Introduction: With the estimated future shortage of primary care physicians there is a need to recruit more medical students into family medicine. Longitudinal programs or primary care tracks in medical schools have been shown to successfully recruit students into primary care. The aim of this study was to examine the characteristics of primary care tracks in departments of family medicine.
Methods: Data were collected as part of the 2016 CERA Family Medicine Clerkship Director Survey. The survey included questions regarding the presence and description of available primary care tracks as well as the clerkship director’s perception of impact. The survey was distributed via email to 125 US and 16 Canadian family medicine clerkship directors.
Results: The response rate was 86%. Thirty-five respondents (29%) reported offering a longitudinal primary care track. The majority of tracks select students on a competitive basis, are directed by family medicine educators, and include a wide variety of activities. Longitudinal experience in primary care ambulatory settings and primary care faculty mentorship were the most common activities. Almost 70% of clerkship directors believe there is a positive impact on students entering primary care.
Conclusions: The current tracks are diverse in what they offer and could be tailored to the missions of individual medical schools. The majority of clerkship directors reported that they do have a positive impact on students entering primary care.
A 2014 US Institute of Medicine report highlighted the need for graduate medical education (GME) to produce more primary care physicians to care for underserved and rural populations.1 An estimated additional 52,000 primary care physicians will be needed within the next 10 years to meet the population’s needs.2,3 The Council on GME estimates it will require 40% of practicing physicians to be in primary care to meet patient demands, which is an 8% increase from the current level.4,5
Suggestions for increasing student interest in family medicine include training students in high-performing ambulatory sites; creating a culture that values primary care, including population health education; and supporting primary care teaching faculty through awarding relative value units (RVUs) for precepting and teacher training, etc.4 Studies investigating student specialty choice have found several factors related to students choosing family medicine, including having a rural background, believing primary care is important, having low income earning expectations, attending a public medical school, and having positive faculty role models.6 Systematic reviews evaluating the impact of interventions aimed at recruiting students to a primary care career have found longitudinal programs with experiences in primary care and/or rural health were the only consistently successful interventions.3,7
Tracks are usually offered in addition to conventional curriculum and may include a variety of components.7 The aim of this study was to characterize longitudinal primary care tracks lasting at least 1 year, determine their prevalence, and estimate their impact on students entering primary care residencies. We hypothesized that while most medical schools do not offer longitudinal primary care tracks, clerkship directors (CD) at institutions where they are offered would feel they influence students to pursue primary care.
The questions of this study were administered to US and Canadian allopathic family medicine CDs as part of a larger omnibus survey conducted annually by the Council of Academic Family Medicine Educational Research Alliance (CERA). The survey methods and sample demographics have been presented previously.8
The CERA steering committee evaluated questions for consistency with the overall project aim, readability, and existing evidence of reliability and validity. Pretesting was done on family medicine educators who were not part of the target population. Questions were modified following pretesting for flow, timing, and readability. The American Academy of Family Physicians Institutional Review Board (IRB) and the University of Florida IRB approved the study. Data were collected between August 9, 2016 and October 9, 2016.
The sampling frame for the survey was institutional representatives—such as the CD or their designee—of allopathic medical schools. Email invitations to participate were delivered with the survey utilizing the online program SurveyMonkey. Four follow-up emails were sent after the initial email invitation to encourage nonrespondents to participate.
Survey Items
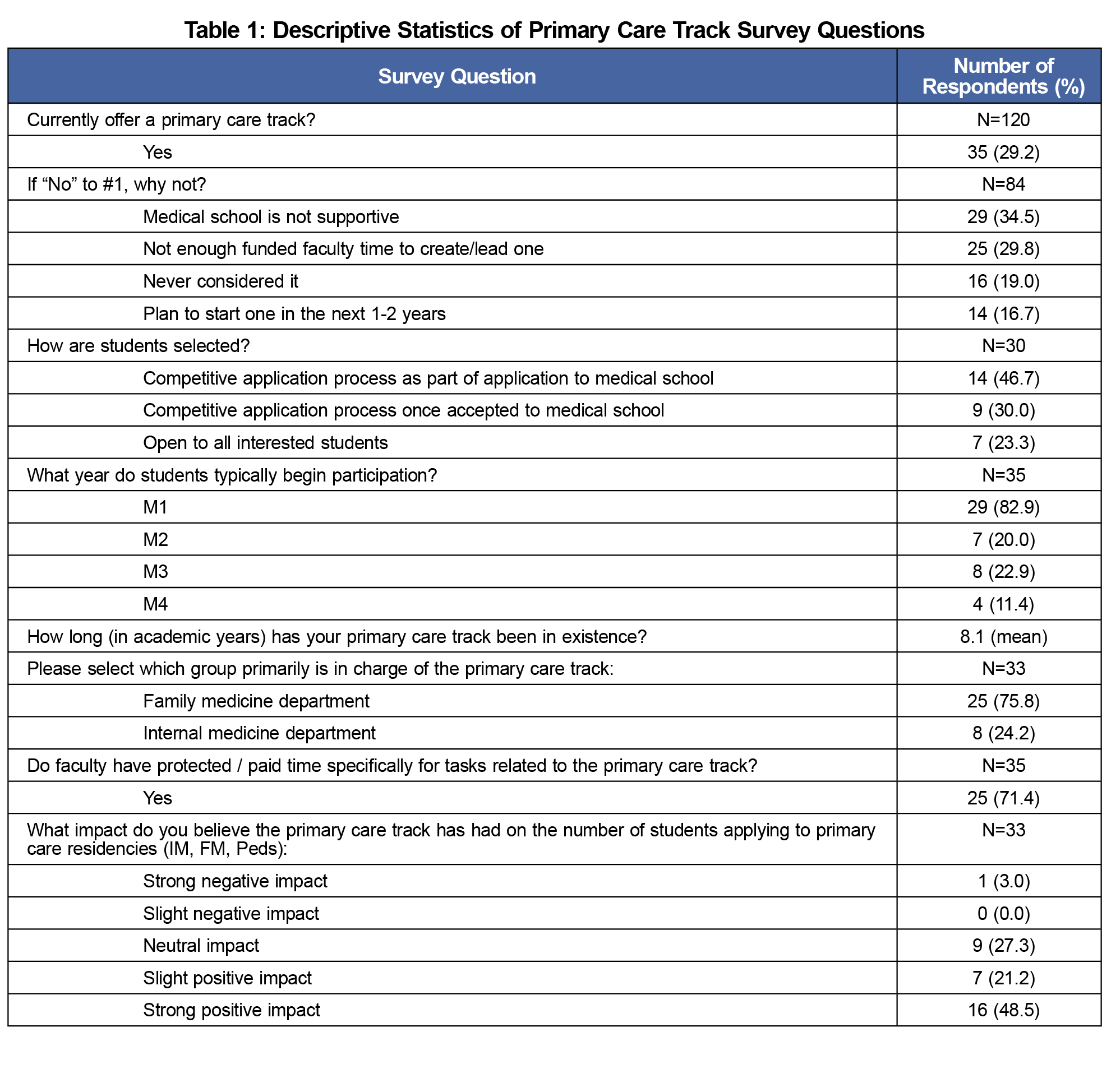
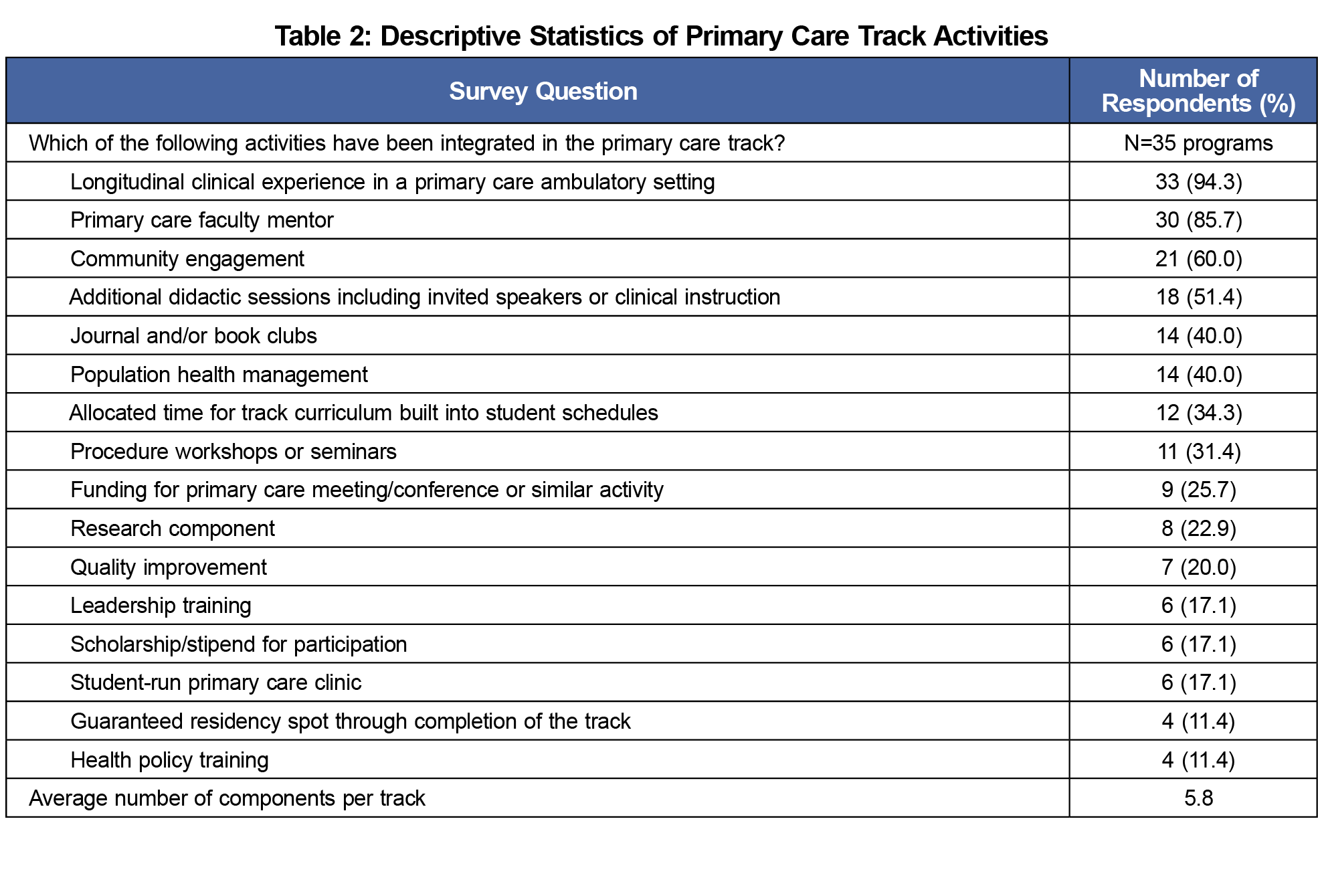
The survey collected basic demographic information about CDs and their medical schools. Survey questions asked about the presence and description of available primary care tracks as well as the CD’s perception of impact (Table 1). Additional questions were based on literature review as well as the research team’s knowledge of activities offered in medical schools (Table 2). A primary care track was defined in the survey as “formal, structured activities that occurred for a period longer than 1 year and were led by an identified faculty member.” We did not further define what activities were considered as primary care.
Statistical Analysis
Descriptive statistics were used to characterize demographic data and longitudinal primary care tracks. Logistic regression was used to investigate associations between schools with primary care tracks and those without across the variety of variables present. The same approach was used to consider associations between programs planning to implement a primary care track in our data. In order to account for the effects of multiple comparison testing on our results, P values were corrected using the false discovery rate approach where appropriate.9 Fisher exact tests were used to test for associations among the subgroup of institutions with a primary care track. Associations between aspects of the track and clerkship directors’ perceptions on the impact of their primary care track on applications to primary care residencies were investigated. Multiple comparison corrections were not applied to this set of tests due to the greater probability of a false negative as a result of a smaller sample size. All analyses were done using R version 3.2.2 statistical program.
The survey was distributed via email to 125 US and 16 Canadian family medicine CDs, with a response rate of 86%. Thirty-five respondents (29%) reported currently offering a longitudinal primary care track (Table 1). The greatest barriers to offering a longitudinal track included lack of medical school support (34%) and funded faculty time (29%). Fourteen schools (16%) planned to offer one in the next 1-2 years (Table 1). There was great variation in activities, but nearly all included a longitudinal primary care ambulatory clinical experience and provided a primary care faculty mentor (Table 2). Community engagement as well as additional didactic sessions were also present in most tracks (Table 2). Almost 70% of CDs felt there was a positive impact on students entering primary care (Table 1). There were no significant differences in characteristics (eg, school region, public or private school, CD gender or ethnicity) between schools with primary care tracks and those without, or between programs planning to implement a primary care track and those that weren’t. Also, CDs’ perceptions of the impact of their program on the number of students applying to primary care programs was not associated with the program offerings (Table 2) or what year students begin their clerkship rotations.
Longitudinal primary care tracks are varied in their characteristics. They are currently offered in about one-third of medical schools with another 10% planned in upcoming years. However, a lack of faculty and/or medical school support were barriers, which may suggest that colleges of medicine are not as supportive of these tracks.
Our study had several limitations. The primary care track impact on students applying to primary care residencies was measured based on the CDs’ perceptions, and such perceptions may be inaccurate. We are unable to determine the actual impact of the track on residency selection. In addition, the survey was only given to CDs in family medicine who may not have been aware of primary care tracks based in other departments. The survey definition of primary care tracks may have been unclear, as we did not clearly state the activities in the structured curriculum should be related to primary care, and some respondents may not have considered other tracks at their institutions as primary care.
Overall this study found that primary care longitudinal tracks are diverse in structure and characteristics, which could allow them to be tailored to meet the missions of individual medical schools. If such tracks have a significant positive impact on students entering primary care and the need for primary care physicians remains at such high levels, a national primary care education organization (eg, Society of Teachers of Family Medicine) should provide a standardized set of criteria or suggestions for such tracks in all medical schools. Additional studies are needed to verify and support this claim.
Acknowledgments
Presentations: Agana DF, Carek P, Harrell J, et al. Primary Care Tracks in Medical Schools: A CERA Survey. Presentation at Society of Teachers of Family Medicine in Washington, DC; May 2018.
References
- Institute of Medicine. Graduate Medical Education That Meets the Nation’s Health Needs. Washington, DC: The National Academies Press; 2014. https://doi.org/10.17226/18754
- Petterson SM, Liaw WR, Phillips RL Jr, Rabin DL, Meyers DS, Bazemore AW. Projecting US primary care physician workforce needs: 2010-2025. Ann Fam Med. 2012;10(6):503-509. https://doi.org/10.1370/afm.1431
- Dupras DM, West CP. Training for Careers in Primary Care: Time for Attention to Culture. J Gen Intern Med. 2015;30(9):1243-1244. https://doi.org/10.1007/s11606-015-3416-1
- Kernan WN, Elnicki DM, Hauer KE. The Selling of Primary Care 2015. J Gen Intern Med. 2015;30(9):1376-1380. https://doi.org/10.1007/s11606-015-3364-9
- Kozakowski SM, Crosley PW, Bentley A. Results of the 2014 National Resident Matching Program®: family medicine. Fam Med. 2014;46(9):701-706.
- Senf JH, Campos-Outcalt D, Kutob R. Factors related to the choice of family medicine: a reassessment and literature review. J Am Board Fam Pract. 2003;16(6):502-512. https://doi.org/10.3122/jabfm.16.6.502
- Pfarrwaller E, Sommer J, Chung C, et al. Impact of Interventions to Increase the Proportion of Medical Students Choosing a Primary Care Career: A Systematic Review. J Gen Intern Med. 2015;30(9):1349-1358. https://doi.org/10.1007/s11606-015-3372-9
- Mainous AG III, Seehusen D, Shokar N. CAFM Educational Research Alliance (CERA) 2011 Residency Director survey: background, methods, and respondent characteristics. Fam Med. 2012;44(10):691-693.
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc B. 1995;57(1):289-300. https://doi.org/10.1111/j.2517-6161.1995.tb02031.x



There are no comments for this article.