Background and Objectives: In 2020, approximately 47% of family physicians reported burnout. For physicians, professional burnout is implicated in damage to relationships, increased rates of alcohol and/or substance abuse, depression, and suicide. Professional isolation can be a major contributor to burnout. Organizational interventions targeted at promoting workplace community and collegiality have been effective in decreasing professional isolation. This study sought to decrease professional isolation and promote collegiality among family medicine faculty through an origin storytelling group.
Methods: Family medicine faculty of a residency program in the Midwestern United States were invited to participate in an 8-week origin storytelling group. At the end of the study, individual interviews were offered for participants to reflect on the perceived impact of the process. Additionally, 1 year poststudy, open-ended email responses were invited to assess lasting effects of collegiality.
Results: Fifty percent (12/24) of eligible faculty members participated in the study. Participants who completed one-on-one structured interviews shared their perspectives of the study, which allowed for the importance of the study and next directions to be identified. One-year postcompletion of the study, participants described continued changes they experienced from these groups, via open-ended, email response.
Conclusion: Storytelling groups can provide acceptable, valuable, and easily-implemented contributions to initiatives that enhance physician faculty well-being.
Approximately 42% of physicians report burnout.1 At 47%, family medicine ranks seventh of 30 specialties.1 Burnout encompasses emotional exhaustion, depersonalization, and decreased sense of personal accomplishment. It is associated with impaired clinical care, attrition and turnover of professional staff, and increased health care costs.2-5 Burnout has multiple negative impacts on individuals including damage to relationships, increased rates of alcohol and/or substance abuse, depression, and suicide.6 Professional isolation is a major contributor to burnout.4
Both personal and organizational risk factors have been identified for the three domains of burnout. Organizational interventions targeting excessive workload and stressful clinical environments have successfully reduced burnout scores. Benefits have also been demonstrated from programs to enhance individual coping skills, through programs such as mindfulness-based stress reduction,3,7,9,10 and from small-group activities to promote workplace community, collegiality, and enhance the meaning of work.4,6,8-10 The storytelling small-group activity is a simple way of conveying messages and understanding human complexity, and has been valued by health care workers and has demonstrated increased interpersonal understanding and connection.11,12 We sought to decrease professional isolation and promote collegiality among family medicine faculty through an origin-storytelling group, in which participants reflected, wrote, and shared their personal trajectory to medical academia.
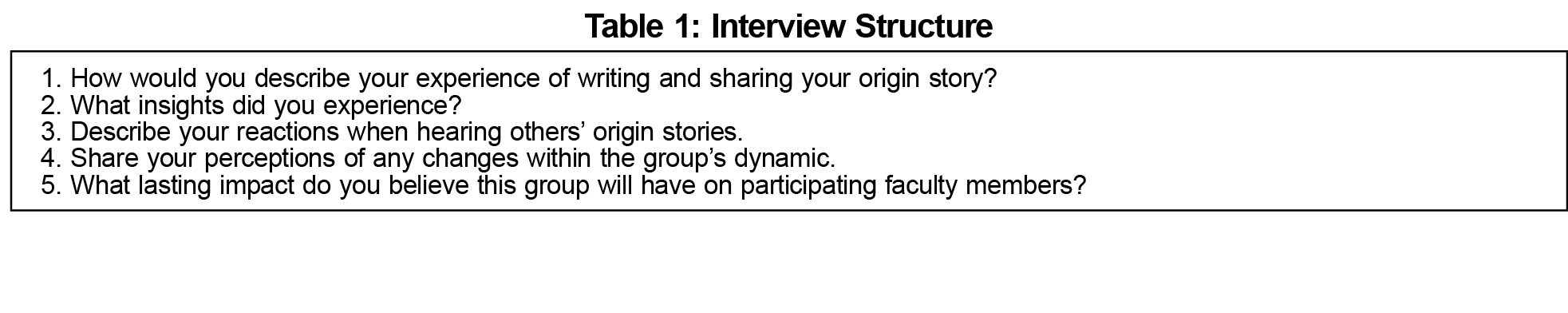
All 24 faculty members were invited to participate in this pilot study via email, announcements during faculty meetings, and through personal communications. Each week, for 8 consecutive weeks, one or two participants reflected on her/his story of origin and prepared a written summary that she/he read in person to the group. Each presentation was followed by discussion involving all participants. At the end of the intervention, participants were also invited to participate in structured individual interviews to reflect on the impact of the intervention (Table 1). Additionally, participants filled out the Mini-Z Burnout Survey prior to and after the storytelling intervention. This survey tool was developed to efficiently measure physician burnout and was of interest to the study team to assess formal workplace burnout.13
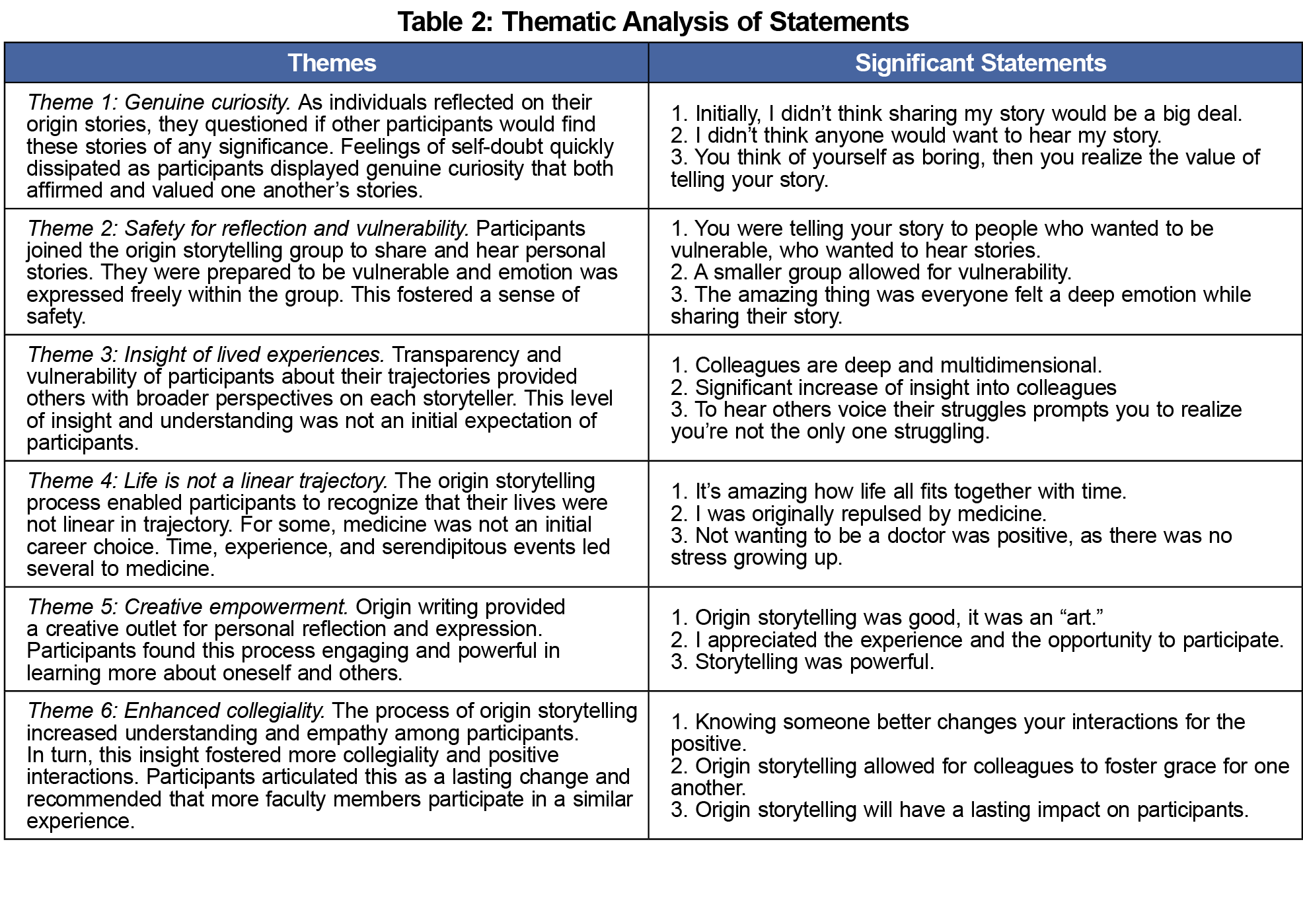
The research team (R.N. and K.N.) completed phenomenological analysis of the recorded interviews. Phenomenological analysis was utilized as it describes the meaning of individuals' lived experience of a phenomenon.14 First, a list of significant statements was developed; similar statements were clustered together into themes. Textural descriptions of what was experienced, structural descriptions of how the experience happened, and composite descriptions incorporating the what and how captured the essence of the experience. Credibility was achieved through prolonged engagement with the group participants, transferability was enhanced by transcription of interviews, dependability was ensured by having two experienced researchers verify the themes, and confirmability was met by the rigor of the note taking and reflection of the process.14 To assess lasting effects on faculty collegiality, participants were asked to describe, via email, any enduring outcomes after 1 year. Prior to implementation, the study was approved by the University of Kansas School of Medicine - Wichita Institutional Review Board.
Twelve (50%) of the full-time faculty members volunteered to participate in the storytelling intervention, which included story writing, storytelling, and discussion. Three (25%) of the 12 participants were male, two (16.7%) were in early career (<5 years), nine (75%) in midcareer (>5 years), and one was in late career (>25 years). African American (8%), Japanese American (8%), Latino (8%), and Euro-Caucasian (76%) ethnicities were represented. There were no measurable changes on the Mini-Z Burnout survey. Despite efforts to involve all participants, only four (30%) interviews were completed due to scheduling challenges. Analysis of the four verbatim transcripts extracted 77 significant statements and identified six themes: (1) genuine curiosity, (2) safety for reflection and vulnerability, (3) insight of lived experience, (4) nonlinear life trajectory, (5) creative empowerment, and (6) enhanced collegiality (Table 2).
One year poststudy, member-checking was completed by inviting all 12 participants to respond, via email, regarding sustained impacts of the intervention. Three of the 12 original participants had relocated, three responded, and the other six did not respond. The three respondents indicated continuing strengthening of relationships among participants as illustrated by the statement “these stories have helped to bridge some of the distances and misconceptions that inevitably arise over time as we work together.”
Despite many competing demands, half of the faculty members volunteered to participate in the storytelling group intervention, indicating perceived value in self-care and support of colleagues as well as acceptability of the intervention. The findings demonstrated that self-reflection to write and share personal stories of origin provide insight into the dynamic interrelated complexities of life. The origin storytelling group provided a safe and comfortable environment in which to listen and express genuine curiosity about one another’s experiences, motivations, and life trajectories. Vulnerability of each participant increased compassion for colleagues and fostered positive interactions. One year following this initiative, feedback identified sustained comfort with interpersonal interactions stimulated by the project. This should provide a positive substrate for proposed initiatives targeting organizational and individual well-being. One such initiative is Balint-type groups for faculty.
To foster a culture of well-being, storytelling initiatives reflect the culture of family medicine in valuing the stories of individual patients and relationships within groups. The resources required are minimal ie, a project champion, designated time and space, and possibly refreshments. Half of our faculty volunteered for this study, but faculty participation may vary depending on individuals’ degree of willingness to reveal personal information and/or respectfully listen, share reflective feedback, and maintain confidentiality.
The generalizability of this study is limited by being conducted in a single residency program, its small sample size, limited diversity of participants, and nonprobability-based sample. A quantitative measure (Mini-Z Burnout Survey)14 was attempted, but there were no statistically significant changes in any component postintervention. This may indicate that the chosen instrument did not measure the impact of the study, or at least did not have an effect size measurable in the sample of 12 participants.
A next step would be to implement similar storytelling groups in several residency programs, including those in other specialties, to determine how outcomes compare within and among different specialties. Outcome measures should be expanded to include aspects of faculty professional vitality and resilience, and potential impact on patient care factors such as teamwork, collegiality, and trust. Enhanced efforts should be made to incorporate long-term follow up of program impact.
The pilot storytelling project enhanced collegiality among faculty physicians that was still evident after 1 year. Although interpersonal relationships improved, no significant reduction was documented in faculty workplace stress scores, possibly due to external factors impacting the residency program. These findings indicate that storytelling groups can provide acceptable, valuable, and easily-implemented contributions to initiatives that enhance physician faculty well-being.
Acknowledgments
Funding Statement: Funding for this study was provided by the Ascension Via Christi Philanthropy Foundation.
Presentations: This study was presented at the following meetings:
- 2020 Society of Teachers of Family Medicine Annual Conference, August 2020 (virtual)
- Collaborative Family Healthcare Association 2020 Annual Conference, October 2020 (virtual)
References
- Kane L. Death by 1000 cuts: Medscape national physician burnout & suicide report 2021: The generational divide. https://www.medscape.com/slideshow/2021-lifestyle-burnout-6013456#2. Published January 15, 2020. Accessed April 28, 2020.
- Shanafelt TD, West CP, Sinsky C, et al. Changes in burnout and satisfaction with work-life integration in physicians and the general US working population between 2011 and 2017. Mayo Clin Proc. 2019;94(9):1681-1694. doi:10.1016/j.mayocp.2018.10.023
- Gregory ST, Menser T, Gregory BT. An organizational intervention to reduce physician burnout. J Healthc Manag. 2018;63(5):338-352. doi:10.1097/JHM-D-16-00037
- Linzer M, Poplau S, Grossman E, et al. A cluster randomized trial of interventions to improve work conditions and clinician burnout in primary care: results from the Healthy Work Place (HWP) study. J Gen Intern Med. 2015;30(8):1105-1111. doi:10.1007/s11606-015-3235-4
- Maslach C. Job burnout. Curr Dir Psychol Sci. 2003;12(5):189-192. doi:10.1111/1467-8721.01258
- Shanafelt TD, Noseworthy JH. Executive leadership and physician well-being: nine organizational strategies to promote engagement and reduce burnout. Mayo Clin Proc. 2017;92(1):129-146. doi:10.1016/j.mayocp.2016.10.004
- Buck K, Williamson M, Ogbeide S, Norberg B. Family physician burnout and resilience: a cross-sectional analysis. Fam Med. 2019;51(8):657-663. doi:10.22454/FamMed.2019.424025
- Aronsson G, Theorell T, Grape T, et al. A systematic review including meta-analysis of work environment and burnout symptoms. BMC Public Health. 2017;17(1):264-277. doi:10.1186/s12889-017-4153-7
- Awa WL, Plaumann M, Walter U. Burnout prevention: a review of intervention programs. Patient Educ Couns. 2010;78(2):184-190. doi:10.1016/j.pec.2009.04.008
- West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018;283(6):516-529. doi:10.1111/joim.12752
- Bruce A, Daudt H, Breiddal S. Can writing and storytelling foster self-care? A qualitative inquiry into facilitated dinners. J Hosp Palliat Nurs. 2018;20(6):554-560. doi:10.1097/NJH.0000000000000478
- Campion-Smith C, Austin H, Criswick S, Dowling B, Francis G. Can sharing stories change practice? A qualitative study of an interprofessional narrative-based palliative care course. J Interprof Care. 2011;25(2):105-111. doi:10.3109/13561820.2010.515427
- Linzer M, Poplau S, Babbott S, et al. Work-life and wellness in academic general internal medicine: results from a national survey. J Gen Intern Med. 2016;31(9):1004-1010. doi:10.1007/s11606-016-3720-4
- Creswell JW. Qualitative Inquiry & Research Design: Choosing Among the Five Approaches. 2nd ed. Thousand Oaks, CA: SAGE Publications; 2013.



There are no comments for this article.