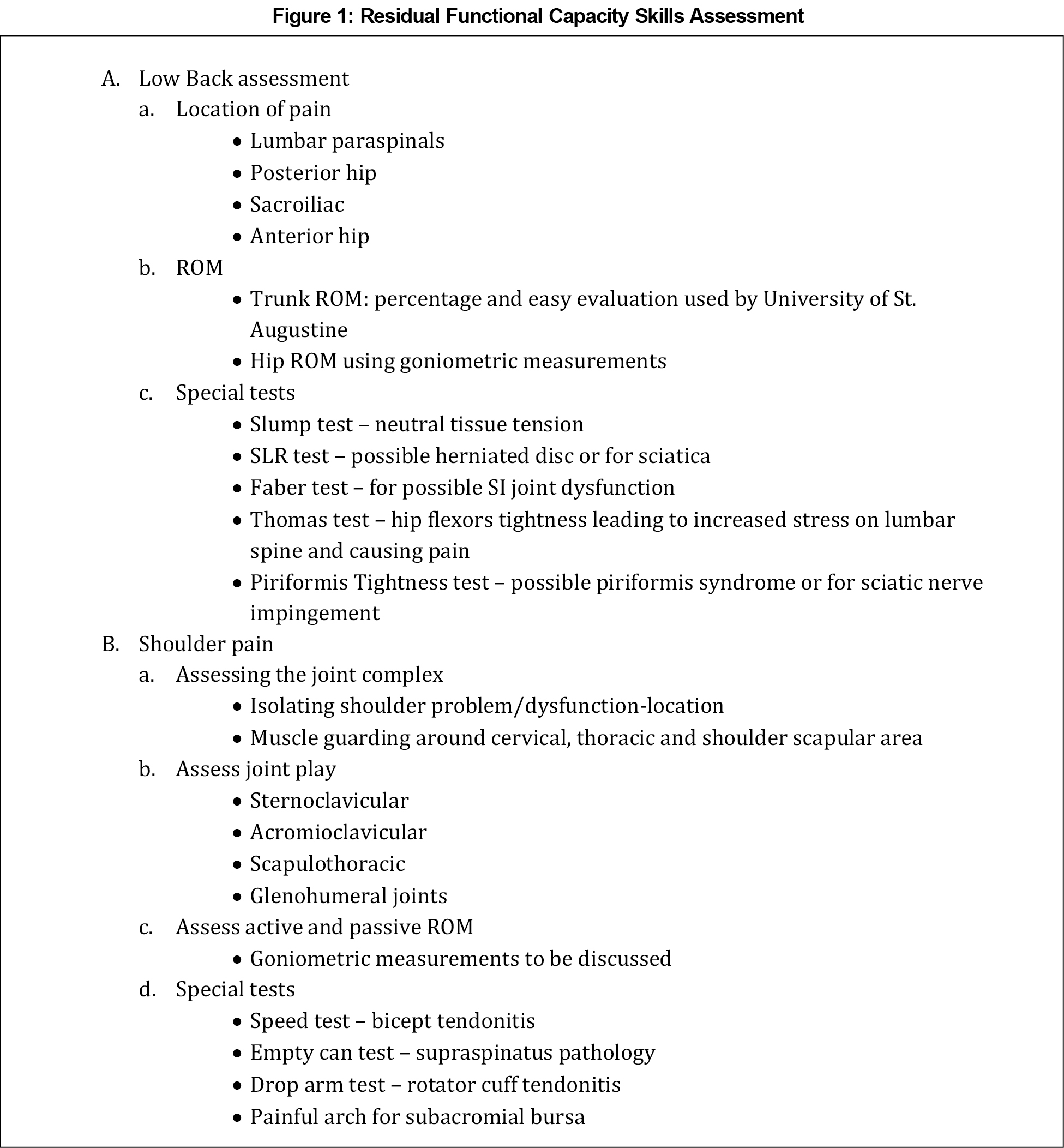
The learner evaluation strategies involved the use of (a) pre and post optional knowledge questions, (b) a structured checklist for direct observation of selected components of the RFC exam (Figure 1), and (c) a review of mock disability cases with an expert panel consisting of federally certified SSA workers.19
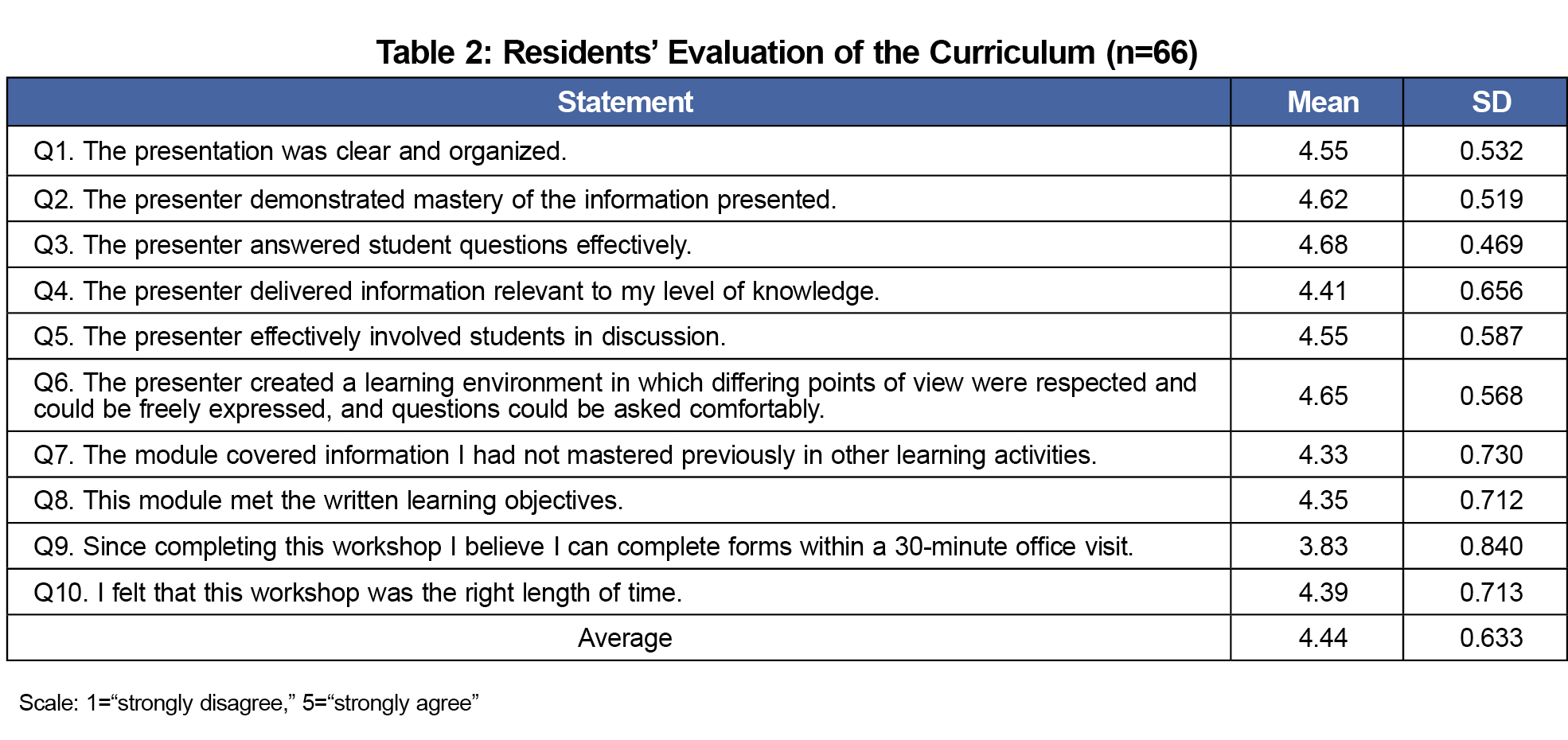
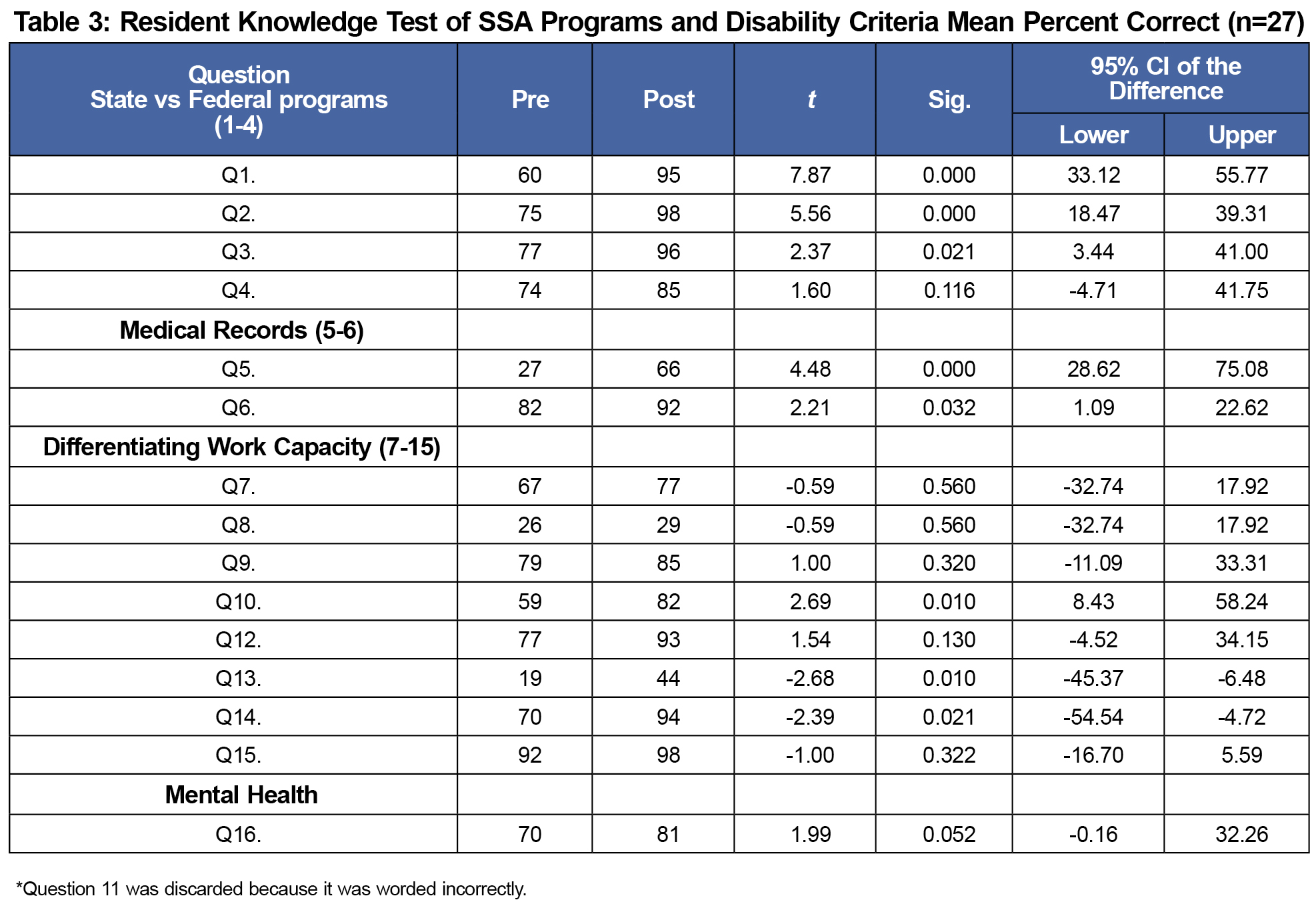
The curriculum for FIMR was evaluated on a 5-point Likert scale using: (a) 10 mandatory curriculum evaluation questions administered during the final workshop section for all 66 residents (Table 2), (b) 15 Yes/No pre- and postworkshop test questions (Table 3), and (c) four 5-point Likert scale perception questions pre- and postworkshop (Table 4). Independent sample t tests were used to compare pre- and postworkshop data. Statistical significance was set at P<0.05. Michigan State University and Sparrow Hospital’s institutional review boards approved this curriculum project.
All 66 FIMRs completed the curriculum evaluation. The mean scores ranged from 3.83 to 4.68, with an overall mean of 4.44 on the 10 questions (Table 2). A total of 27 out of 66 FIMRs completed the knowledge test and perception questions. Results showed significant improvement on nine out of 15 knowledge test questions regarding SSA programs and disability criteria. The posttest scores for the remaining six questions were higher than the pretest scores, but not statistically significant (Table 3).
Table 4 indicates the perception of FIMRs in their ability to complete disability forms before and after the workshop. There were significant improvements in two of the four pre-perception questions. All four post-perception questions revealed there was improvement for completing DAF.
People with disabilities are twice as likely to find health care provider skills and equipment inadequate to meet their needs, three times as likely to be denied care, and four times as likely to be treated badly by health care providers.16 It is a known fact that impairment is more common than death before the age of 65.16 For these reasons, it is essential that FIMR programs intentionally incorporate curriculum directed at acquired disability, as a result of eroding RFC secondary to chronic disease.13,17,18 Such information will improve historic documentation of chronic disorders and make completion of DAF less daunting.
Encapsulated by the learning objectives of this pilot curriculum was the intent to increase residents’ knowledge, skills, and perceptions of completing patient DAF during an office visit. Through the curriculum evaluation, residents indicated that they did learn information they had not received or mastered in other learning activities. All residents demonstrated increased knowledge of SSA criteria and RFC exam skills (specifically arm, hip, and low back), but were not confident they could complete a DAF in a 30-minute office visit. Even experienced physicians struggle with this. It requires familiarity with tools in one’s electronic medical record software, a process for handling DAF requests, and some knowledge of the SSA definitions of sedentary, light, medium, and heavy work. Educators made it clear that the 6-hour workshop shared information that, when used over the years, would make DAF completion less daunting.
Studies that have shown that clinical exams coupled with functional capacity exams give the best information for disability determination.9,10 Unfortunately, medical insurance plans do not cover functional capacity exams. However, they do cover problem-focused exams done by physical therapists and physiatrists. Clinicians can refer to such professionals for consultations that will help them in completing the DAF.
Teaching residents how to determine a patient’s RFC can reduce anxiety, frustration, and time required to complete related paperwork. This translates to practicing physicians that are more comfortable with the SSA process of disability determination. The societal benefits are timely and accurate information that will expedite the disability process, and in some cases may allow determination to be made without requiring additional resources. This benefits the patient in that they are privy to Medicaid services and financial assistance.
In future iterations of this curriculum, we plan to create an office protocol for handling DAF requests. We will add more exam room skills that will enhance residents’ ability to determine how long a patient can sustain activities during an 8-hour work day. We will also add a structured didactic component that involves videotaping such office visits so that residents can review the process with their faculty for direct feedback.
When using this curriculum, it is recommended to choose patient cases based on the needs of residents. The developers of this curriculum suggest that DAF forms from the local state department of human services be used and that the educational team consist of local SSA workers, physical therapists/PM&R doctors, and a clinician well versed in the musculoskeletal exam.1,4,5,7,16
Acknowledgments
The authors recognize William Anderson, PhD, Samuel Etim and Mr Chinmay Zinzuvadia, PT, DPT, CIMT of Lansing Rehabilitation Services, PLLC for their contributions to this curriculum. We also thank the State of Michigan Social Security Administration, in particular, Charles Jones, Dave Ludington, Brice Edmonds, Jenna Shackelford, Dr Sharon Bland-Brady, and Dr Hirute Marsha-Scarlet.
References
- Maness DL, Khan M. Disability evaluations: more than completing a form. Am Fam Physician. 2015;91(2):102-109.
- Leigh JP, Markowitz SB, Fahs M, Shin C, Landrigan PJ. Occupational injury and illness in the United States. Estimates of costs, morbidity, and mortality. Arch Intern Med. 1997;157(14):1557-1568. https://doi.org/10.1001/archinte.1997.00440350063006.
- Holmes EB. Impairment rating and disability determination. Medscape. https://emedicine.medscape.com/article/314195-overview?
pa=BwPjPNVru6qQOOm25irpWG6cQDnoJ5GCh1j%2BPicaluz3cY7V%2FT6
hcWO%2BhDKSQ%2FC35zu8jhRO1Gk3ky%2BvTO4hEaMMvXjUcyZ8uhFN
FUtVAb4%3D. Updated April 6, 2016. Accessed March 15, 2018.
- Potts S, Shields S, Upshur C. Preparing Future Leaders: An Integrated Quality Improvement Residency Curriculum. Fam Med. 2016;48(6):477-481.
- Sarmiento C, Miller SR, Chang E, Zazove P, Kumagai AK. From Impairment to Empowerment: A Longitudinal Medical School Curriculum on Disabilities. Acad Med. 2016;91(7):954-957. https://doi.org/10.1097/ACM.0000000000000935.
- Robey KL, Minihan PM, Long-Bellil LM, Hahn JE, Reiss JG, Eddey GE; Alliance for Disability in Health Care Education. Teaching health care students about disability within a cultural competency context. Disabil Health J. 2013;6(4):271-279. https://doi.org/10.1016/j.dhjo.2013.05.002.
- Symons A, McGuigan D, Aki E. A curriculum to teach medical students to care for people with disabilities: development and initial implementation. BMC Medical Educ. 2009;9(78).
- Long-Bellil LM, Robey KL, Graham CL, Minihan PM, Smeltzer SC, Kahn P; Alliance for Disability in Health Care Education. Teaching medical students about disability: the use of standardized patients. Acad Med. 2011;86(9):1163-1170. https://doi.org/10.1097/ACM.0b013e318226b5dc.
- Peppers D, Figoni SF, Carroll BW, Chen MM, Song S, Mathiyakom W. Influence of functional capacity evaluation on physician’s assessment of physical capacity of veterans with chronic pain: a retrospective analysis. PM&R. 2017;9(7):652-659. https://doi.org/10.1016/j.pmrj.2016.10.011.
- Fu JB, Osborn MP, Silver JK, et al. Evaluating disability insurance assistance by physiatrists at a cancer center. Am J Phys Med Rehabil. 2017;96(7):523–528. https://doi.org/10.1097/PHM.0000000000000641.
- Kirschner KL, Curry RH. Educating health care professionals to care for patients with disabilities. JAMA. 2009;302(12):1334-1335. https://doi.org/10.1001/jama.2009.1398.
- Minihan PM, Robey KL, Long-Bellil LM, et al; Alliance for Disability in Health Care Education. Desired educational outcomes of disability-related training for the generalist physician: knowledge, attitudes, and skills. Acad Med. 2011;86(9):1171-1178. https://doi.org/10.1097/ACM.0b013e3182264a25.
- Shakespeare T, Kleine I. Educating health professionals about disability: a review of interventions. Health and Social Care Education. 2013;2(2):20-37. https://doi.org/10.11120/hsce.2013.00026.
- O’Fallon E, Hillson S. Brief report: physician discomfort and variability with disability assessments. J Gen Intern Med. 2005;20(9):852-854. https://doi.org/10.1111/j.1525-1497.2005.0177.x.
- Colledge A, Homes E, Soo Hoo E, Johns R, Kuhnlein J, De Berard S. Motivation and determination (sincerity of effort): the performance APGAR model. Disability Medicine. 2001;1(2):5-18.
- World Health Organization. World report on disability. Geneva: World Health Organization; 2011.
- Moroz A, Gonzalez-Ramos G, Festinger T, Langer K, Zefferino S, Kalet A. Immediate and follow-up effects of a brief disability curriculum on disability knowledge and attitudes of PM&R residents: a comparison group trial. Med Teach. 2010;32(8):e360-e364. https://doi.org/10.3109/0142159X.2010.490602.
- Graham CL, Brown RS, Zhen H, McDermott S. Teaching medical students about disability in family medicine. Fam Med. 2009;41(8):542-544.
- Sekoni KI, Zinzuvadia C. Accurate Disability Form Completion in a 30-Minute Office Visit. https://resourcelibrary.stfm.org/viewdocument/accurate-disability-form-completion. Accessed March 15, 2018.




There are no comments for this article.