Introduction: Student-run free clinics (SRFCs) have become important primary care homes during the COVID-19 pandemic. With students pulled from clinical sites, funding deficits, SRFCs’ voluntary nature, and no best practices for telehealth SRFCs, many have been forced to close. This report shares a systematic approach for implementing a telehealth clinic along with initial outcomes from the Dedicated to Aurora’s Wellness and Needs (DAWN) SRFC.
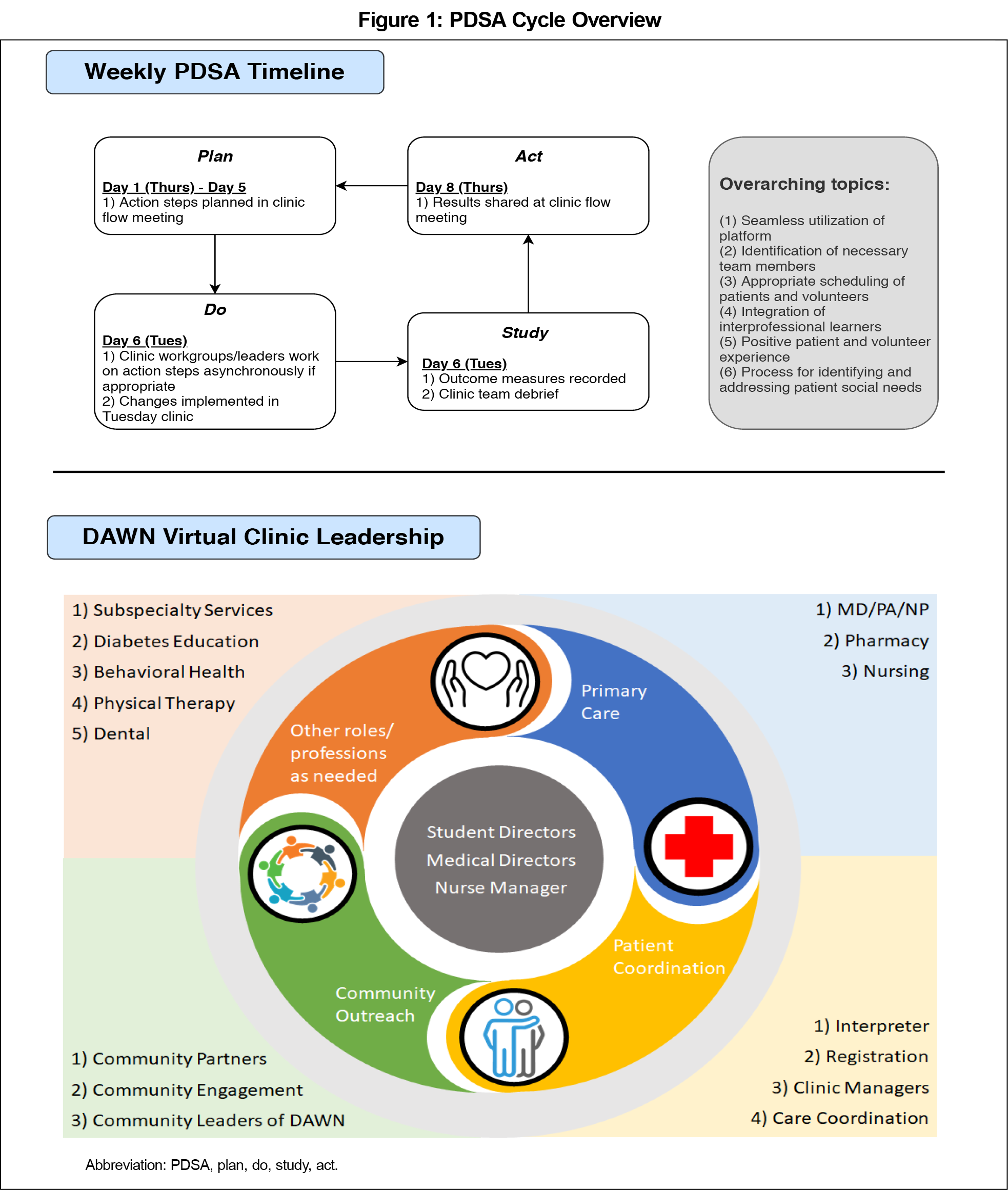
Methods: We utilized pilots with students, community volunteers, and patients to identify a telehealth platform. We implemented weekly plan-do-study-act (PDSA) cycles to develop a feasible interprofessional telehealth model. Key PDSA cycle goals included seamless utilization of platform, identification of necessary team members, appropriate scheduling of patients and volunteers, integration of interprofessional learners, positive patient and volunteer experience, and process for identifying and addressing patient social needs. Measured outcomes included total visits, no-show rates, and chief complaints addressed.
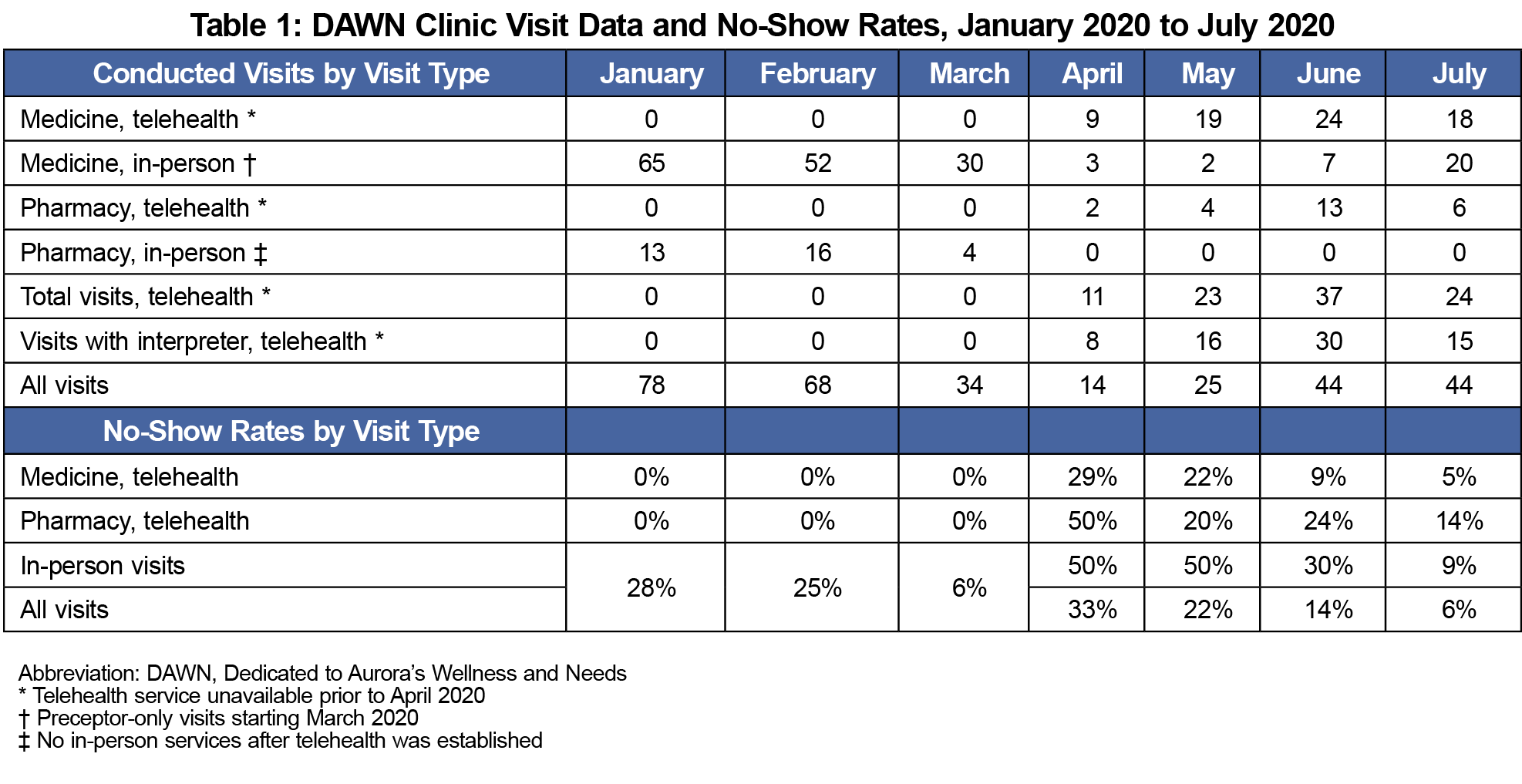
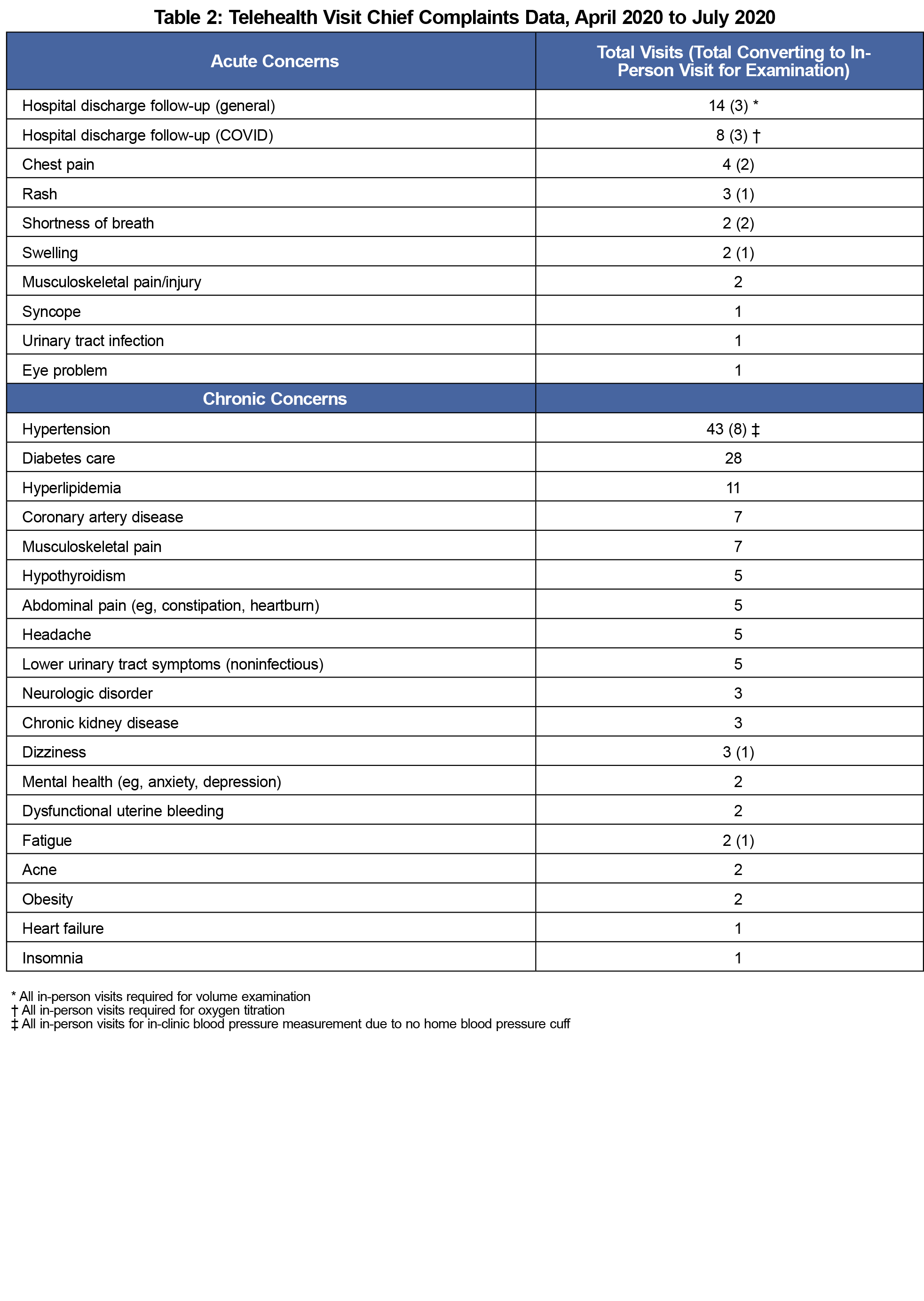
Results: Outcomes from PDSA cycles included a resultant telehealth clinic team and model, workflow for outreach for social needs screening and navigation, and team training guides. Visit data and no-show rates from January 2020 through July 2020 demonstrated total visits returned to 60% of pre-COVID numbers while no-show rates decreased significantly below pre-COVID rates. A range of acute and chronic concerns were successfully managed via telehealth.
Conclusion: SRFCs are poised to continue serving an important role in caring for the country’s most vulnerable populations. The DAWN telehealth implementation process, outcomes, and resultant protocols may help inform other SRFCs seeking to establish telehealth services.
Since March 2020, communities have adopted social distancing policies to limit COVID-19 cases.1 Medical schools nationwide withdrew students from clinical duties and transitioned to remote learning. The pandemic created disproportionate strain on many vulnerable populations by exacerbating inequities in health care access, wealth, and income volatility.2 Student-run free clinics (SRFCs), essential primary care homes to many underserved populations, are present at 75% of Association of American Medical Colleges (AAMC) member institutions with 74% of 2019 medical school graduates participating.3,4 SRFCs were forced to confront concerns of asymptomatic viral transmission and limited protective equipment.
The Dedicated to Aurora’s Wellness and Needs (DAWN) interprofessional SRFC in Aurora, Colorado integrates licensed interprofessional providers with over 500 student volunteers per year from dental, medicine, nurse practitioner, nursing, physician assistant, pharmacy, physical therapy, prehealth, and psychology programs. Forty student volunteers weekly serve uninsured adults of all ages, 45% of whom are male and 55% female. Approximately 70% identify as Hispanic/Latino and 18% as Black/African American. Upon establishing care, 91% do not have a usual source of care and over 50% report their health as poor or fair.
Motivated to ensure patients still had services, DAWN reviewed the literature and found limited examples of how to implement a telehealth SRFC.5-12 In March 2020, displaced DAWN students initiated development of an interprofessional telehealth model and recorded the systematic approach and initial outcomes from implementation to support other SRFCs desiring to initiate telehealth.
This project met the definition of a quality improvement project, thus did not require review by the Colorado Institutional Review Board.
Preparing for Implementation
DAWN student leaders met weekly starting March 11, 2020 to develop an initial telehealth workflow based on literature review and the historical in-person model. Leaders identified and piloted six telehealth options, and then top platforms were piloted with volunteer community members and finally with patients over several clinic sessions before Zoom was selected.13 Telehealth options can be found in the STFM Resource Library.14
Implementation
We utilized a plan-do-study-act (PDSA) framework starting April 7, 2020 for implementing telehealth with goals including seamless utilization of platform, identification of necessary team members, appropriate scheduling of patients and volunteers, integration of interprofessional learners, positive patient and volunteer experience, and process for identifying and addressing patient social needs. We completed weekly PDSA cycles with DAWN Virtual Clinic leadership as shown in Figure 1. We incorporated staged changes according to key PDSA cycle goals over an 8-week period until the model reached relative stability. We obtained short-term outcome measures via manual chart review including total medical and clinical pharmacy visits by month, average no-show rates by month, frequency of chief complaints addressed via telehealth, and reasons for conversion from a telehealth visit to in-person follow-up, if applicable.
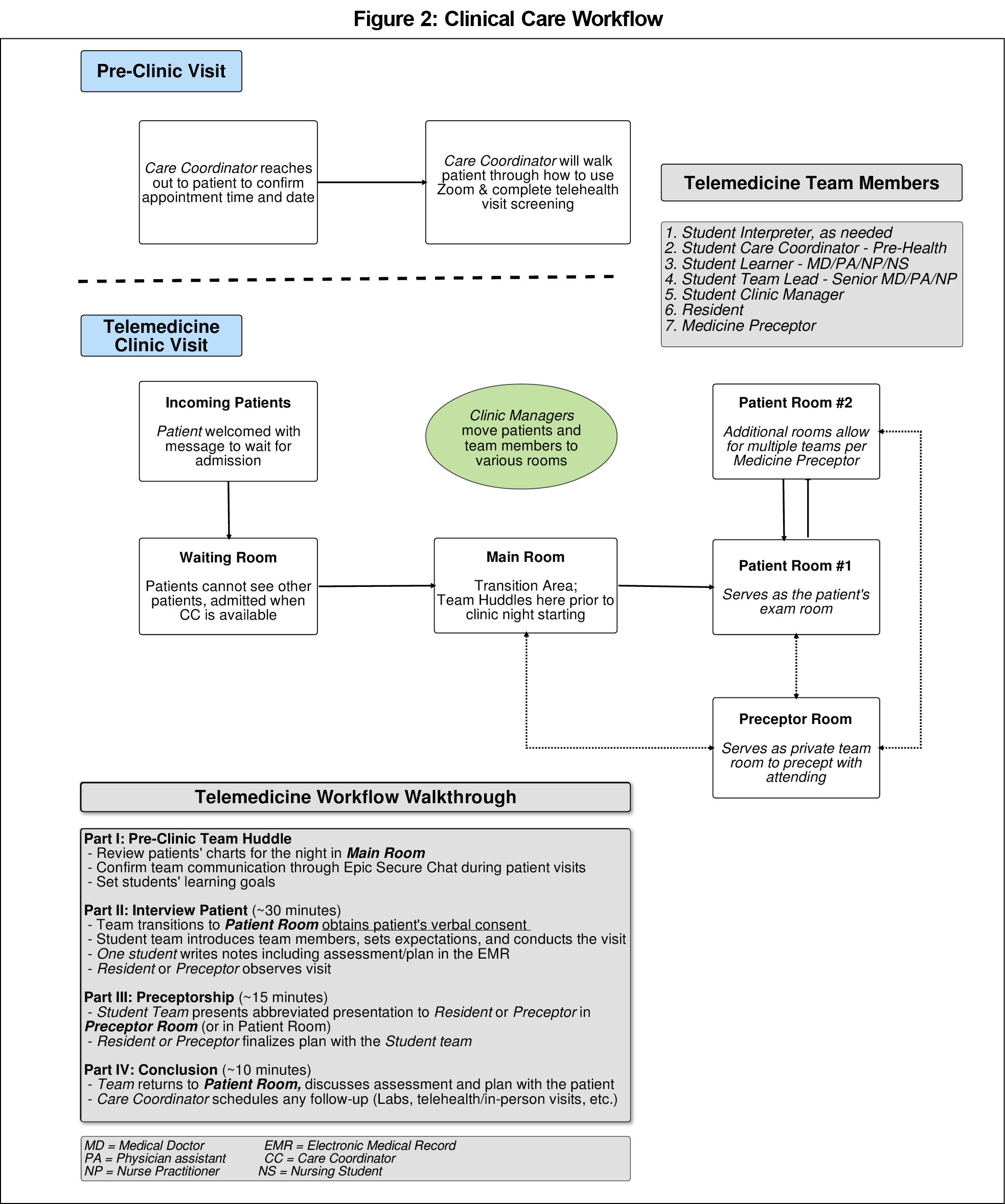
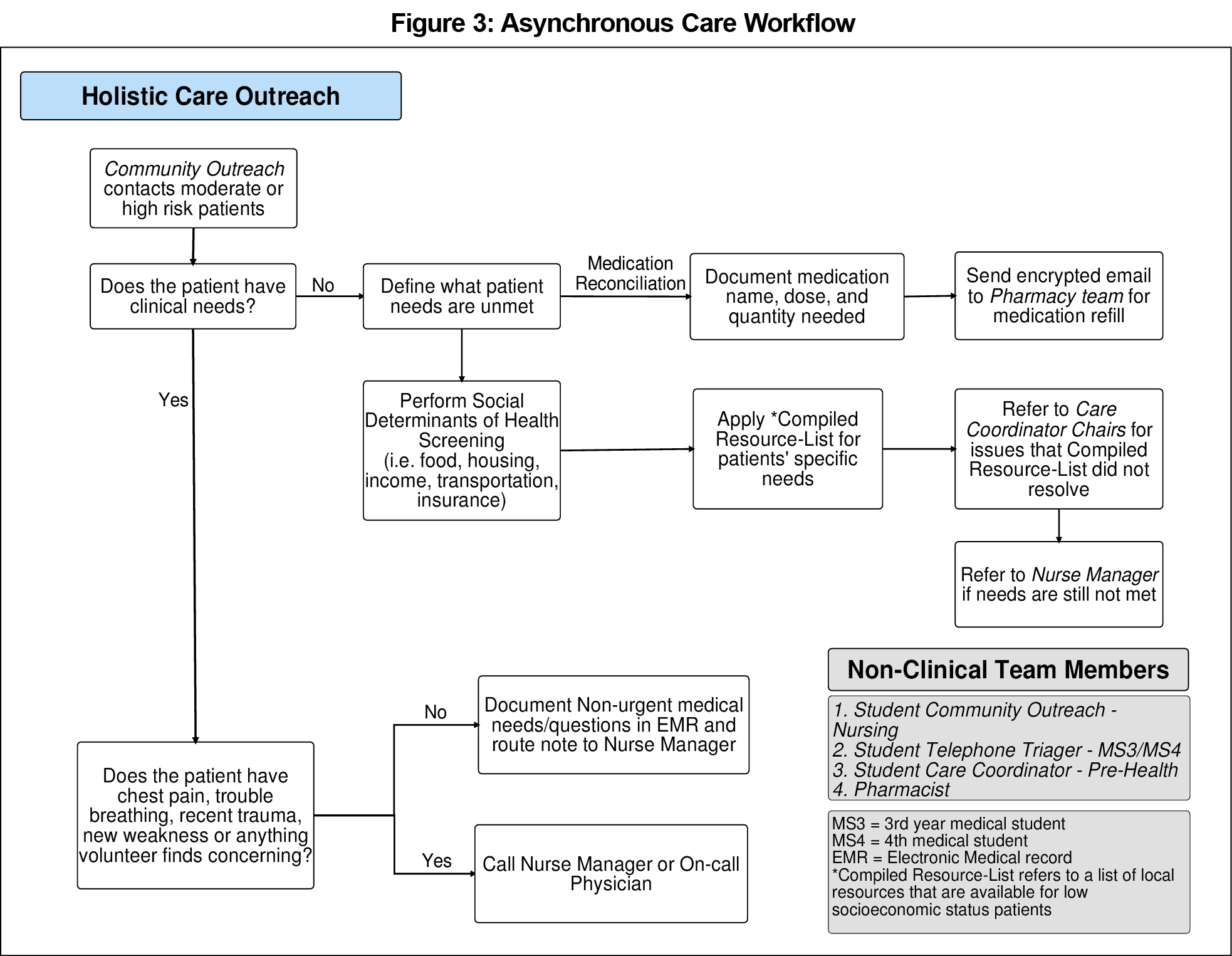
We developed a student telehealth training guide and Zoom instruction guide based on the literature review along with consensus feedback from student leaders. The guides can be found in the STFM Resource Library.15,16 Virtual student medical and clinical pharmacy clinics with continuous PDSA-guided improvements resulted in a near-finalized model by May 2020. See Figure 2 for the resultant volunteer roles, model, and clinic flow. Lastly, the goal to respond to increased patient social needs resulted in the creation of a workflow leveraging student leaders for nonclinical outreach related to social determinants of health (Figure 3).
Visit data and no-show rates from January 2020 through July 2020 are shown in Table 1. Total visits in June and July recovered to 60% capacity of pre-COVID visits in January and February. With the implementation of telehealth at DAWN, no-show rates in June and July decreased significantly from pre-COVID rates. Approximately three-quarters of total telehealth visits were completed via interpreters in six languages—Spanish, Twi, Tigrigna, Nepali, Korean, and Marshallese.
The range of chief complaints addressed via telehealth visits are noted in Table 2. Notably, it was possible for hypertension to be exclusively managed via telehealth if a patient had a home blood pressure cuff. Two acute concerns that required in-person follow-up 100% of the time were patients discharged from the hospital on oxygen and patients requiring a volume examination.
To continue serving the community in the COVID-19 era, SRFCs need immediate telehealth solutions to develop effective models of care. DAWN’s success with integrating telehealth is the result of the tireless work of a large group of clinic leaders over numerous hours. No formal data were gathered to assess patient or volunteer experience. Attendings, residents, and students provided positive feedback regarding clinical care during the pandemic as well as fluidity and rapid improvement of the telehealth model during weekly debriefs. For SRFCs seeking to develop their own telehealth model, it is imperative to have dedicated volunteers able to engage consistently over several months coupled with a standardized process for reflection and improvement.
A notable finding in this review was an improvement in no-show rates to better than pre-COVID rates by the end of the study period. This may reflect the accessibility of telehealth, warm handoffs between team members, or increased follow-up between care coordinators and patients within this new model. One related limitation was that the visit cancellations in the medical record may not have been fully updated in March and April 2020, making the apparent improvement from April through July more impressive than actuality. This effect was minimized through manual review of all visits. Lastly, this report is limited in that it pertains to only one clinic site, has limited short-term outcomes due to data extraction options, and is contextual to the local resources and prior clinic model.
DAWN’s response to complex needs during this unprecedented era is a model with materials and lessons that can be instructive to other settings and communities. Beyond SRFCs, this example shares affordable telehealth solutions for any clinic serving similar populations, and demonstrates how to integrate interprofessional learners into a virtual care setting for the field of medical education.
References
- Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Strong social distancing measures in the United States reduced the COVID-19 growth rate. Health Aff (Millwood). 2020:101377hlthaff202000608. doi:10.1377/hlthaff.2020.00608. [Epub ahead of print].
- Raifman MA, Raifman JR. Disparities in the population at risk of severe illness from COVID-19 by race/ethnicity and income. Am J Prev Med. 2020;59(1):137-139; Epub ahead of print. doi:10.1016/j.amepre.2020.04.003
- Smith S, Thomas R III, Cruz M, Griggs R, Moscato B, Ferrara A. Presence and characteristics of student-run free clinics in medical schools. JAMA. 2014;312(22):2407-2410. doi:10.1001/jama.2014.16066
- Association of American Medical Colleges. Medical School Graduation Questionnaire. Washington, DC: AAMC; 2019. https://www.aamc.org/system/files/2019-08/2019-gq-all-schools-summary-report.pdf. Accessed September 14, 2020.
- Waseh S, Dicker AP. Telemedicine training in undergraduate medical education: mixed-methods review. JMIR Med Educ. 2019;5(1):e12515. doi:10.2196/12515
- van Veen T, Binz S, Muminovic M, et al. Potential of mobile health technology to reduce health disparities in underserved communities. West J Emerg Med. 2019;20(5):799-802. doi:10.5811/westjem.2019.6.41911
- Bramstedt KA, Prang M, Dave S, Shin PN, Savy A, Fatica RA. Telemedicine as an ethics teaching tool for medical students within the nephrology curriculum. Prog Transplant. 2014;24(3):294-297. doi:10.7182/pit2014289
- Goetter EM, Blackburn AM, Bui E, Laifer LM, Simon N. Veterans’ prospective attitudes about mental health treatment using telehealth. J Psychosoc Nurs Ment Health Serv. 2019;57(9):38-43. doi:10.3928/02793695-20190531-02
- Afshari M, Witek NP, Galifianakis NB. Education Research: an experiential outpatient teleneurology curriculum for residents. Neurology. 2019;93(4):170-175. doi:10.1212/WNL.0000000000007848
- Holekamp NM. Moving from clinic to home: what the future holds for ophthalmic telemedicine. Am J Ophthalmol. 2018;187:xxviii-xxxv. doi:10.1016/j.ajo.2017.11.003
- Molleda L, Bahamon M, St George SM, et al. Clinic personnel, facilitator, and parent perspectives of eHealth Familias Unidas in Primary Care. J Pediatr Health Care. 2017;31(3):350-361. doi:10.1016/j.pedhc.2016.11.001
- Kolltveit BH, Gjengedal E, Graue M, Iversen MM, Thorne S, Kirkevold M. Conditions for success in introducing telemedicine in diabetes foot care: a qualitative inquiry. BMC Nurs. 2017;16(1):2. doi:10.1186/s12912-017-0201-y
- Zoom Video. https://zoom.us/. Published 2020. Accessed September 4, 2020.
- Phan RC, Le DV, Nguyen A, Mader K. Student-run free clinics telehealth platform solutions. 2020. STFM Resource Library. https://resourcelibrary.stfm.org/viewdocument/student-run-free-clinic-telehealth-1. Accessed September 14, 2020.
- Phan RC, Le DV, Nguyen A, Mader K. Zoom meeting instructions. 2020. STFM Resource Library. https://resourcelibrary.stfm.org/viewdocument/zoom-meeting-instructions. Accessed September 14, 2020.
- Phan RC, Le DV, Nguyen A, Mader K. DAWN Student-Run Free Clinic Telehealth Student Training Guide. 2020. STFM Resource Library. https://resourcelibrary.stfm.org/viewdocument/dawn-student-run-free-clinic-telehe. Accessed September 14, 2020.



There are no comments for this article.