Advance care planning (ACP) is a process that enables patients and physicians to define goals and preferences that direct future medical care, as well as identify surrogate decision makers.1 Primary care physicians are uniquely suited to perform ACP due to their longitudinal relationships and patient-centered model of care.2,3 However, ACP is a variable entity that takes many forms and occurs across various settings. There is evidence that many physicians feel unprepared to perform ACP4,5 and that ACP may be underbilled.6,7 For organizations that use billing for ACP as a quality metric, this may have significant ramifications and indicate a need for further education and training on ACP performance, documentation, and billing. We performed a retrospective chart review for patients aged 70 and older in our family medicine resident clinic to evaluate the various ways in which ACP is charted and the gap between billed and non-billed ACP.
RESEARCH LETTER
Actual vs Documented Advance Care Planning in a Primary Care Clinic
Garrett Bowen, MD, MSc | Daria Szkwarko, DO, MPH | Matt Brown, PA-C | Joanne E. Wilkinson, MD, MSc
PRiMER. 2022;6:45.
Published: 12/20/2022 | DOI: 10.22454/PRiMER.2022.495262
Introduction: Advance care planning (ACP) is a complex and multifaceted entity that has significant impact on patient care. ACP takes many forms, may be underbilled, and can have significant ramifications on quality care metrics. We performed a retrospective chart review for patients over 70 years in age in our family medicine resident clinic to evaluate the ways in which ACP is charted and the gap between billed and nonbilled ACP.
Methods: The first 50 patients over 70 years in age seen between August 25, 2020 and September 25, 2020 were selected for standardized chart review. Billing for ACP was defined as Current Procedural Terminology codes=-10 codes 99497 or 99498. Primary outcomes were the percentage of patients with ACP and incidence of ACP documents. Secondary outcome was the proportion of documented ACP conversations in office visits which had billing for ACP.
Results: Forty-eight patients over 70 years in age were identified with an average age of 80.9 years old. Forty-one of 48 patients (85.4%) had some form of ACP and 12 (25%) had formal ACP documents. Of 25 patients with documented ACP conversations in office visits, eleven patients (44%) had ACP which had been formally billed.
Conclusion: The majority of our patients had some form of ACP ranging from inpatient discussions of code status to outpatient visits regarding end-of-life care. However, ACP was underbilled in our practice. Physicians are often evaluated based on quality care metrics such as billed ACP which may not accurately reflect the work physicians are doing.
The project was reviewed and approved by the Care New England Insitutional Review Board. We searched the electronic medical record (EMR) for clinic patients over 70 years old seen between August 25, 2020 and Sepetember 25, 2020. Seventy years was chosen as an arbitrary cutoff age to ensure a population most likely to have undergone ACP. We organized results in order of most recent contact (visit with PCP or associated specialist, telephone call, refill, or any interaction with the hospital system) to exclude patients remote from care. We selected the first 50 patients for chart review. Two patients were excluded due to never being seen in our office. We collected demographic information.
We then reviewed charts for ACP using a standardized template specific to the EMR (Epic). This included reviewing billing, all uploaded documents, all encounters from the past calendar year, a special ACP tab, and searching the chart for use of any of the following terms: “code,” “DNR,” “DNI,” “ACP,” “living,” “life,” “death,” “POA,” “goals,” “end,” “MOLST,” “palliative,” and “hospice.” Billing for ACP was defined as use of CPT codes 99497 or 99498 at any point. All ACP was graded on a binary scale of present or not present. Primary outcomes were the percentage of patients with ACP and incidence of ACP documents. Secondary outcome was the proportion of documented ACP conversations in office visits that had billing for ACP.
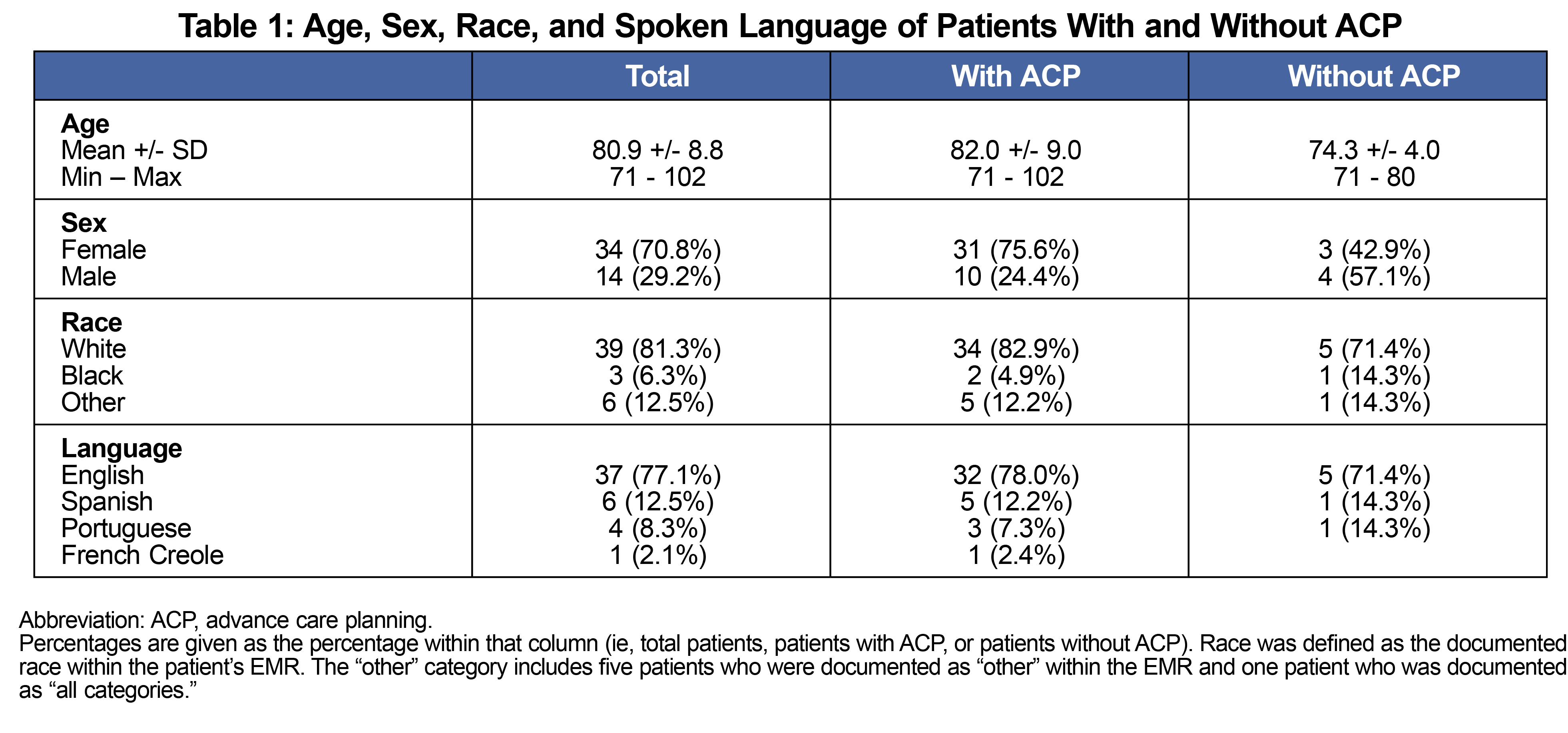
The average patient age was 80.9 years, and the majority were female, White, and English-speaking (Table 1). Documents found included power of attorney (POA, four patients, 8.3%), medical orders for life-sustaining treatment (MOLST, 2, 4.2%), and advanced directives (AD, 6, 12.5%). Twenty-five patients (52.1%) had a discussion regarding ACP in a PCP visit. Thirty-eight (79.2%) had a documented code status. Eleven (22.9%) were billed for ACP.
While the vast majority of patients (85.6%) had some form of ACP on chart review, only 25% of patients had ACP documents (eg, POA, MOLST, or AD) found in the EMR. This is consistent with prior studies which have demonstrated a low rate of signed, legal ACP documents scanned in the EMR.8 Although many of the ACP conversations discussed ACP documents, the majority did not result in signed documents. This may reflect a gap in the ACP process as physicians may not emphasize the importance of returning such documents to the PCP office.
Eleven patients (22.9%) were billed for ACP. This rate of billing compares favorably to nationwide averages showing a peak rate of 5.1% for seriously ill patients9 and is consistent with analysis that shows a higher rate of billing in New England.8 However, there is evidence that ACP was underbilled. Fourteen (29%) patients had documented conversations about ACP without billing. Although the criteria for billing for ACP are stringent,10,11 we suspect that some of these visits met criteria based on the quantity and content of documentation.
That ACP is underbilled is consistent with data showing that ACP billing increases with minor educational interventions6 and has increased steadily since its inception in 2016.12,13 Indeed, one study found that having physicians reflect on a patient’s risk of dying doubled rates of ACP billing.14 The potential underbilling of ACP could have major implications for organizations using billed ACP as a quality care metric and represents an opportunity for further training. Given that many physicians feel unprepared to perform ACP4,5 and the significant inter-provider variation in billing rates,14 training on best ACP practices could significantly improve performance and billing rates.
Limitations of our study include its retrospective, observational nature which limits causal inference. Our population was older, majority White, and English-speaking, limiting generalizability. Moreover, lack of a standardized definition for ACP limits application to clinical practice.
Overall, our review demonstrates the complex, multifaceted nature of ACP. At a time when many are calling into question the utility of ACP,15-18 future research is needed to better define ACP and help organizations apply these definitions in ways that contribute meaningfully to patient care.
Acknowledgments
Financial Support: This project was supported by the Health Resources and Services Administration (HRSA) of the US Department of Health and Human Services (HHS) as part of an award totaling $797,500 with 1% financed with nongovernmental sources. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by HRSA, HHS, or the US Government. For more information, please visit HRSA.gov.
References
- Rietjens JAC, Sudore RL, Connolly M, et al. Definition and recommendations for advance care planning: an international consensus supported by the European Association for Palliative Care. Lancet Oncology.2017(1474-5488 (Electronic)). doi:10.1016/S1470-2045(17)30582-X
- Dhillon K, Jerome D, Teeluck R, Yu Y; On behalf of the Section of Residents. Advance care planning in family medicine training. Can Fam Physician. 2018;64(5):394-396.
- Ahluwalia SC, Harris BJ, Lewis VA, Colla CH. End-of-Life Care Planning in Accountable Care Organizations: Associations with Organizational Characteristics and Capabilities. Health Serv Res. 2018;53(3):1662-1681. doi:10.1111/1475-6773.12720
- Howard M, Bernard C, Klein D, et al. Barriers to and enablers of advance care planning with patients in primary care: survey of health care providers. Can Fam Physician. 2018;64(4):e190-e198.
- Snyder S, Hazelett S Fau - Allen K, Allen K Fau - Radwany S, Radwany S. Physician knowledge, attitude, and experience with advance care planning, palliative care, and hospice: results of a primary care survey. Am J Hosp Palliat Care.2013(1938-2715 (Electronic)).
- Henage CB, McBride JM, Pino J, et al. Educational interventions to improve advance care planning discussions, documentation and billing. Am J Hosp Palliat Care. 2021;38(4):355-360. doi:10.1177/1049909120951088
- Luth EA-O, Manful A, Weissman JS, et al. Practice billing for Medicare advance care planning across the USA. J Gen Intern Med.2022(1525-1497 (Electronic)). doi:10.1007/s11606-022-07404-9
- Wilson CJ, Newman J, Tapper S, Lai S, Cheng PH, Wu FM, Tai-Seale M. Multiple locations of advance care planning documentation in an electronic health record: are they easy to find? J Palliat Med. 2013 Sep;16(9):1089-94. doi: 10.1089/jpm.2012.0472
- Reich AJ, Jin G, Gupta A, Kim D, Lipstiz S, et al. (2020) Utilization of ACP CPT codes among high-need Medicare beneficiaries in 2017: A brief report. PLOS ONE 15(2): e0228553. doi: 10.1371/journal.pone.0228553
- Frequently Asked Questions about Billing the Physician Fee Schedule for Advance Care Planning Services. Centers for Medicare and Medicaid; 2016. Accessed December 12, 2022. https://www.cms.gov/medicare/medicare-fee-for-service-payment/physicianfeesched/downloads/faq-advance-care-planning.pdf
- Kim P, Daly JM, Berry-Stoelzle M, Schmidt M, Levy BT. Use of advance care planning billing codes in a tertiary care center setting. J Am Board Fam Med. 2019;32(6):827-834. doi:10.3122/jabfm.2019.06.190121
- Belanger E, Loomer L, Teno JM, Mitchell SL, Adhikari D, Gozalo PL. Early utilization patterns of the new Medicare procedure codes for advance care planning. JAMA Intern Med. 2019;179(6):829-830. doi:10.1001/jamainternmed.2018.8615
- Grant M. Use of Billing Codes for Advance Care Planning Exceeds Projections. The Coalition to Transform Advanced Care; 2017. Accessed December 12, 2022. https://www.thectac.org/2017/08/use-billing-codes-advance-care-planning-exceeds-projections/
- Barnato AE, O'Malley AJ, Skinner JS, Birkmeyer JD. Use of Advance Care Planning Billing Codes for Hospitalized Older Adults at High Risk of Dying: A National Observational Study. J Hosp Med. 2019 Apr;14(4):229-231. doi: 10.12788/jhm.3150.
- Morrison RS, Meier DE, Arnold RM. What’s wrong with advance care planning? JAMA. 2021;326(16):1575-1576. doi:10.1001/jama.2021.16430
- Korfage IJ, Carreras G, Arnfeldt Christensen CM, et al. Advance care planning in patients with advanced cancer: A 6-country, cluster-randomised clinical trial. PLoS Med. 2020 Nov 13;17(11):e1003422. doi: 10.1371/journal.pmed.1003422.
- Mitchell SL, Volandes AE, Gutman R, et al. Advance care planning video intervention among long-stay nursing home residents: a pragmatic cluster randomized clinical trial. JAMA Intern Med. 2020;180(8):1070-1078. doi:10.1001/jamainternmed.2020.2366
- McMahan RD, Tellez I, Sudore RL. Deconstructing the Complexities of Advance Care Planning Outcomes: What Do We Know and Where Do We Go? A Scoping Review. J Am Geriatr Soc. 2021 Jan;69(1):234-244. doi: 10.1111/jgs.16801
Lead Author
Garrett Bowen, MD, MSc
Affiliations: Warren Alpert Medical School of Brown University, Department of Family Medicine Residency, Pawtucket, RI
Co-Authors
Daria Szkwarko, DO, MPH - Warren Alpert Medical School of Brown University, Department of Family Medicine Residency, Pawtucket, RI
Matt Brown, PA-C - Warren Alpert Medical School of Brown University, Department of Family Medicine Residency, Pawtucket, RI
Joanne E. Wilkinson, MD, MSc - Warren Alpert Medical School of Brown University, Department of Family Medicine Residency, Pawtucket, RI
Corresponding Author
Garrett Bowen, MD, MSc
Correspondence: 111 Brewster St, Pawtucket, RI 02909. 401-729-2304. 401-921-6961
Email: garrett_bowen@brown.edu
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.