Drug overdose is now the leading cause of death for Americans under age 50 years.1 New Mexico is ranked 17th nationwide for overdose deaths, and New Mexico overdose deaths tripled between 1990 and 2015 (Figure 1).2
Current evidence shows that naloxone distribution reduces opioid-related overdose deaths and is cost effective.3-7 The American Academy of Family Physicians recommends family physicians prescribe naloxone, an opioid reversal agent, to patients at high risk of overdose and support community naloxone distribution programs.8
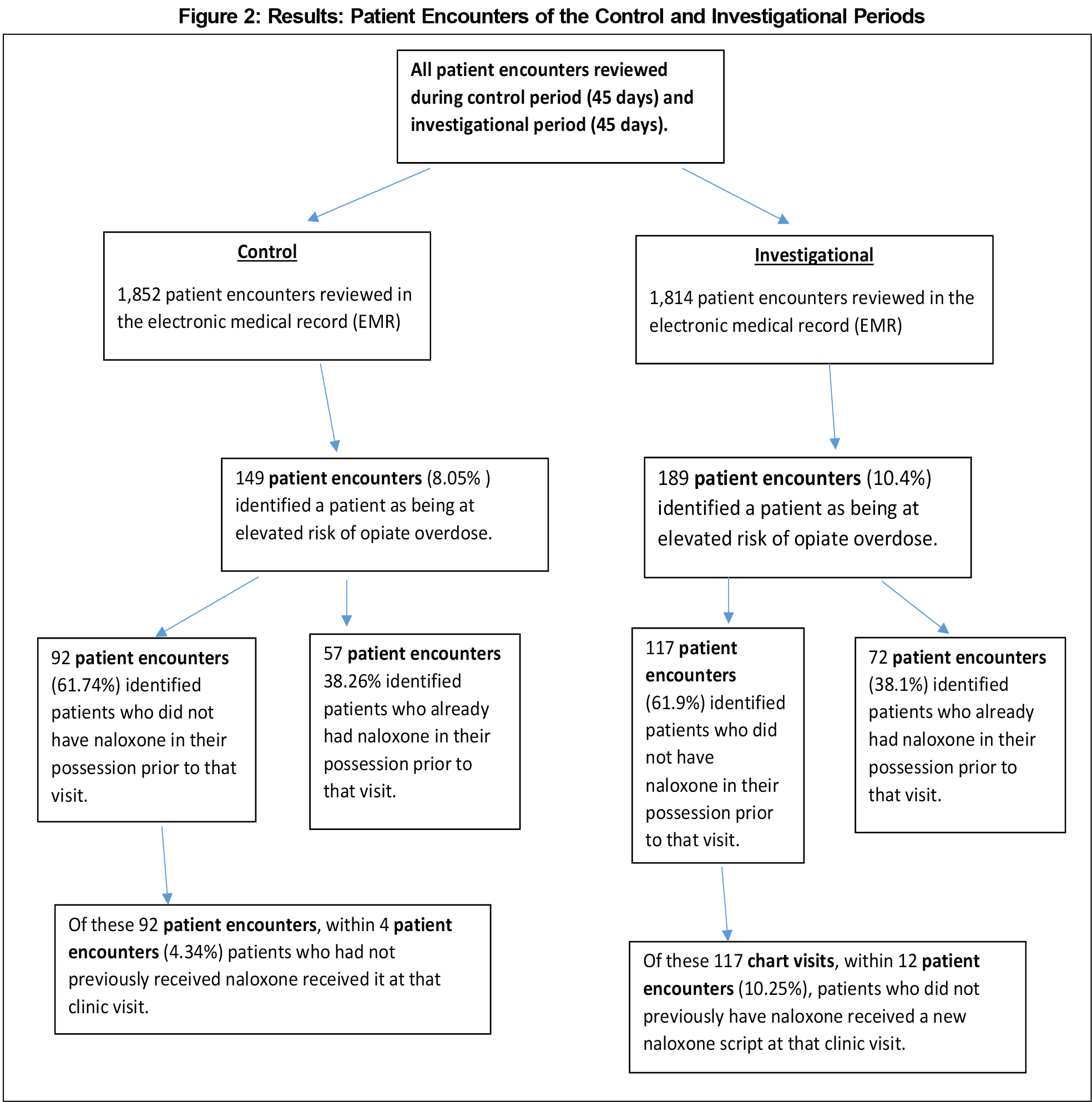
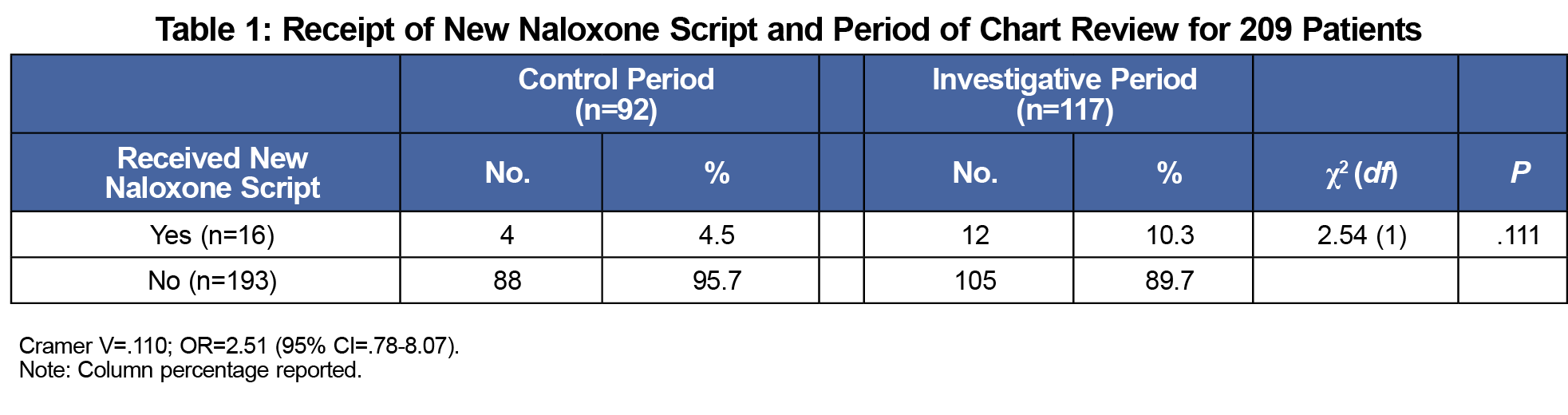
This project seeks to decrease opioid overdose deaths in a community by increasing the number of people with naloxone, and assesses effectiveness of a brief intervention that can be performed in a typical primary care clinic with implications for harm reduction at the community level.




There are no comments for this article.