Introduction: The needs of medically-underserved populations (MUPs) are consistently outpacing the number of physicians caring for them. Medical students’ motivations toward working with MUPs consistently decline as they progress through medical school. Given the shortage of doctors caring for MUPs, the objective of our study was to further investigate factors that influence medical students’ motivation to work with MUPs while they progress through their education. By identifying these elements, we hope to recommend identified factors within medical education that support the development of more physicians who care for MUPs.
Methods: This cross-sectional study is an assessment of medical students at the University of Texas at Southwestern Medical School (UTSW). The study utilized the Medical Student Attitudes Toward the Underserved (MSATU), a validated survey that assesses medical student motivations toward the provision of medical care to MUPs. Surveys were administered at three time points selected to represent key transition points in medical education.
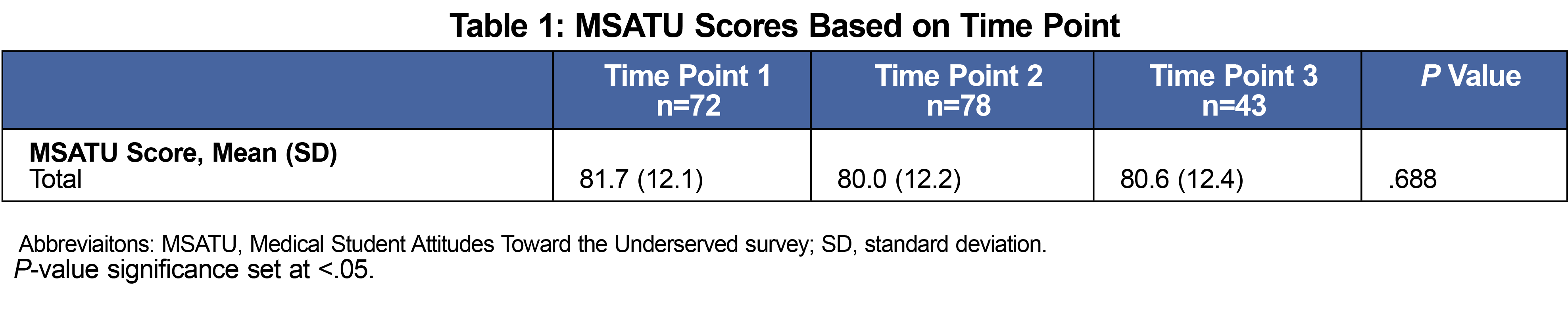
Results: There was no significant difference between MSATU scores among the three time points. MSATU scores were higher among students who identified as female, had higher empathy, had higher value placed on teamwork, and had higher community-centeredness. MSATU scores were also higher among students planning to specialize in primary care compared to students planning to specialize in a non-primary care field (P=.239).
Conclusion: This study identifies factors associated with high MSATU scores within UTSW medical education, including female identification, higher empathy score, higher emphasis on teamwork, higher community-centeredness, and plans to practice primary care. Additionally, the results support maintenance of MSATU scores across all three time points. Future research should examine individual-level data to determine whether individual students are maintaining their MSATU scores or if individual fluctuations are neutralized by group changes.
The needs of medically-underserved populations (MUPs) are consistently outpacing the number of physicians caring for them.1 Given the shortage of doctors caring for MUPs and the complexities associated with caring for these populations, it is vital to identify and address protective factors affecting medical students’ attitudes toward working with MUPs. In this study, we define protective factors as experiences and characteristics that correlate with higher and more stable medical students’ motivations to work with MUPs.
A 2021 systematic review demonstrates that medical students’ motivations toward working with MUPs consistently decline as they progress through medical school.2,3 Other studies show that protective factors like global health experiences,4 community health electives,5 and female gender2,6,7,8,9 act to buffer decreasing medical student attitudes toward working with MUPs.
The aim of our study was to investigate if certain experiences and personal characteristics (including empathy, community-centeredness, and prioritization of teamwork) act as protective factors to bolster medical student’s motivations to work with MUPs as they progress through their education. We hope to recommend implementation of and support for protective factors within medical education to assist the development of more physicians who care for MUPs.
This cross-sectional study was an assessment of medical students at the University of Texas at Southwestern Medical School (UTSW). The study utilized the Medical Student Attitudes Toward the Underserved (MSATU), a validated survey that assesses medical student motivations towards the provision of medical care to MUPs. We also used the Interpersonal Reactivity Index (IRI) that scores empathy, and the Interprofessional Attitudes Survey (IPAS) that measures community-centeredness and teamwork emphasis to quantify characteristics intuitively and historically associated with MUP-focused activities.2,10,11 In the final survey, the MSATU was used in its entirety, select Interprofessional Attitudes Scale (IPAS) subscales were included that can be independently validated, and a previously established modified version of the IRI was used. Participants were also asked about demographics, experiential learning activities, self-reported grades, and anticipated career choices. Career choices were subdivided into primary care (family medicine, internal medicine, pediatrics, internal medicine/pediatrics, obstetrics and gynecology) and non-primary care specialties (all others). The master survey is available on the STFM Resource Library.12
Surveys were administered to UTSW first-year medical students beginning medical school (time point 1), second-year medical students completing preclinical studies (time point 2), and fourth-year medical students before graduation (time point 3). We selected each time point to represent a key transition point in medical education. A REDCap survey link was emailed to each class with a 2-month completion window. Participation was voluntary, and results were anonymized. An incentive of a $10 gift card was provided to students who completed the survey. This study was approved by the UTSW Institutional Review Board.
The outcome variable of interest in this study was the MSTAU total scores. We computed subscales of the IPAS measuring teamwork and community centeredness by using the total sum responses for these items in the IPAS. We computed IRI measurement of empathy was computed by summing eight items from the two subscales of Perspective Taking and Empathic Concern from the IRI. We performed Pearson correlations, two-tailed independent t tests, and analyses of variance to test the main research questions for this study. We set significance at P<.05.
Response rates for the three time points were 30.6%, 33.2%, and 18.6%, respectively. There was no significant difference between MSATU scores among the three time points (Table 1). Regarding demographics, 62.4% of respondents identified as female, 36.0% identified as male, 1.1% preferred to self-describe, and 0.5% preferred not to identify a gender. In terms of ethnicity, 14.5% of participants identified as Hispanic, Latino, or Spanish origin. The racial demographics of participants were 53.0% White or Caucasian, 5.4% African American, 42.2% Asian or Pacific Islander, 1.1% American Indian or Alaskan Native, and 3.8% other.
MSATU scores were higher among females compared to males (t [2, 110]=4.38, P<.001) and among students who did not do a research project with a faculty member compared to those who did (t [2, 133]=2.45, P=.015).
MSATU scores were higher among students who reported planning to care primarily for an underserved population in comparison to those who were undecided and to those who reported no plans to care for a primarily underserved population. (85.9 vs 79.1 vs 70.1; P<.001, Bonferroni test).
MSATU scores were higher among students planning to specialize in primary care compared to students planning to specialize in a non-primary care field (r [1, 178]=.239, P<.001).
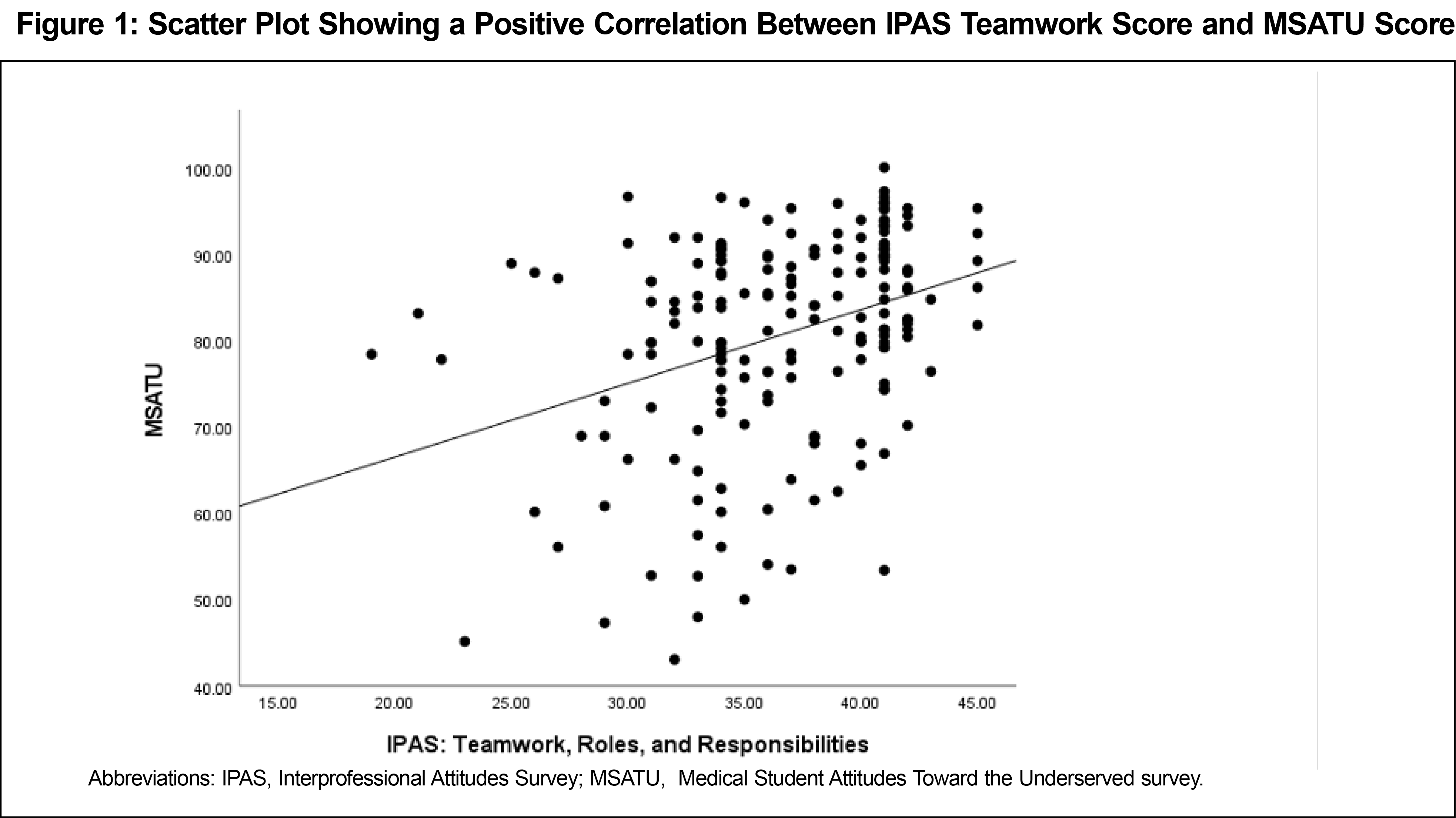
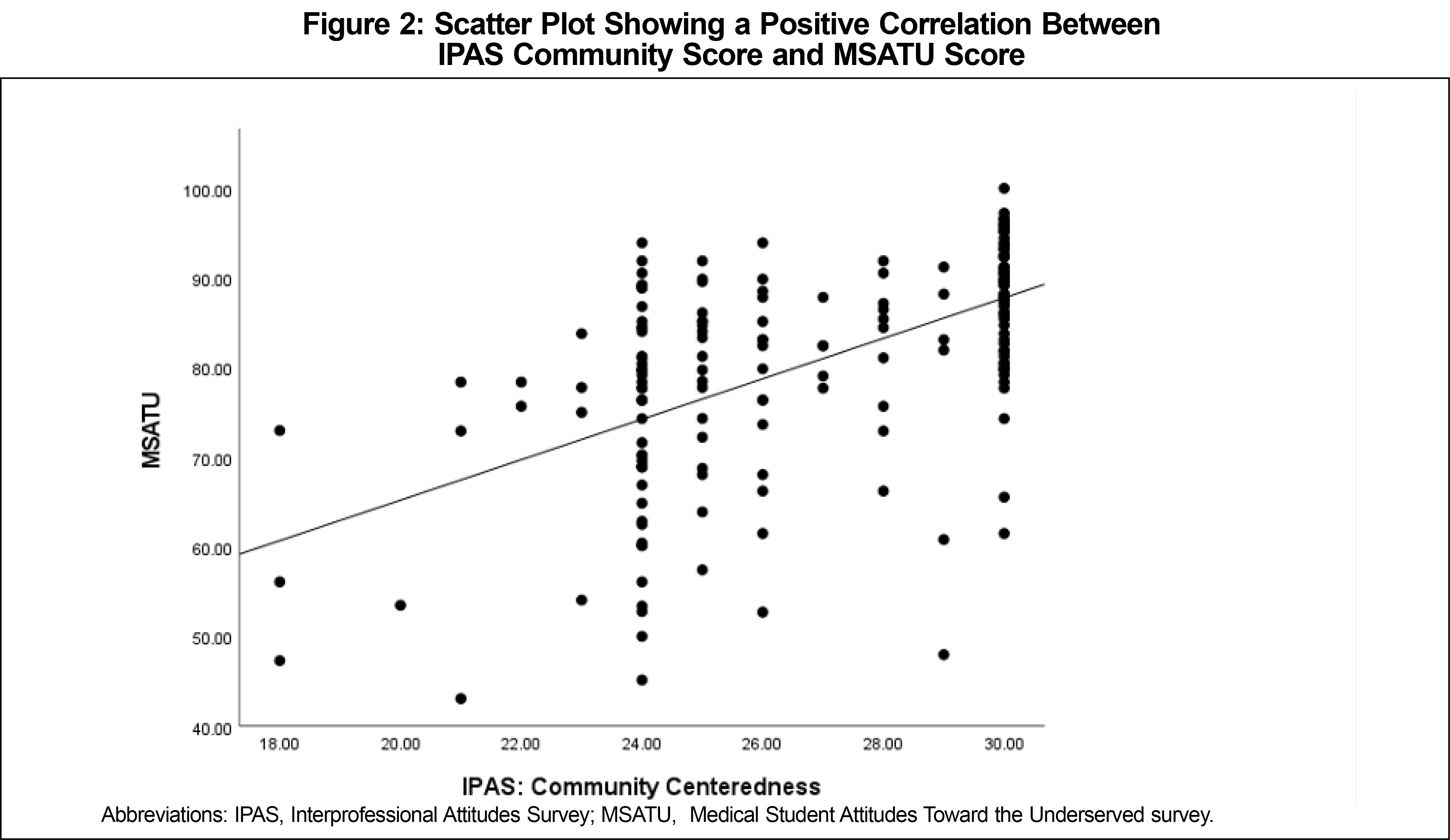
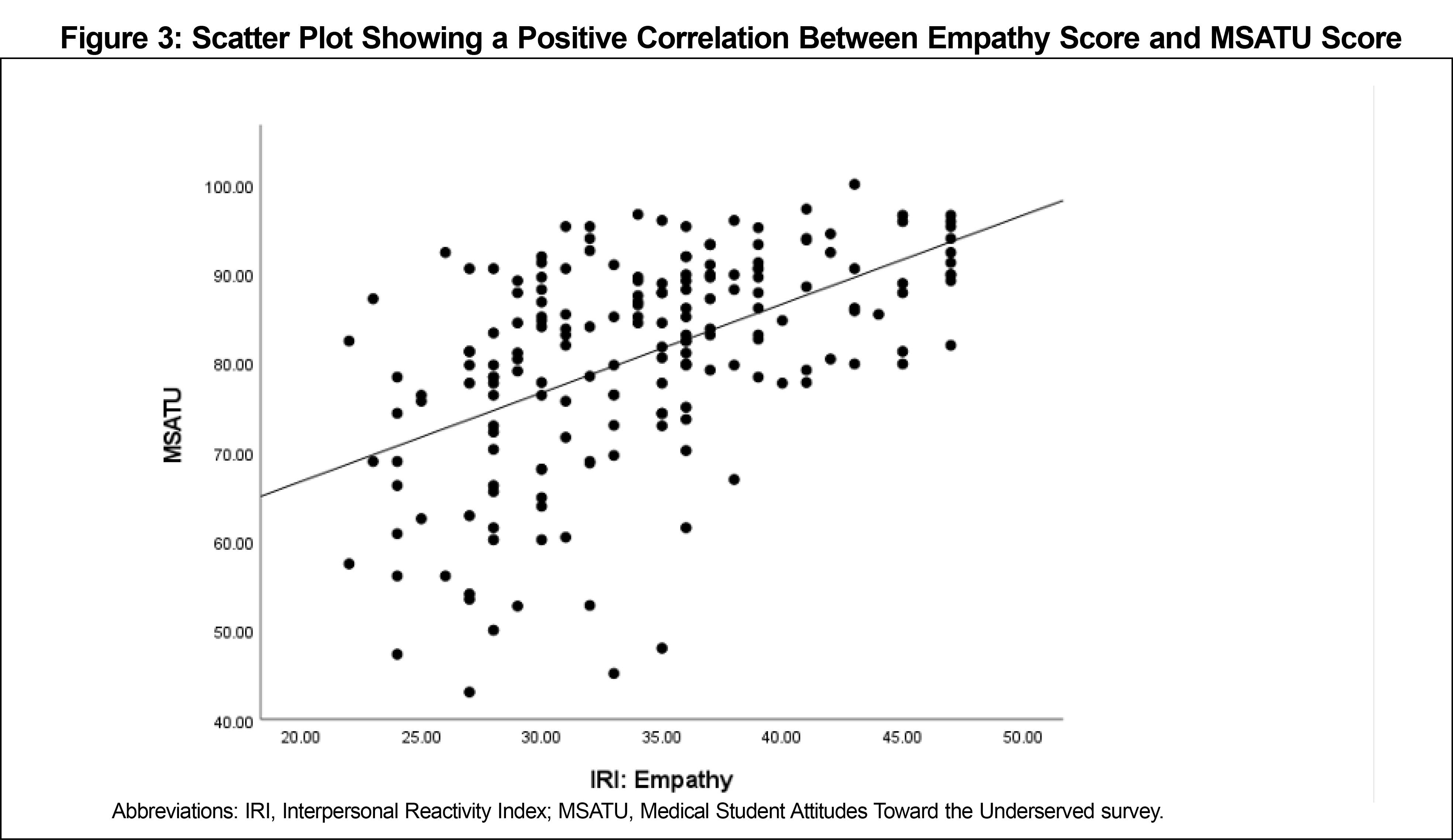
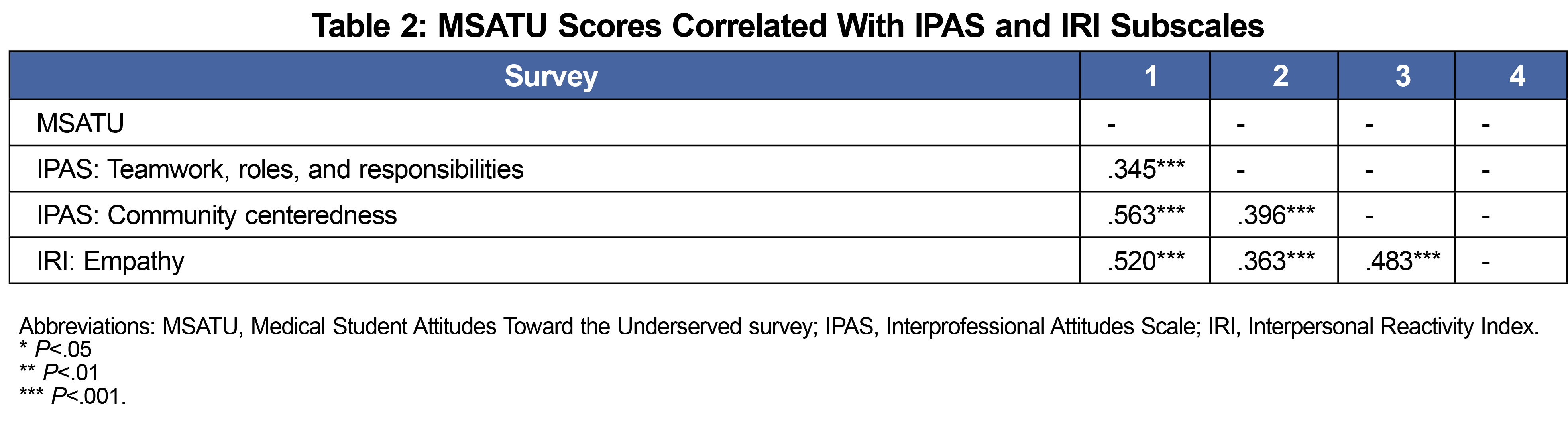
We found positive correlations between MSATU scores and the IRI empathy measurement (r [1, 184]=0.48, P<.001) and between MSATU scores and both teamwork and community centeredness as measured by IPAS (Figures 1-3, Table 2).
The results support maintenance of MSATU scores across all three time points, going against the previous hypotheses showing that students’ motivation to work with MUPs decreases throughout medical education.3,6 This consistency suggests protective factors within UTSW. Future iterations of this study could focus on individual-level data to determine whether individual students are maintaining their MSATU scores or if individual fluctuations are neutralized by group changes.
Self-identified female students consistently have more positive attitudes towards working with MUPs compared to self-identified male counterparts, aligning with previous studies and showing female identification to be a protective factor.6,13,14 One potential pitfall of this analysis is that women may be more conditioned to respond with higher empathy due to societal constructs regardless of true motivations.15 Nevertheless, there is an undeniable female-predominance in medical careers involving MUPs and primary care fields.16
The positive correlations of high MSATU scores with the IRI empathy score, the IPAS teamwork and community-centeredness scores suggest that higher empathy, teamwork, and community-centeredness serve as protective factors. This correlation is reasonable given the self-motivation, selflessness, community prioritization, and overall teamwork needed to effectively care for MUPs and the fact that these characteristics are often associated with involvement in MUP-focused experiences like volunteering in free clinics and local health initiatives.17-19 These findings could help advance education initiatives that bolster such values in students.
This study, along with many others, shows a correlation between interest in primary care and interest in working with MUPs, demonstrating how plans to practice primary care might act as a protective factor.17,20 This correlation between primary care and working with MUPs can be explained by how both realms tend to attract trainees pursuing medicine as a calling. It is important to emphasize the immense need for subspecialized practitioners motivated to work with MUPs, highlighted by the decreased MSATU scores of students interested in non-primary care specialties.21 Correspondingly, the negative correlation between MSATU scores and students involved in research could be associated with higher research expectations within more intense non-primary care subspecialities.22
Our study’s strengths include the use of multiple previously-validated tools in combination, evaluation across different time points, and assessing specific factors within one institution. Limitations of this study include decreasing response rates among older medical students likely associated with focuses shifting toward residency, and how survey fatigue likely impacted survey completion and the thoughtfulness of responses. Additionally, it is possible that students with interest in MUPs would be more inclined to respond to a survey studying these concepts and that students might feel pressured to report exaggerated motivations toward MUPs, skewing MSATU scores higher. Lower survey responses in the third time point could have been associated with fourth-year students with lower MSATU scores being less likely to respond to the survey, shifting the overall MSATU average of that time point higher. However, most conclusions involve comparisons of other variables in relation to MSATU scores, minimizing effects of such a skew in terms of tracking factors that influence MSATU scores. Overall, our study elucidated protective factors, including plans to practice primary care, emphasis on teamwork, community-centeredness, empathy, and female identification, that are associated with high MSATU scores throughout medical education at UTSW. Future research should be done to survey student cohorts throughout their education and track changes within their cohorts as well as in comparison to other cohorts, allowing for more targeted identification of trends and protective factors at UTSW and other institutions.
Acknowledgments
Financial Support: This study was supported by the University of Texas Southwestern Medical Center Southwestern Academy of Teachers (SWAT) Small Grants Program.
Presentations: Preliminary results have been presented at the Texas Academy of Family Physicians 2021 meeting (virtual) and 2021 Society of Teachers of Family Medicine Annual Conference (virtual) in poster format.
*Author Contributions: Ashley Herrera and Courtney Johnson served as co-lead authors and contributed equally to the study.
References
- 2017 Update: The Complexities of Physician Supply and Demand: Projections From 2015 to 2030: Final Report. Association of American Medical Colleges; February 28, 2017. Accessed August 23, 2022. https://aamc-black.global.ssl.fastly.net/production/media/filer_public/a5/c3/a5c3d565-14ec-48fb-974b-99fafaeecb00/aamc_projections_update_2017.pdf
- Crandall SJ, Volk RJ, Cacy D. A longitudinal investigation of medical student attitudes toward the medically indigent. Teach Learn Med. 1997;9(4):254-260. doi:10.1207/s15328015tlm0904_2
- Leaune E, Rey-Cadilhac V, Oufker S, et al. Medical students attitudes toward and intention to work with the underserved: a systematic review and meta-analysis. BMC Med Educ. 2021;21(1):129. doi:10.1186/s12909-021-02517-x
- Godkin M, Savageau J. The effect of medical students’ international experiences on attitudes toward serving underserved multicultural populations. Fam Med. 2003;35(4):273-278.
- Briggs AM, Wang SY, Bhowmik S, Wasag J, Pinto-Powell RC. The beyond the books program: improving medical student attitudes toward the underserved. Health Equity. 2018;2(1):98-102. doi:10.1089/heq.2018.0015
- Crandall SJ, Volk RJ, Loemker V. Medical students’ attitudes toward providing care for the underserved. Are we training socially responsible physicians? JAMA. 1993;269(19):2519-2523. doi:10.1001/jama.1993.03500190063036
- Woloschuk W, Harasym PH, Temple W. Attitude change during medical school: a cohort study. Med Educ. 2004;38(5):522-534. doi:10.1046/j.1365-2929.2004.01820.x
- Wayne S, Dellmore D, Serna L, Jerabek R, Timm C, Kalishman S. The association between intolerance of ambiguity and decline in medical students’ attitudes toward the underserved. Acad Med. 2011;86(7):877-882. doi:10.1097/ACM.0b013e31821dac01
- Chen D, Lew R, Hershman W, Orlander J. A cross-sectional measurement of medical student empathy. J Gen Intern Med. 2007;22(10):1434-1438. doi:10.1007/s11606-007-0298-x
- Norris J, Carpenter MJG, Eaton MJ, et al. Development and construct validation of the Interprofessional Attitudes Scale. Acad Med. 2015;90(10):1394-1400. doi:10.1097/ACM.0000000000000764
- Davis MH. A multidimensional approach to individual differences in empathy. Catal Sel Doc Psychol. 1980;10:85.
- Herrera A, Johnson C, Anasi C, et al. Master Survey.STFM Resource Library. Uploaded July 13, 2022. Accessed August 23, 2022. https://resourcelibrary.stfm.org/viewdocument/master-survey?CommunityKey=2751b51d-483f-45e2-81de-4faced0a290a&tab=librarydocuments
- Magalhães E, Salgueira AP, Costa P, Costa MJ. Empathy in senior year and first year medical students: a cross-sectional study. BMC Med Educ. 2011;11(1):52. doi:10.1186/1472-6920-11-52
- Hojat M, Vergare MJ, Maxwell K, et al. The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84(9):1182-1191. doi:10.1097/ACM.0b013e3181b17e55
- Baez S, Flichtentrei D, Prats M, et al. Men, women…who cares? A population-based study on sex differences and gender roles in empathy and moral cognition. PLoS One. 2017;12(6):e0179336. doi:10.1371/journal.pone.0179336
- Phillips R, Dodoo M, Petterson S, et al. Specialty and geographic distribution of the physician workforce: what influences medical student and resident choices? Robert Graham Center; 2009. Accessed August 23, 2022. https://www.graham-center.org/dam/rgc/documents/publications-reports/monographs-books/Specialty-geography-compressed.pdf
- Bazargan M, Lindstrom RW, Dakak A, Ani C, Wolf KE, Edelstein RA. Impact of desire to work in underserved communities on selection of specialty among fourth-year medical students. J Natl Med Assoc. 2006;98(9):1460-1465.
- Smith SD, Yoon R, Johnson ML, Natarajan L, Beck E. The effect of involvement in a student-run free clinic project on attitudes toward the underserved and interest in primary care. J Health Care Poor Underserved. 2014;25(2):877-889. doi:10.1353/hpu.2014.0083
- Weitzman CC, Freudigman K, Schonfeld DJ, Leventhal JM. Care to underserved children: residents’ attitudes and experiences. Pediatrics. 2000;106(5):1022-1027. doi:10.1542/peds.106.5.1022
- Tippets E, Westpheling K. The Health Promotion-Disease Prevention Project: effect on medical students’ attitudes toward practice in medically underserved areas. Fam Med. 1996;28(7):467-471.
- Strum JR. Medical student characteristics and Intent to Work with the Underserved: A Study Conducted At the University of North Carolina At Chapel Hill. 2003. doi:10.17615/6cd8-0y10
- Rosenkranz SK, Wang S, Hu W. Motivating medical students to do research: a mixed methods study using Self-Determination Theory. BMC Med Educ. 2015;15:95. Published 2015 Jun 2. doi:10.1186/s12909-015-0379-1



There are no comments for this article.