Introduction: With growing efforts to provide comprehensive and inclusive sexual health care, family medicine clerkships are well positioned to educate learners about a spectrum of related topics. This study investigated the current state of sexual health instruction in family medicine clerkships, including specific factors impacting its delivery.
Methods: Questions about sexual health curricula were created and included as part of the 2020 Council of Academic Family Medicine’s Educational Research Alliance survey of family medicine clerkship directors. The survey was distributed via email to 163 recipients between June 1, 2020 and June 25, 2020.
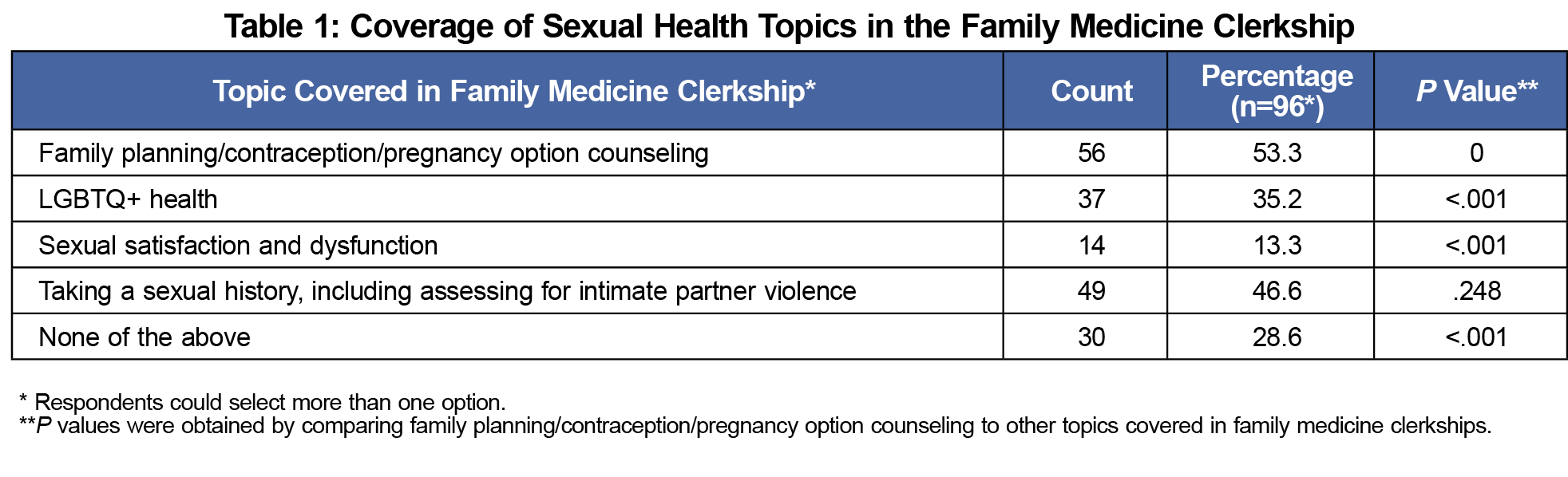
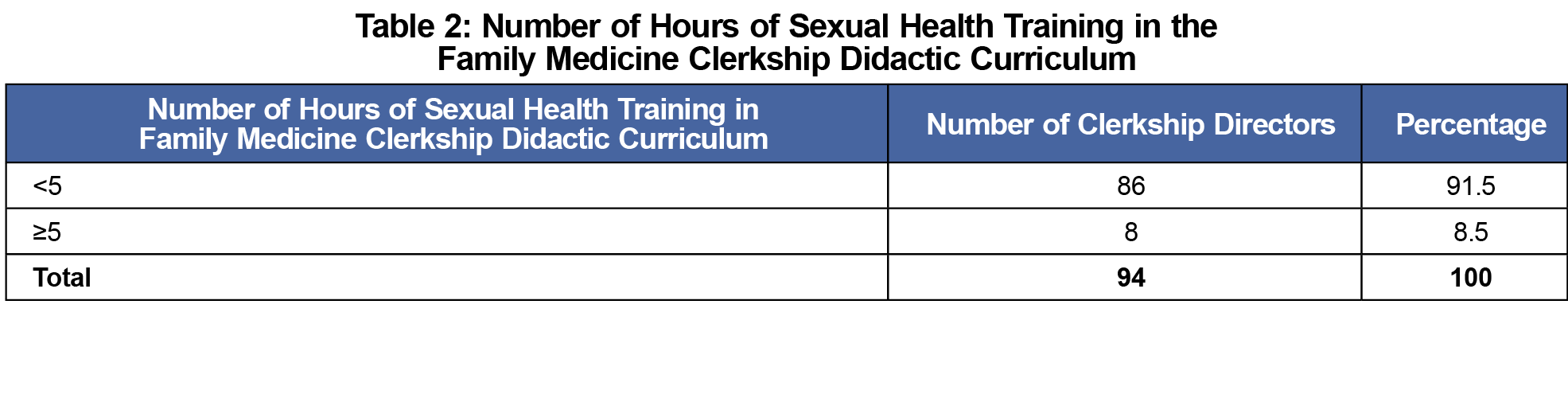
Results: One hundred five (64.42%) of 163 clerkship directors responded to the survey. Our results revealed that during family medicine clerkships, family planning, contraception, and pregnancy options counseling are covered significantly more often than topics related to sexual dysfunction and satisfaction and LGBTQ+ health. Most clerkship directors (91.5%) reported less than 5 hours of sexual health training in their curriculum. Those with more dedicated sexual health curricular hours were more likely to include simulation. Lack of time (41.7%) was the most frequently reported barrier to incorporating sexual health content into the clerkship.
Conclusions: Coverage of sexual health topics during the family medicine clerkship is limited in scope and delivery. To support curricular development and integration, future studies should more thoroughly examine the factors influencing the inclusion of sexual health content in family medicine clerkships as well as the development of assessment methods to determine competency.
In 2014, the Association of American Medical Colleges published 30 professional competencies for medical students and physicians related to LGBTQ+ health.1 In 2017 and 2020, subsequent articles outlined sexual health curricular competencies for undergraduate medical education.2,3 Despite this, previous studies have shown inconsistent and limited education on sexual health in most North American medical schools.4-6
The majority of schools include topics of sexually transmitted infections (STIs), pregnancy, contraception, safe sex, and infertility.6-8 However, sexual health topics such as puberty and decision making, targeting younger (ages 10-14 years) patients, and sexual dysfunction and satisfaction, targeting geriatric populations, are less likely to be covered.6,8 While curricular coverage of LGBTQ+ health issues has increased in recent years, there is opportunity for increased diversity of education regarding sexual and gender minority health.6,7
Challenges to the implementation of a sexual health curriculum in undergraduate medical education include content prioritization within a busy curriculum, insufficient faculty training and subsequent knowledge, and religious influence.9 Additionally, students who reported limited sexual experience and insufficient training in clinical sexuality, were less likely to report feeling comfortable talking to patients about sexual health.10
Despite these challenges, family medicine, as a specialty that emphasizes comprehensive care and the biopsychosocial model, is well positioned to address the need to diversify the sexual health topics covered in medical school curricula.1 In order to better understand the factors influencing sexual health coverage in family medicine clerkships, we investigated the presence, extent, and type of sexual health content delivered as well as the factors influencing this curriculum.
Data were gathered and analyzed as part of the 2020 Council of Academic Family Medicine’s Educational Research Alliance survey of family medicine clerkship directors, which is distributed annually to participating accredited US and Canadian medical schools. In 2020, 147 US and 16 Canadian family medicine or primary care clerkship directors were identified; they all received the survey via SurveyMonkey between June 1, 2020 and June 25, 2020.
We conducted data analysis using R 3.6.1. bivariate analyses for all research questions. We used Cochran’s Q test, post-hoc McNemar test, and Fisher’s exact test to calculate the statistical significance (α=0.05) for all research questions. The American Academy of Family Physicians Institutional Review Board approved the study in May 2020.
A total of 105 of 163 (64.42%) clerkship directors responded to at least some questions on the survey. Our results revealed that family planning, contraception, and pregnancy options counseling are covered significantly more often than sexual satisfaction and dysfunction and LGBTQ+ health (Table 1). The majority of clerkships (86, 91.5%) reported having less than 5 hours of sexual health-related content (Table 2). Of note, 31 (33%) clerkship directors reported no sexual health-related content.
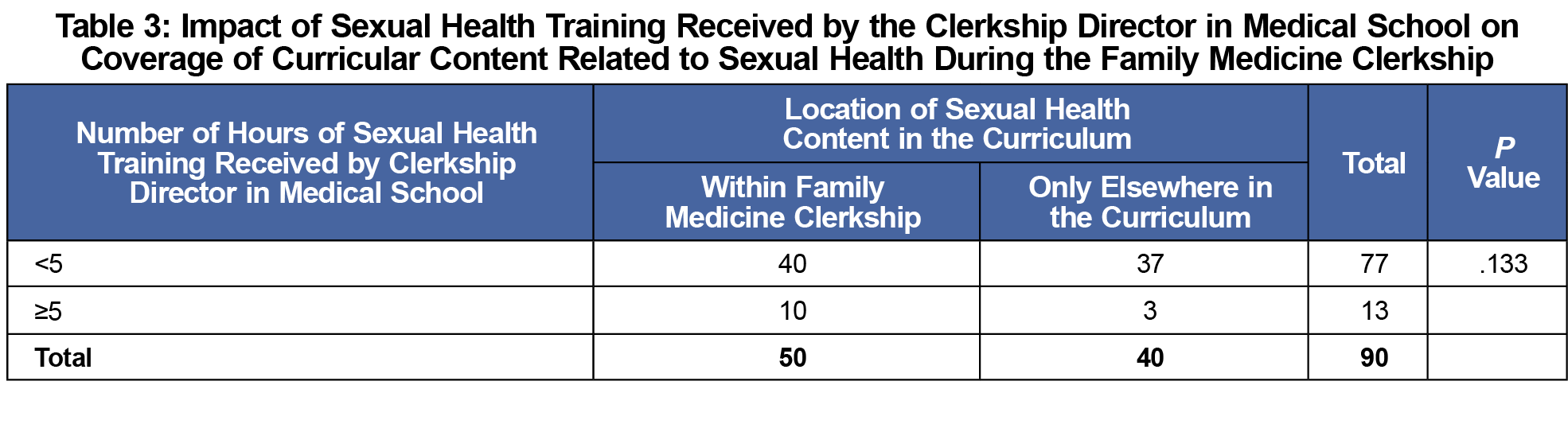
The amount of sexual health training received by clerkship directors during their own medical school training did not significantly influence the inclusion of related curricular content in their clerkship as faculty (Table 3).
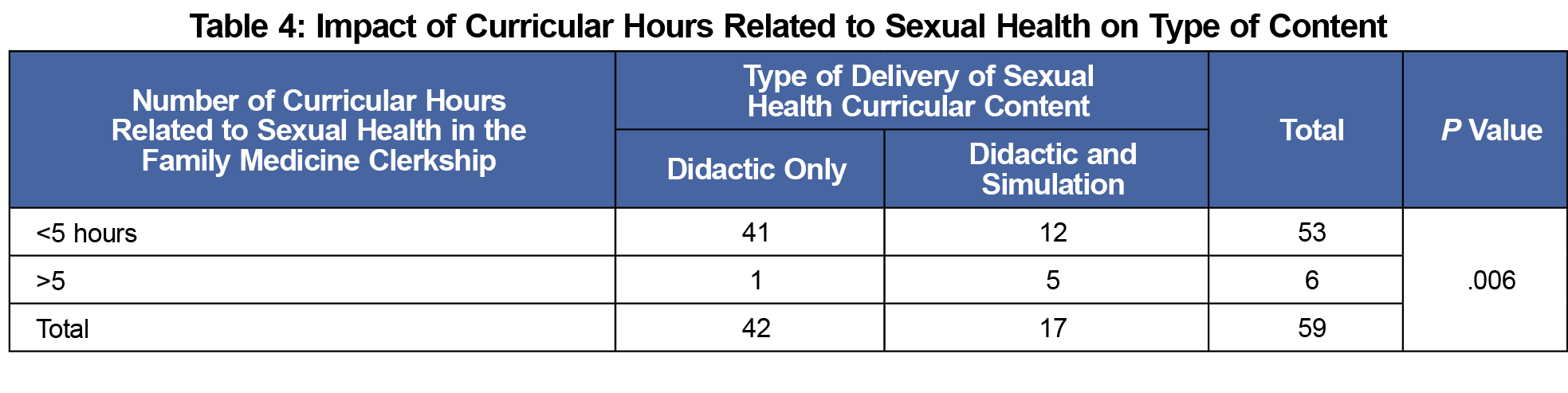
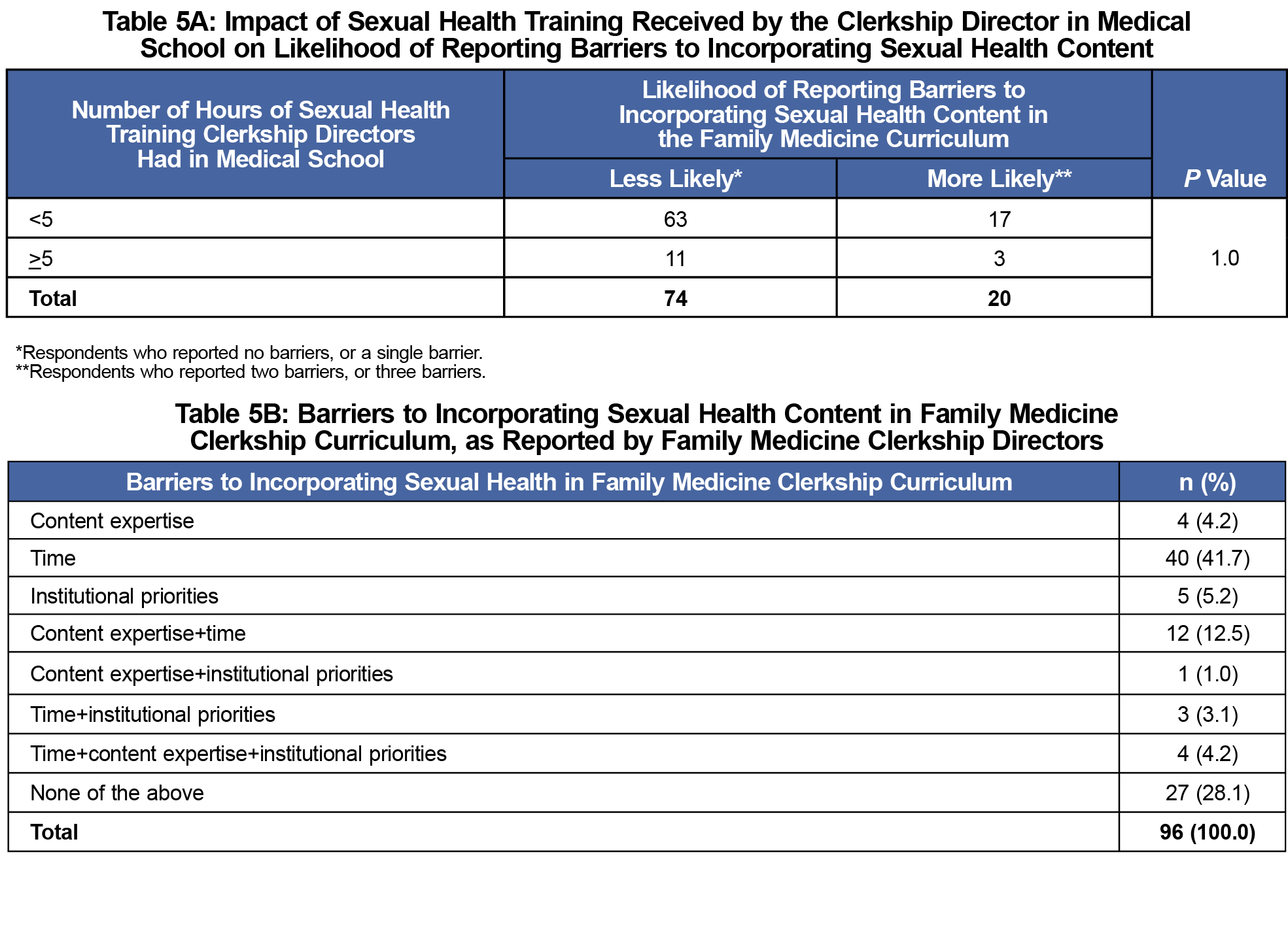
Clerkships with more curricular hours devoted to sexual health topics are more likely to include simulations, such as observed structured clinical examinations (OSCEs,Table 4). Finally, the number of hours of sexual health training received by clerkship directors was not associated with the likelihood of reporting barriers to including sexual health content (Table 5a). However, time was the most commonly reported barrier to including sexual health content in the curriculum (Table 5b).
Similar to previous studies,6-8 our results revealed that contraception, family planning, and pregnancy options counseling are the most frequently covered topics related to sexual health during the family medicine clerkship. However, there was no statistically significant difference between the coverage of these topics compared to taking a sexual history, including screening for intimate partner violence. Sexual dysfunction and LGBTQ+ health topics were covered significantly less frequently, again, consistent with prior studies.6,8 Although 31 schools reported no sexual health curriculum during the family medicine clerkship, it was more likely for clerkships to cover at least one topic.
Our results showed that the amount of sexual health content that clerkship directors received during their own medical school training did not have a significant impact on their likelihood to include sexual health topics during the family medicine clerkship. Based on our results, institutional climate, time constraints, or a lack of resources may have a greater impact on curricular decision-making; with time being the most often reported barrier to including sexual health topics in the curriculum.
Not surprisingly, family medicine clerkships that have less than 5 hours of curricular content related to sexual health are more likely to have only didactic experiences. Other educational methods, such as observed structured clinical experiences, may be limited by time and other required resources. While our questions utilized 5 hours as a benchmark for both the amount of sexual health training received by clerkship directors and the extent of the curriculum in the family medicine clerkship, this number does not necessarily correlate as a marker for competency; we chose 5 hours as the benchmark in our study due to research finding that medical schools have 3-10 hours of sexual health curriculum and an average of 5 hours of LGBTQ+ content.6, 12
An unexpected finding was that approximately 33% of surveyed clerkship directors reported no sexual health content in their clerkship curriculum. This was surprising as sexual health is an essential component of holistic patient care, and multiple related topics are also included in the STFM National Clerkship Curriculum.11 Given that time alone (41.7%) and content expertise and time (12.5%) were the most frequently reported barriers to a sexual health curriculum, the importance of family medicine clerkships prioritizing sexual health-related education and further faculty development regarding sexual health must be emphasized.
There are several limitations to this study. First, clerkship directors with an interest in sexual health may have been more likely to complete the survey, thereby creating possible selection bias. The small sample size limits the power of our analyses and may limit the generalizability of our results. Results may have also been impacted by recall bias, as it is likely difficult to remember the specific content hours received during one’s own medical school training. Additionally, as this was a survey of clerkship directors, it focused on sexual health content during the family medicine clerkship, and these topics may be comprehensively covered in other courses at some institutions. Finally, as STIs are a core topic in the STFM National Clerkship Curriculum,11 we assumed that they are likely to be frequently covered in clerkship curriculum. Due to the limited number of questions permitted for a CERA survey, we prioritized questions on other related topics. As there are numerous sexual health topics, the fact that we assessed the curricular inclusion of just a few is a limitation to this study. Lastly, respondents may have had different definitions of our survey terminology, thereby resulting in variable answers.
While sexual health is an integral part of a patient’s overall well-being and an important part of family medicine, this study found that coverage of these topics during the family medicine clerkship is overall limited in scope and delivery. As family physicians are tasked with using the biopsychosocial model to holistically manage diverse patients, more time should be devoted to covering topics related to sexual health. In particular, family medicine clerkships should work to thoughtfully integrate teaching regarding both sexual satisfaction and dysfunction and LGBTQ+ populations, topics which are currently less likely to be covered by family medicine curriculum; national standards may useful in guiding the creation of this content.1-3 Future studies need to further investigate the factors influencing inclusion of sexual health content in family medicine clerkships and to develop assessment and evaluation strategies to ensure competency in this area.
References
- Implementing Curricular and Institutional Climate Changes to Improve Health Care for Individuals Who Are LGBT, Gender Nonconforming, or Born with DSD: A Resource for Medical Educators. Association of American Medical Colleges. Accessed October 23, 2020. https://store.aamc.org/implementing-curricular-and-institutional-climate-changes-to-improve-health-care-for-individuals-who-are-lgbt-gender-nonconforming-or-born-with-dsd-a-resource-for-medical-educators.html
- Bayer CR, Eckstrand KL, Knudson G, et al. Sexual health competencies for undergraduate medical education in North America. J Sex Med. 2017;14(4):535-540. doi:10.1016/j.jsxm.2017.01.017
- Stumbar SE, Brown DR, Lupi CS. Developing and implementing curricular objectives for sexual health in undergraduate medical education: a practical approach. Acad Med. 2020;95(1):77-82. doi:10.1097/ACM.0000000000002891
- Criniti S, Andelloux M, Woodland MB, Montgomery OC, Hartmann SU. The state of sexual health education in US medicine. Am J Sex Educ. 2014;9(1):65-80. doi:10.1080/15546128.2013.854007
- Malhotra S, Khurshid A, Hendricks KA, Mann JR. Medical school sexual health curriculum and training in the United States. J Natl Med Assoc. 2008;100(9):1097-1106. doi:10.1016/S0027-9684(15)31452-8
- Coleman E, Elders J, Satcher D, et al. Summit on medical school education in sexual health: report of an expert consultation. J Sex Med. 2013;10(4):924-938. doi:10.1111/jsm.12142
- Obedin-Maliver J, Goldsmith ES, Stewart L, et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA. 2011;306(9):971-977. doi:10.1001/jama.2011.1255
- Steinauer J, LaRochelle F, Rowh M, Backus L, Sandahl Y, Foster A. First impressions: what are preclinical medical students in the US and Canada learning about sexual and reproductive health? Contraception. 2009;80(1):74-80. doi:10.1016/j.contraception.2008.12.015
- Zamboni B, Bezek K. Medical Students’ Perceptions and preferences for sexual health education. Sex Educ. 2017;17(4):371-385. doi:10.1080/14681811.2017.1299703
- Shindel AW, Ando KA, Nelson CJ, Breyer BN, Lue TF, Smith JF. Medical student sexuality: how sexual experience and sexuality training impact U.S. and Canadian medical students’ comfort in dealing with patients’ sexuality in clinical practice. Acad Med. 2010;85(8):1321-1330. doi:10.1097/ACM.0b013e3181e6c4a0
- National Clerkship Curriculum-2nd Edition. Society of Teachers of Family Medicine. Published 2018. Accessed 20 May 2021.https://www.stfm.org/media/1828/ncc_2018edition.pdf
- Obedin-Maliver J, Goldsmith ES, Stewart L, et al. Lesbian, gay, bisexual, and transgender-related content in undergraduate medical education. JAMA. 2011;306(9):971-977. doi:10.1001/jama.2011.1255



There are no comments for this article.