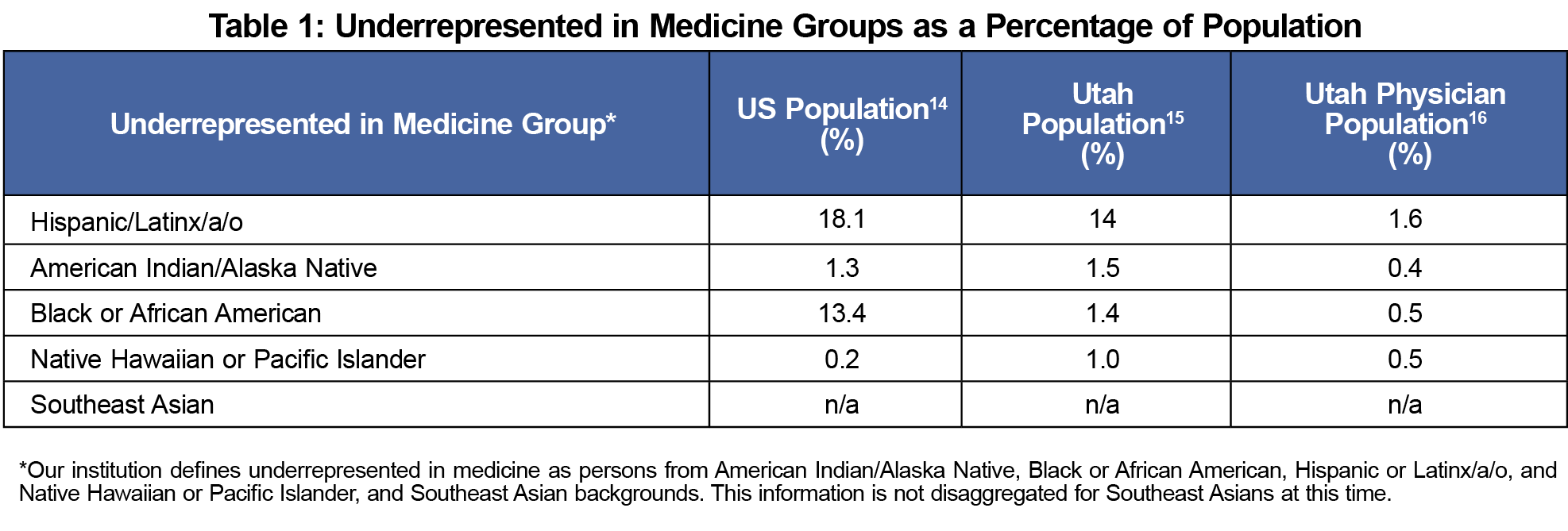
Black, Latinx, American Indian/Alaska Native, Pacific Islander, and Southeast and refugee Asian populations remain underrepresented in medicine (URiM) at levels far below their representation in the general population.1-3 The growing diversity of the US population necessitates increased diversity in family medicine, as patients from URiM communities often prefer physicians who share their cultural background.4 These patients have improved health outcomes when seen by physicians with similar racial/ethnic backgrounds.5-7 Furthermore, URiM family physicians are more likely to serve URiM communities8 and are twice as likely to practice in the inner-city and rural areas.9 Utah and national URiM population percentages are presented in Table 1.
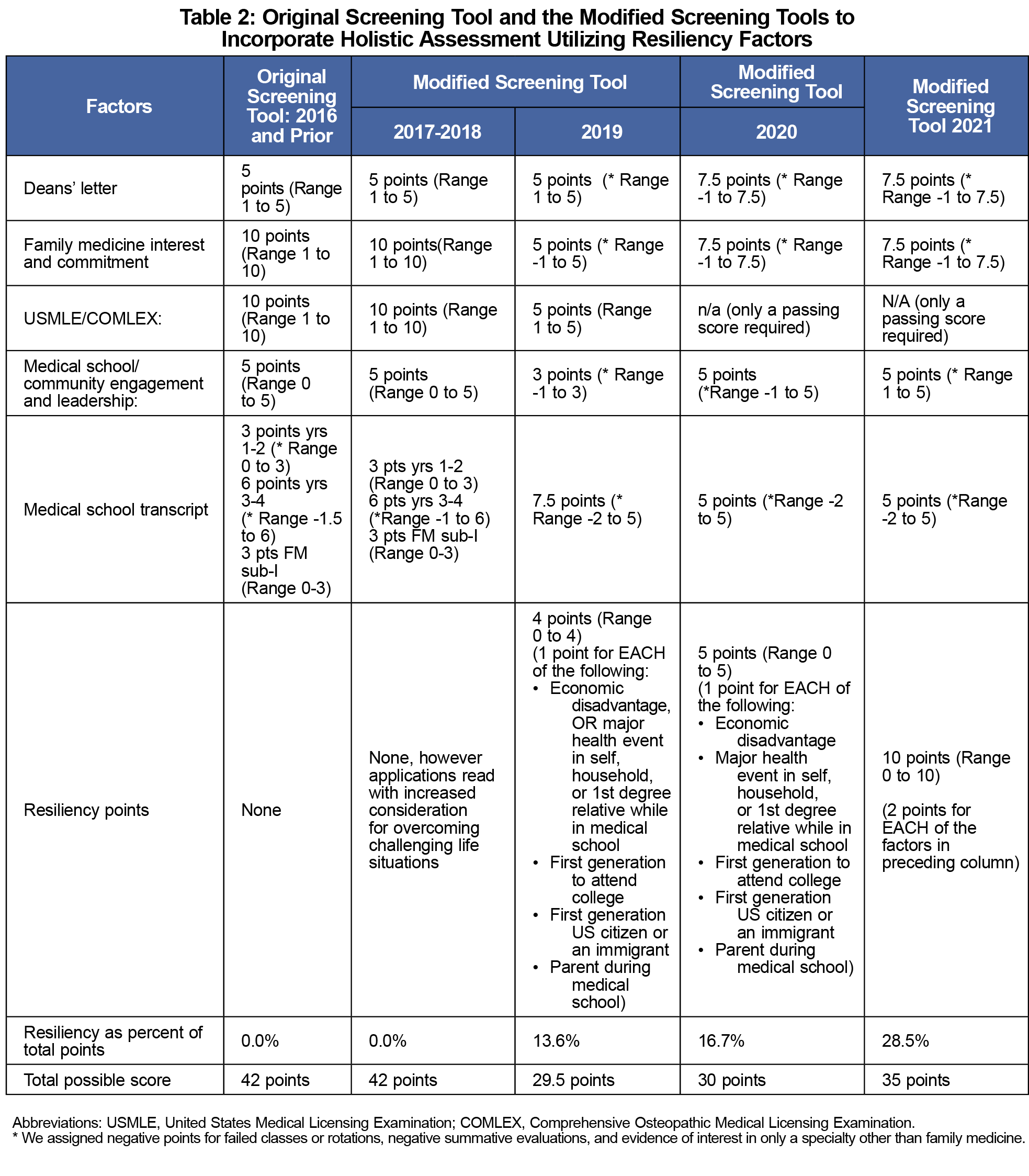
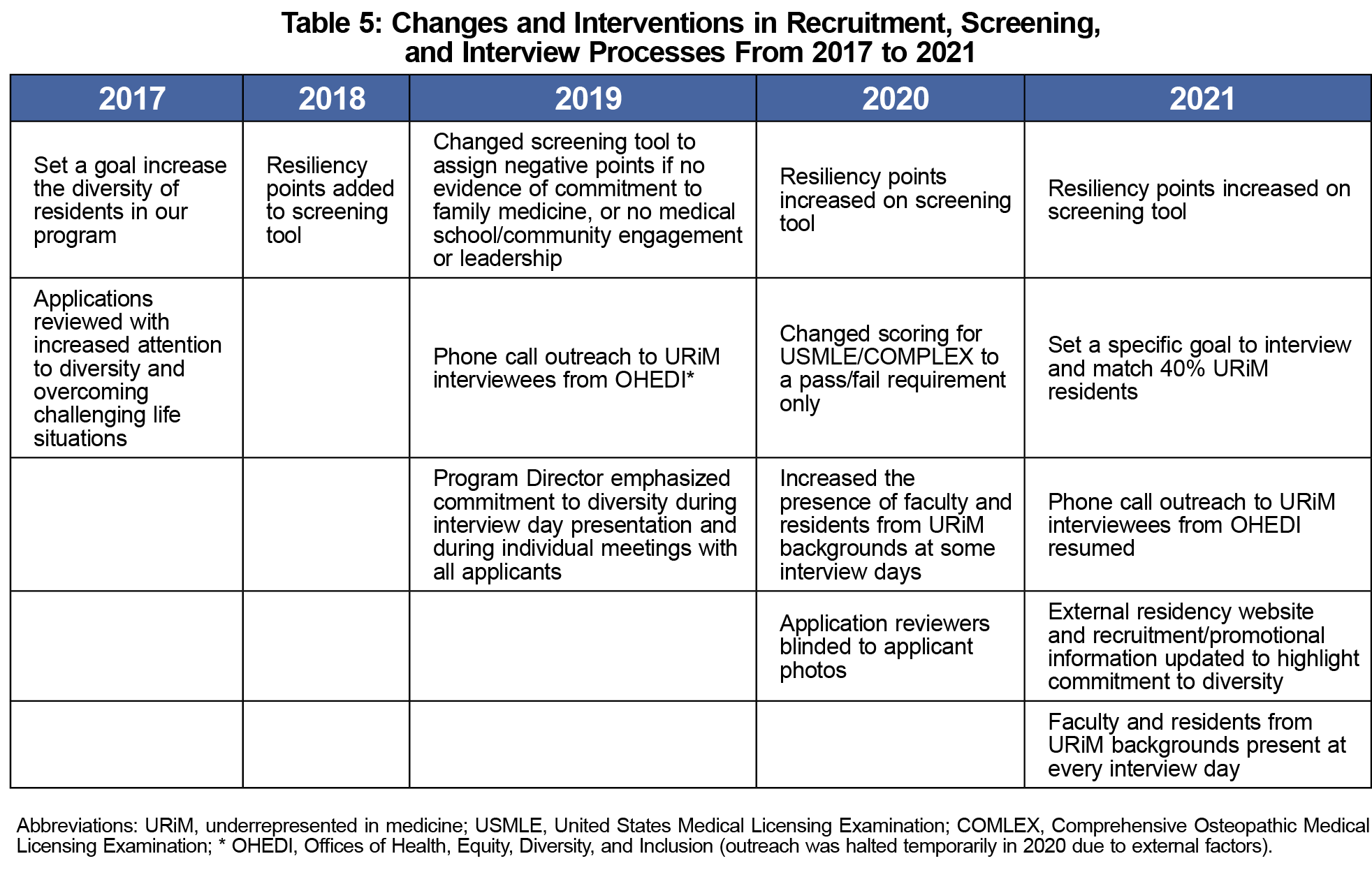
To address the lack of URiM physicians in our state, the University of Utah Family Medicine Residency Program (UUFMRP) set a goal to increase the match rates of URiM applicants into our residency program. From 2010 to 2020, 64.9% of all family medicine graduates have remained in Utah to practice, with 77.8% of UUFMRP graduates remaining here to practice in 2020.10 We felt a systematic change incorporating multiple modalities would be both sustainable and beneficial in our equity, diversity, and inclusion efforts.11,12 We report on a successful iterative improvement process.




There are no comments for this article.