A growing body of research illustrates the importance of incorporating formal telemedicine training into postgraduate medical education.1 Studies support the validity of virtual examination for specific conditions. Several guides now exist that offer a basic systematic approach to the virtual physical examination.2-6 A myriad of technologies have been developed to support the collection of home-based objective patient data.7 However, there is no gold standard for how these tools should be employed in the virtual setting and to what extent patients may acceptably participate in gathering objective data. There is ongoing need for further research regarding the limitations of virtual medicine in order to effectively teach learners how to safely deliver care.8
During the COVID-19 pandemic, primary care offices across the United States pivoted quickly to deliver care via telemedicine. Kaiser Permanente Santa Rosa Family Medicine Residency had a longitudinal telemedicine curriculum in place prior to the pandemic. This curriculum included an introduction to virtual care, patient secure message training, and guidance on effective virtual communication with patients. Prior to the COVID-19 pandemic, approximately 10%-20% of resident clinic visits were telephone or video visits. In March 2020, these percentages flipped. Approximately 80% of appointments were virtual visits and 20% were in-person visits. This increase exposed a lack of resident confidence and skill in conducting virtual physical exams, documenting virtual exams, and assessing the limitations associated with virtual care. We conducted this project to address these knowledge gaps by adding to the existing telemedicine curriculum.
Eighteen family medicine resident physicians (postgraduate years [PGY] 1-3) participated in a single didactic session on how to conduct and document a virtual physical exam during a telephone or video visit in the ambulatory setting. This training reviewed a body system-based approach to conducting a virtual physical exam, when virtual care may be indicated, and a discussion of the limitations of telemedicine. The content was delivered through lecture, case review, and role-play. A senior resident and attending physician led the training. Sessions were 120 minutes in length for PGY-1 residents and 60 minutes in length for PGY-2 and PGY-3 residents. The difference in session duration was justified by prior telemedicine training and experience among the PGY-2 and PGY-3 residents compared with PGY-1 residents.
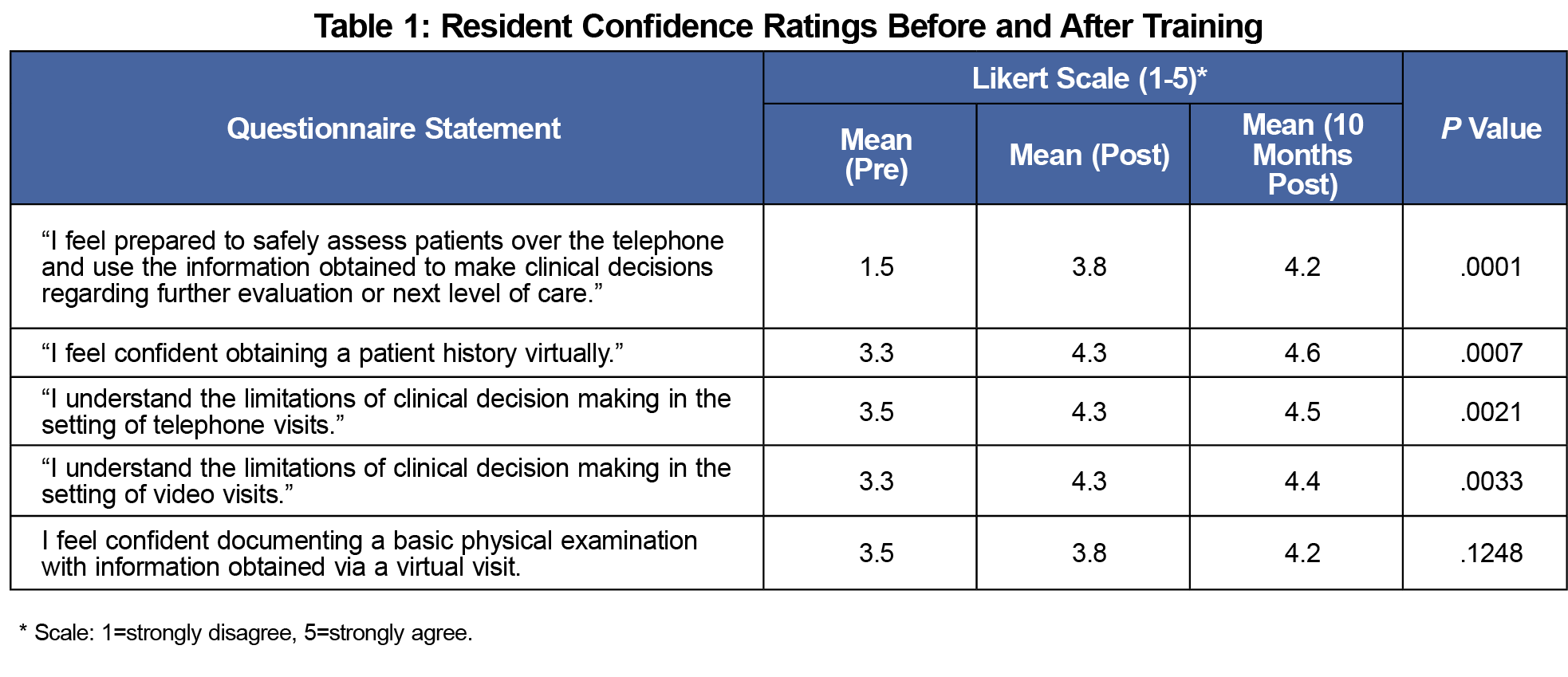
We assessed resident confidence in performing each element of the virtual physical exam through a series of surveys with 5-point Likert scale responses (1=strongly disagree, 5=strongly agree). These questionnaires were administered immediately before the training, immediately after the training, and 10 months following the training. We used descriptive and nonparametric statistical tests (Friedman Test) to assess changes in reported confidence over the three time periods. The Kaiser Permanente Northern California Institutional Review Board reviewed this project and determined it to be exempt from the full review process.
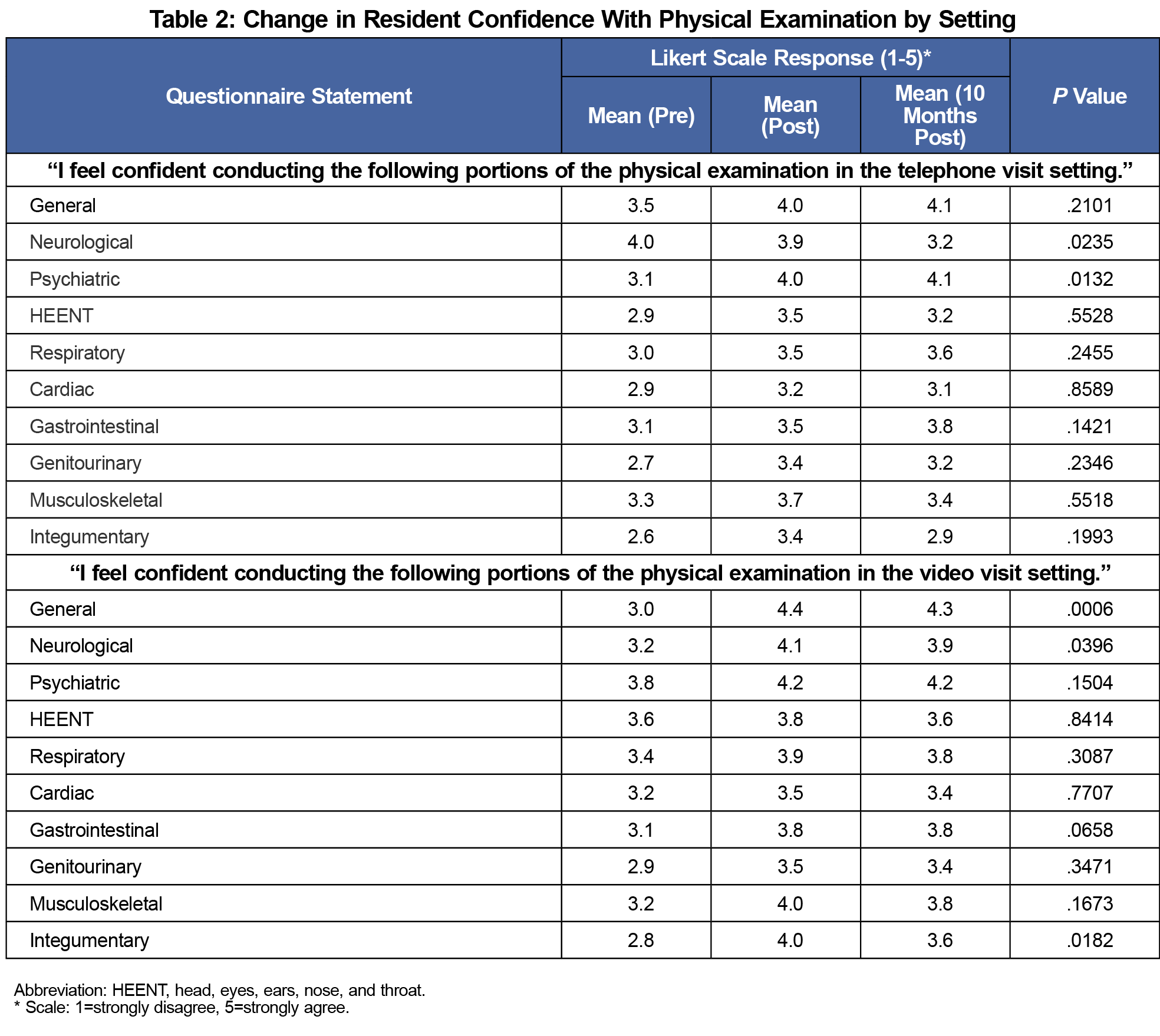
Following the training, there was a sustained improvement in resident confidence with obtaining a patient history virtually (P=.0007), conducting a physical examination in telephone settings (P=.0021) and video-based (P=.0033) settings (Table 1). Resident confidence in assessing patients in the virtual setting and using information obtained to make clinical decisions regarding further evaluation or next level of care also improved over time (P<.0001). There was significantly improved and sustained confidence in evaluating the psychiatric body system via telephone (Table 2). However, there was decreased confidence in the telephone-based evaluation of the neurological body system (P=.0235), and no significant change across other areas assessed.
Similar to the data collected regarding telephone-based examinations, confidence with video examinations was mixed (Table 2). Of the 10 body systems evaluated, residents had statistically significant immediate and sustained increase in confidence with the general, neurological and integumentary body systems. In no area was sustained decreased confidence noted.
This project provided 18 residents with formal training on telephone and video-based examinations, and assessed changes in resident confidence before, immediately after, and 10 months following the training. However, as self-reported confidence is not a proxy for actual skill level, future research is warranted to evaluate the degree to which training in telemedicine correlates with improved skill level and clinical outcomes. The generalizability of these findings is limited due to the project being conducted on a small population of residents who practiced in an organization with a robust prepandemic culture of telemedicine, which is likely not representative of the experience of family medicine residents more generally.
Specific training on telemedicine is an important component of preparing residents to safely care for patients in the virtual setting. The data obtained in this project may inform future didactic focus areas for other graduate medical education programs, including the incorporation of body system-level guidance on how to conduct the virtual examination in both the telephone and video visit settings.
Acknowledgments
The authors acknowledge the residents at Kaiser Permanente Santa Rosa Family Medicine Residency who participated in this project, as well as faculty member, Dr Lea Hoff Arcand, who supported the development of the virtual physical examination didactic and led the trainings evaluated in this research.
References
- Ha E, Zwicky K, Yu G, Schechtman A. Developing a telemedicine curriculum for a family medicine residency. PRiMER Peer-Rev Rep Med Educ Res. 2020;4:21. doi:10.22454/PRiMER.2020.126466
- Piche J, Butt BB, Ahmady A, Patel R, Aleem I. Physical examination of the spine using telemedicine: a systematic review. Global Spine J. 2021;11(7):1142-1147. doi:10.1177/2192568220960423
- Seuren LM, Wherton J, Greenhalgh T, Cameron D, A’Court C, Shaw SE. Physical examinations via video for patients with heart failure: qualitative study using conversation analysis. J Med Internet Res. 2020;22(2):e16694. doi:10.2196/16694
- Theobald M, Brazelton T. STFM forms task force to develop a national telemedicine curriculum, from STFM. Ann Fam Med. 2020;18(3):285-286. doi:10.1370/afm.2549
- Laskowski ER, Johnson SE, Shelerud RA, et al. The telemedicine musculoskeletal examination. Mayo Clin Proc. 2020;95(8):1715-1731. doi:10.1016/j.mayocp.2020.05.026
- Benziger CP, Huffman MD, Sweis RN, Stone NJ. The telehealth ten: a guide for a patient-assisted virtual physical examination. Am J Med. 2021;134(1):48-51. doi:10.1016/j.amjmed.2020.06.015
- Ansary AM, Martinez JN, Scott JD. The virtual physical exam in the 21st century. J Telemed Telecare. 2021;27(6):382-392. doi:10.1177/1357633X19878330
- Weinstein RS, Krupinski EA, Doarn CR. Clinical examination component of telemedicine, telehealth, mHealth, and connected health medical practices. Med Clin North Am. 2018;102(3):533-544. doi:10.1016/j.mcna.2018.01.002



There are no comments for this article.