Retrieving evidence-based clinical information is an essential skill for medical professionals. The Liaison Committee on Medical Education emphasized the importance of evidence-based medicine (EBM) in medical curricula when “retrieving and applying evidence” became a Core Entrustable Professional Activity.1 In preclinical medical education, teaching EBM in an integrated and relevant manner remains challenging. The use of a multifaceted approach that includes journal clubs, workshops, or online sessions may be helpful in increasing skills and confidence when teaching EBM.2-4
To enhance our EBM teaching, we created a journal club-based curriculum for a cohort of students. We evaluated effectiveness by measuring changes in students’ knowledge and confidence related to evidence analysis.
Setting
We implemented our EBM Journal Club curriculum (EBMJCC) at Oregon Health & Science University (OHSU), a tertiary center in Portland, Oregon. Students participating in this curricular intervention were part of an 18-month longitudinal preclinical preceptorship.5 Students self-selected into this program, which focused on patient navigation for psychosocially complex primary care patient populations. The EBMJCC transitioned to modified operations and virtual learning during the COVID-19 pandemic. In OHSU’s general EBM curriculum, all preclinical students complete four 90-minute small group sessions over 18 months focusing on EBM principles.
Curriculum and Participants
Eight students participated in the EBMJCC between May 2020 and August 2020, over eight sessions. Sessions were 1 hour long, with the first 20 minutes dedicated to student presentation of a paper focused on specific patient experiences. Students were provided a seven-page Evidence Cycle Summary6 and were encouraged to form clinical questions that would support their work with patients.
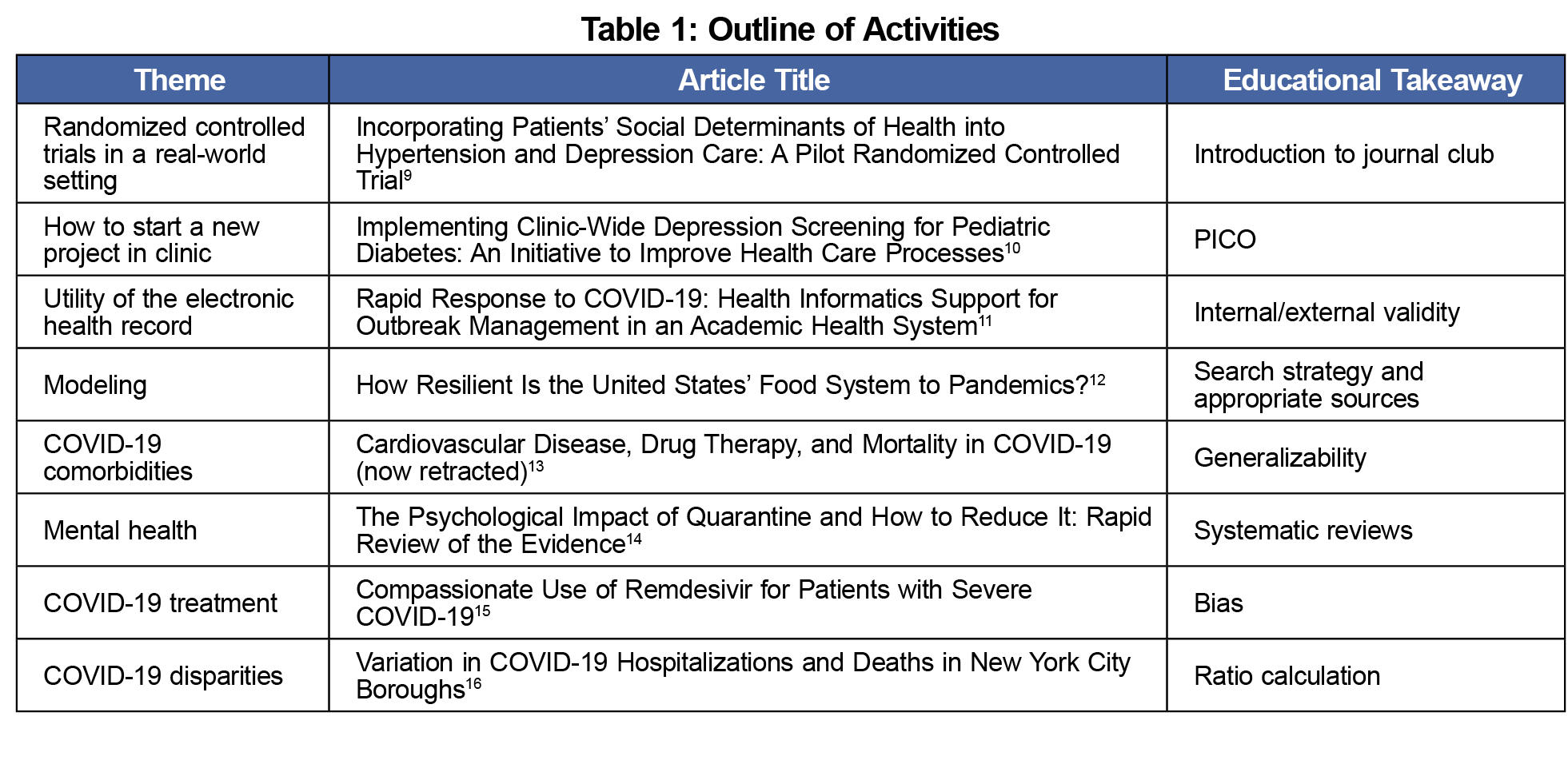
Student graduates of the program facilitated discussion of a preselected article for the remaining time. Selection of articles occurred a few weeks in advance of each session to maximize flexibility in identifying timely, pertinent literature. EBM principles outlined by Duke directed selection of education topics,6 illustrating themes that were salient to EBM or relevant to structural determinants of health (Table 1). A faculty member was also available during the session.
Evaluation
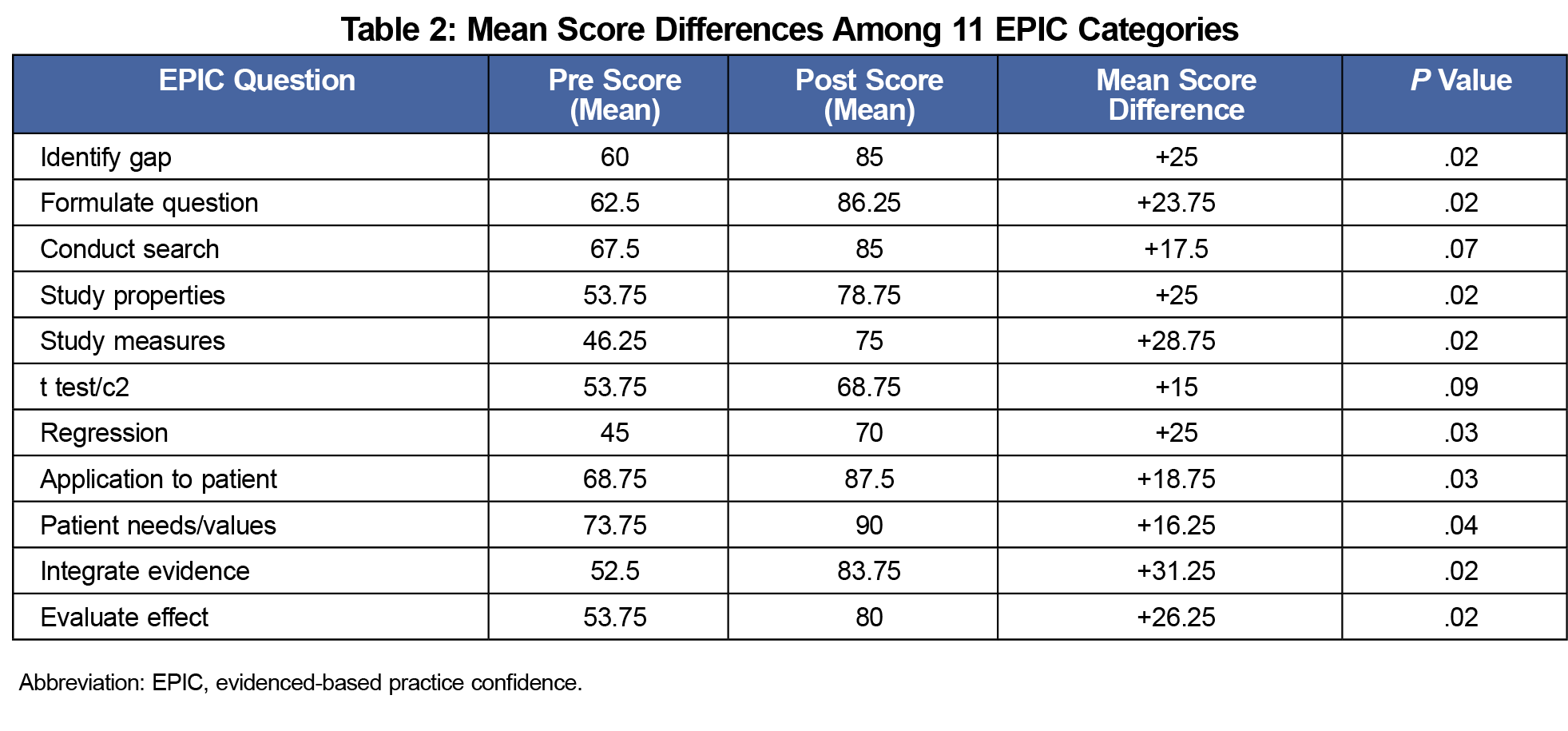
We assessed students’ EBM knowledge and confidence in EBM principles using the Modified Fresno Test (MFT)7 and the Evidenced-Based Practice confidence (EPIC) scale.8 We assessed scores before and after the eight sessions. Survey responses were collected via Qualtrics software (Provo, UT). The MFT assessed knowledge and was scored independently using a standard rubric by two student graduates. Scoring discrepancies were discussed and, if needed, brought to the faculty supervisor for a tie-breaking score. We calculated total scores based on the sum of the seven domains. We averaged and compared pre- and postintervention scores. We assessed confidence using a 10-point Likert scale over the 11 domains of the EPIC scale. We calculated mean scores for each domain for both the pre- and postcurriculum test. Wilcoxon Signed Rank Tests were used to assess statistical significance (P<.05) using SPSS Software (Chicago, IL). OHSU’s Institutional Review Board deemed this educational activity exempt from oversight.
Students’ knowledge and confidence improved following completion of the EBMJCC. Average improvement on the MFT was 18%. Specifically, six of the eight students improved their scores on the MFT, ranging from 2.5% to 75% improvement in overall score (P=.21). Two of the students’ scores decreased by a mean of 11.5 points out of 168 total possible points (-6.8%). Of the EPIC scale’s eleven categories, students showed statistically significant improvements in nine categories (P<.05; Table 2). Two areas of improvement were in formulating research questions and applying knowledge to specific patients.
Our eight-session EBMJCC improved preclinical medical students’ knowledge and confidence in applying EBM principles to primary care patient populations. Students' confidence improved in all categories, and we noted an almost 20% increase in EBM knowledge. Our data support the use of familiar, simple interventions to achieve these gains in a virtual setting. Additionally, our intervention uniquely engages students in learning EBM principles via discussion of recently published literature.
The limitations of our study are its small sample size, the selection bias of our self-selected sample, and the use of pre/postintervention statistics instead of more delayed evaluation. Although a small cohort, the results were promising, and this style of learning was subsequently implemented broadly in the preclinical curriculum.
Our pilot experience demonstrates that a student-facilitated journal club series can be used to effectively teach EBM principles, with meaningful increases in student knowledge and confidence. These skills are critical to their future as medical providers and will provide a foundation for more equitable and evidence-based care.
Acknowledgments
The authors gratefully acknowledge the contribution of the students in this longitudinal cohort, as well as their patients. They also recognize the support from the School of Medicine, the Departments of Internal Medicine and Pediatrics, and clinic leadership and staff, in making this program possible.
References
- Obeso V, Brown D, Aiyer M, et al, eds.; Core EPA Publications and Presentations. Association of American Medical Colleges; 2017. Accessed November 22, 2021. aamc.org/initiatives/coreepas/publicationsandpresentations
- Ahmadi N, McKenzie ME, Maclean A, Brown CJ, Mastracci T, McLeod RS; Evidence-Based Reviews in Surgery Steering Group. Teaching evidence based medicine to surgery residents-is journal club the best format? A systematic review of the literature. J Surg Educ. 2012;69(1):91-100. doi:10.1016/j.jsurg.2011.07.004
- Ilic D, de Voogt A, Oldroyd J. The use of journal clubs to teach evidence-based medicine to health professionals: A systematic review and meta-analysis. J Evid Based Med. 2020;13(1):42-56. doi:10.1111/jebm.12370
- Kyriakoulis K, Patelarou A, Laliotis A, et al. Educational strategies for teaching evidence-based practice to undergraduate health students: systematic review. J Educ Eval Health Prof. 2016;13:34. doi:10.3352/jeehp.2016.13.34
- Hasan R, Caron R, Kim H, et al. The Student Navigator Project (SNaP): Preparing Students Through Longitudinal Learning. Med Sci Educ. 2020;30(2):833-841. doi:10.1007/s40670-020-00957-6
- Tajer, T. Evidence-Based Medicine Guide. 2021. STFM Resource Library. Posted Augsut 12, 2021. Accessed November 22, 2021. https://resourcelibrary.stfm.org/viewdocument/evidence-based-medicine-guide?CommunityKey=2751b51d-483f-45e2-81de-4faced0a290a&tab=librarydocuments
- Ramos KD, Schafer S, Tracz SM. Validation of the Fresno test of competence in evidence based medicine. BMJ. 2003;326(7384):319-321. doi:10.1136/bmj.326.7384.319
- Salbach NM, Jaglal SB. Creation and validation of the evidence-based practice confidence scale for health care professionals. J Eval Clin Pract. 2011;17(4):794-800. doi:10.1111/j.1365-2753.2010.01478.x
- McClintock HF, Bogner HR. Incorporating patients’ social determinants of health into hypertension and depression care: A pilot randomized controlled trial. Community Ment Health J. 2017;53(6):703-710. doi:10.1007/s10597-017-0131-x
- Marker AM, Patton SR, McDonough RJ, Feingold H, Simon L, Clements MA. Implementing clinic-wide depression screening for pediatric diabetes: an initiative to improve healthcare processes. Pediatr Diabetes. 2019;20(7):964-973. doi:10.1111/pedi.12886
- Reeves JJ, Hollandsworth HM, Torriani FJ, et al. Rapid response to COVID-19: health informatics support for outbreak management in an academic health system. J Am Med Inform Assoc. 2020;27(6):853-859. doi:10.1093/jamia/ocaa037
- Huff AG, Beyeler WE, Kelley NS, McNitt JA. How resilient is the United States’ food system to pandemics? J Environ Stud Sci. 2015;5(3):337-347. doi:10.1007/s13412-015-0275-3
- Mehra MR, Desai SS, Kuy S, Henry TD, Patel AN. Cardiovascular disease, drug therapy, and mortality in covid-19. N Engl J Med. 2020;382(25):e102. doi:10.1056/NEJMoa2007621
- Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. SSRN Electronic Journal. 2020;395(10227):912-920. doi:10.2139/ssrn.3532534
- Grein J, Ohmagari N, Shin D, et al. Compassionate use of remdesivir for patients with severe covid-19. N Engl J Med. 2020;382(24):2327-2336. doi:10.1056/NEJMoa2007016
- Wadhera RK, Wadhera P, Gaba P, et al. Variation in covid-19 hospitalizations and deaths across new york city boroughs. JAMA. 2020;323(21):2192-2195. doi:10.1001/jama.2020.7197



There are no comments for this article.