Introduction: Burnout during medical training, including medical school, has gained attention in recent years. Resiliency may be an important characteristic for medical students to have or obtain. The aim of this study was to examine the level of resiliency in fourth-year medical students and whether certain characteristics were associated with students who have higher levels of resiliency.
Methods: Subjects were fourth-year medical students who completed a survey during a required end-of-year rotation. The survey collected subjects’ demographic information including age, gender, race, ethnicity, marital status, and chosen specialty. They were also asked to complete the Brief Resilience Scale (BRS) and answer questions that assessed personal characteristics.
Results: The response rate was 92.4%. Most respondents had personal time for themselves after school (92.6%), exercise or participate in physical activity for at least 30 minutes most days of the week (67.2%), were able to stop thinking about medical school after leaving for the day (58.2%), and had current financial stress (51.6%). No differences were noted in demographic information among students across specialty categories. A higher BRS score was associated with being male and having the ability to stop thinking about school.
Conclusions: BRS scores in medical students are associated with specific demographic characteristics and the ability to stop thinking about school. Addressing the modifiable activities may assist students with increasing their resiliency and potentially decreasing their risk of burnout.
Professional burnout is a syndrome characterized by emotional exhaustion, feelings of cynicism or depersonalization, and decreased sense of personal accomplishment.1-3 A national survey completed in 2012 of all physician types found 46% of physicians reported at least one symptom of burnout.1 Family, internal, and emergency medicine physicians had the highest rates of burnout compared to other specialties, particularly the surgical subspecialties.
Studies using the Maslach Burnout Inventory indicate medical students are impacted by burnout.4-6 In a study of students at seven medical schools in 2008, approximately 50% of students experienced burnout.4 Among these students, 40.1% had high emotional exhaustion, 31.8% had high depersonalization, and 30.6% had a low sense of personal accomplishment. In another study, medical students were found to be at slightly greater risk for burnout as they progressed through medical school.6
As suggested by Elkins,6 further research regarding student burnout is needed in order to develop and implement appropriate interventions. Furthermore, more studies are needed regarding the relationships among personality traits, resilience, burnout, work satisfaction, and the physician training environment.7 Resiliency (defined as the ability of an individual to respond to stress in a healthy, adaptive way) may be an important characteristic for medical students to have or further develop in order to prevent or address symptoms of burnout. Studies conducted to identify traits or characteristics associated with physician well-being and resiliency found that certain factors associated with resident well-being include building of competence, strong social relatedness, sleep, and time away from work.8 Medical students with higher resilience levels were found to have a better quality of life and better perception of educational environment.9 Emotional skills training embedded into the medical school curriculum was suggested as a method to reduce psychological distress among medical students.10
The aim of this study was to examine the level of resiliency in fourth-year medical students and whether certain characteristics are associated with students who have higher levels of resiliency. This information can be used to identify students who may be at risk for burnout and target students who may benefit from further development of resiliency.
Subjects and Survey Items
We asked an entire class of fourth-year medical students to complete a survey during a required end-of-year rotation. This rotation occurred after the students matched into their residency program and prior to their graduation from medical school.
We developed and reviewed a survey that asked for subjects’ demographic information, including age, gender, race, ethnicity, marital status, and chosen specialty. The survey included questions addressing resiliency, and it used the Brief Resilience Scale (BRS). The BRS is a reliable means of assessing resilience, and may provide unique and important information about individuals coping with stressors.11 To identify additional factors that may add to resiliency, we developed and included additional questions assessing personal characteristics.
Analysis
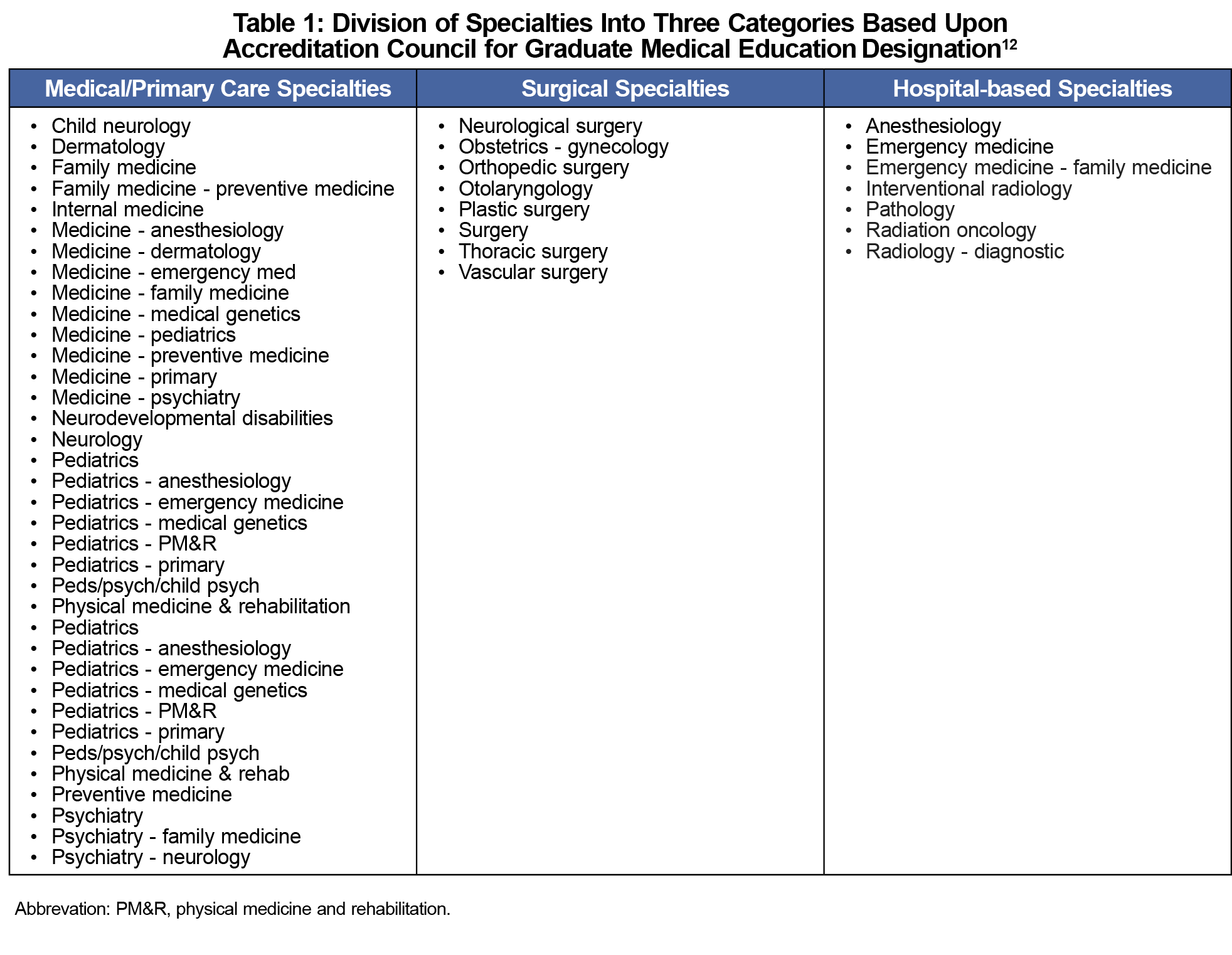
We performed descriptive statistics on the demographic information. We made comparisons between students planning to enter medicine/primary care specialties, surgery and associated specialties, and hospital-based specialties using Accreditation Council for Graduate Medical Education (ACGME) categories (Table 1).12 We used Wilcoxon rank-sum tests to determine whether the three groups shared similar distributions of resilience response and to test for associations between BRS score and the demographic information, and between BRS scores and the additional questions. We used Fisher exact tests to test for associations between the medical specialty groups and demographic information/additional questions. We also used Fisher exact tests to test for associations between gender and each additional question. For further analyses, we divided the respondents into tertiles based upon their BRS score (low, medium, and high). Statistical significance was defined as P<.05 level of confidence. We performed statistical analyses with the statistical computer package R (version 3.5.1).
The University of Florida Institutional Review Board approved this project as exempt.
The response rate for the survey was 92.4% (122/132). A majority of respondents were female, white, and single, with an average age of 26.9 (+2.4) years (Table 2). Most respondents had personal time for themselves after school (92.6%), exercised or participated in physical activity for at least 30 minutes most days of the week (67.2%), were able to stop thinking about medical school after leaving for the day (58.2%), and had current financial stress (51.6%).
No differences were noted in demographic information among students across specialty categories. Additionally, resilience score did not differ among respondents based upon their specialty category. Students pursuing a career in the medical specialties were less likely to consider their specialty as competitive.
We divided the respondents into tertiles (low BRS score <2.78, medium BRS score <2.78 and <3.89, and high BRS score <3.89). A higher BRS score was found to be associated with being male and having the ability to stop thinking about school (Table 3). Students who identified themselves as Asian were associated with low BRS scores. Finally, being married and having a career prior to medical school were the only demographic characteristics significantly associated with a positive response to any of the questions asked on the BRS (P=.04).
BRS scores in medical students were associated with being male and the ability to stop thinking about school. No differences were found in resiliency levels based upon their chosen specialty category. Furthermore, the scores were not associated with performance in medical school. The lack of association of resiliency level with specialty category suggests that students do not necessarily have a certain level of resiliency used to select their specialty category and no specific specialty category is associated with students with higher or lower levels of resiliency.
Students entering a surgical or hospital-based specialty more often felt their specialty was competitive. The BRS scores did not vary based on this finding. Whether this perception was based upon exposure to these specialties and other factors such as board scores of candidates is not known and require additional study.
Several findings may assist students as they work to improve resilience and decrease risk of burnout. Techniques used to assist students to gain the ability to stop thinking about medical school after leaving for the day should be developed and made available. While over 90% of students reported having personal time after school, only about two-thirds participated in the recommended amount of exercise and physical activity. Reminders concerning the overall benefits of regular physical activity and readily available opportunities for exercise should be considered.
This study has limitations. The survey was used in a single fourth-year class of medical students at one medical school. The results may differ if a larger population were studied. Additionally, the survey was given after students had already matched into their specialties, which may have affected some of their responses.
Certain traits and activities are associated with higher levels of resilience in medical students. Addressing the modifiable activities may assist students with increasing their resiliency, potentially decreasing the risk or severity of symptoms associated with burnout.
Acknowledgments
The authors dedicate this article to Sey Park, MD, who unexpectedly passed on January 9, 2018. He was the inspiration and leader of this study and was committed to the health and wellness of students, residents, and attending physicians.
References
- Shanafelt TD, Boone S, Tan L, et al. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012;172(18):1377-1385. https://doi.org/10.1001/archinternmed.2012.3199
- Dyrbye LN, Shanafelt TD, Thomas MR, Durning SJ. Brief observation: a national study of burnout among internal medicine clerkship directors. Am J Med. 2009;122(3):310-312. https://doi.org/10.1016/j.amjmed.2008.11.008
- Ishak WW, Lederer S, Mandili C, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1(2):236-242. https://doi.org/10.4300/JGME-D-09-00054.1
- Dyrbye LN, Thomas MR, Massie FS, et al. Burnout and suicidal ideation among U.S. medical students. Ann Intern Med. 2008;149(5):334-341. https://doi.org/10.7326/0003-4819-149-5-200809020-00008
- Goel AD, Akarte SV, Agrawal SP, Yadav V. Longitudinal assessment of depression, stress, and burnout in medical students. J Neurosci Rural Pract. 2016;7(4):493-498. https://doi.org/10.4103/0976-3147.188625
- Elkins C, Plante KP, Germain LJ, Morley CP. Burnout and Depression in MS1 and MS3 Years: A Comparison of Cohorts at One Medical School. Fam Med. 2017;49(6):456-459.
- Sullivan GM. The burnout conundrum: nature versus nurture? J Grad Med Educ. 2016;8(5):650-652. https://doi.org/10.4300/JGME-D-16-00605.1
- Raj KS. Well-being in residency: A systemic review. J Grad Med Educ. 2016;8(5):674-684. https://doi.org/10.4300/JGME-D-15-00764.1
- Tempski P, Santos IS, Mayer FB, et al. Relationship among medical student resilence, educational environment, and quality of life. PLoS One. 2015;10(6):e0131535. https://doi.org/10.1371/journal.pone.0131535
- Bore M, Kelly B, Nair B. Potential predictors of psychological distress and well-being in medical students: a cross-sectional pilot study. Adv Med Educ Pract. 2016;7:125-135. https://doi.org/10.2147/AMEP.S96802
- Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194-200. https://doi.org/10.1080/10705500802222972
- Accreditation Council for Graduate Medical Education. Basics of Accreditation for New Program Coordinators. https://www.acgme.org/Meetings-and-Educational-Activities/Other-Educational-Activities/Courses-and-Workshops/Basics-of-Accreditation. Accessed September 20, 2019.





There are no comments for this article.