Introduction: Anticipation guides (AGs) are an active learning tool with broad benefit for both learners and instructors. Though AGs have been more extensively studied in the primary and secondary education contexts, their development and implementation, as well as the benefits that they offer to medical education are not as well understood. The objective of this study was to explore the benefits that AGs afford to resident learners and instructors in the resident-led didactic conference setting.
Methods: We performed a qualitative study of the use of anticipation guides in the resident-led didactic conference setting. Participants included 47 resident learners and three chief resident instructors. Data included learner response sheets, instructor reflective journals, and field notes from nonparticipant observation. Data analysis followed guidelines for content analysis.
Results: Results indicate that AGs highlight changes in knowledge and thinking, prompt learners to reflect on their learning, and offer valuable insight into learner achievement and uncertainty to instructors. This input promotes formative assessment of learners and encourages instructors to improve their practice.
Conclusions: Anticipation guides are an easy-to-implement active learning strategy with multiple benefits in the resident didactic conference setting. Their use helps learners recognize strengths and weaknesses and identify gaps in knowledge—behaviors consistent with the goals of residency as espoused by the Accreditation Council for Graduate Medical Education. Including AGs in instruction also benefits instructors in that they provide insight into learners' thinking and knowledge development and allow educators to assess the efficacy of their instruction.
Educational research has consistently demonstrated that activating a learner’s fund of knowledge prior to instruction provides a foundation for the assimilation of new knowledge1,2 while allowing for misconceptions related to instructional content to surface.3,4 At the conclusion of instruction, revisiting prior knowledge and misconceptions through motivated reflection highlights how learners’ thinking has changed and elevates the process of meaning-making to conscious awareness.5 One instructional strategy that is effective in activating prior knowledge,3,6 highlighting misconceptions,7,4 and promoting reflection on learning8 is the anticipation guide. A type of advanced organizer, anticipation guides (AGs) consist of a series of statements related to the content of a didactic activity that learners are asked to evaluate based on their prior knowledge and understanding. Presented in a true/false format, AG statements generally ask learners to draw on their past experiences and potentially challenge beliefs or assumptions.4 Like most active learning strategies, AGs embody a constructivist approach to learning in which the learner is actively involved in the construction of meaning based on prior knowledge and experience.
Beyond activating prior knowledge and highlighting misconceptions, AGs offer additional benefits to learning as they prime learners for important concepts in a didactic activity,9,3 encourage predicting,7 arouse curiosity,10 and increase engagement.11 For instructors, learner responses from anticipation guides serve as input for formative assessment and may indicate when additional support is needed.12
Studies evaluating the use of AGs in medical education are scarce. As the Accreditation Council for Graduate Medical Education (ACGME) stipulates that residents demonstrate ability in “identifying strengths, deficiencies, and limits in… knowledge and expertise,”13 a tool that fosters these skills within structured didactic activities holds promise for graduate medical education. Moreover, promoting a scholarly, research-informed approach to instruction aligns with the commitment to excellence in teaching as espoused by the ACGME.13 Thus, understanding how pedagogical tools such as AGs function within resident didactic conferences combined with indications for their implementation is of interest to the graduate medical education (GME) community. In this study, we address the paucity of literature investigating the use of AGs in the resident didactic conference to answer the following research questions:
- In what ways do anticipation guides highlight changes in thinking and help resident learners identify strengths and limitations of knowledge?
- In what ways do anticipation guides provide instructors with insight regarding learner development and remaining uncertainties?
We conducted a qualitative case study investigating the implementation of anticipation guides during a series of five, 1-hour, resident-led didactic conferences as part of an ambulatory rotation for internal medicine residents. Conferences took place in the department’s didactic classroom from March 2021 to April 2021. Topics were geriatrics and chronic diarrhea.
A purposive sample of 47 resident learners as well as three of the four chief residents from a large, university-based internal medicine residency program in Worcester, Massachusetts consented to participate. The dataset for the study consisted of (a) resident response sheets that included completed anticipation guides and responses to a follow-up question asking learners to identify the “muddiest point,” or the most challenging/unclear aspect of the talk (n=47), (b) field notes from nonparticipant observation completed by the first author (n=5), and (c) chief resident reflective journals (n=4) in which the chief resident-educators actively reflected on their instruction. We first analyzed differences in pre- and postinstruction AG responses to establish the number of residents whose knowledge or thinking demonstrated a change as a result of instruction. Next, we used qualitative content analysis to explore themes within the resident learners’ responses to the “muddiest point” follow-up question, field notes from nonparticipant observation, and the chief residents’ reflective journals. The study was deemed exempt by the institution’s institutional review board.
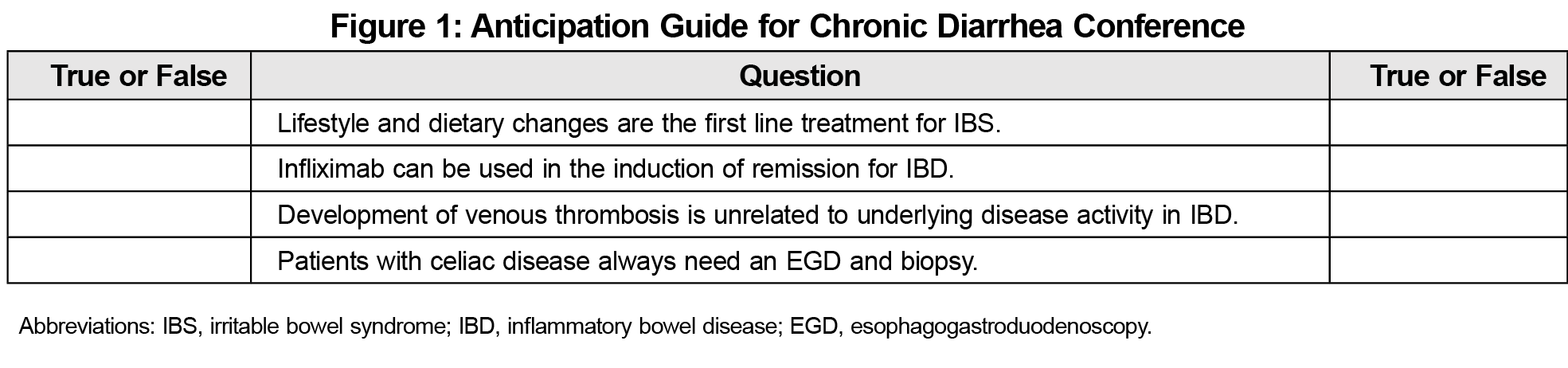
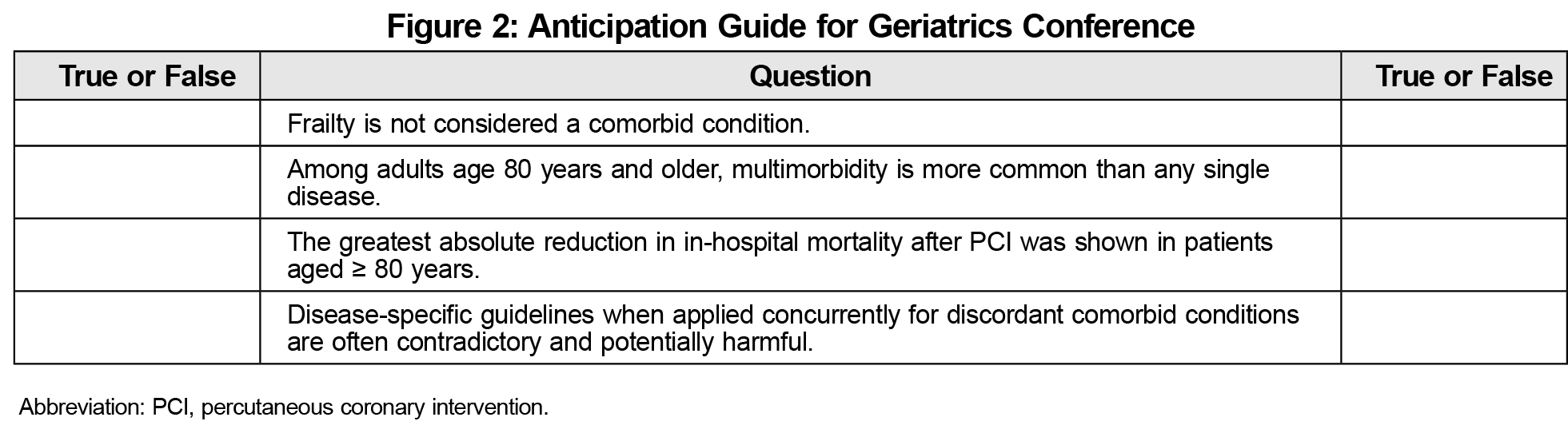
The AGs for each conference can be found in Figures 1 and 2. Residents were given approximately 5 minutes prior to instruction to complete the AG, as well as 5 minutes at the conclusion to reevaluate their responses and reflect on changes in knowledge to identify the “muddiest point,” or the most challenging/unclear aspect of the conference on their response sheets.
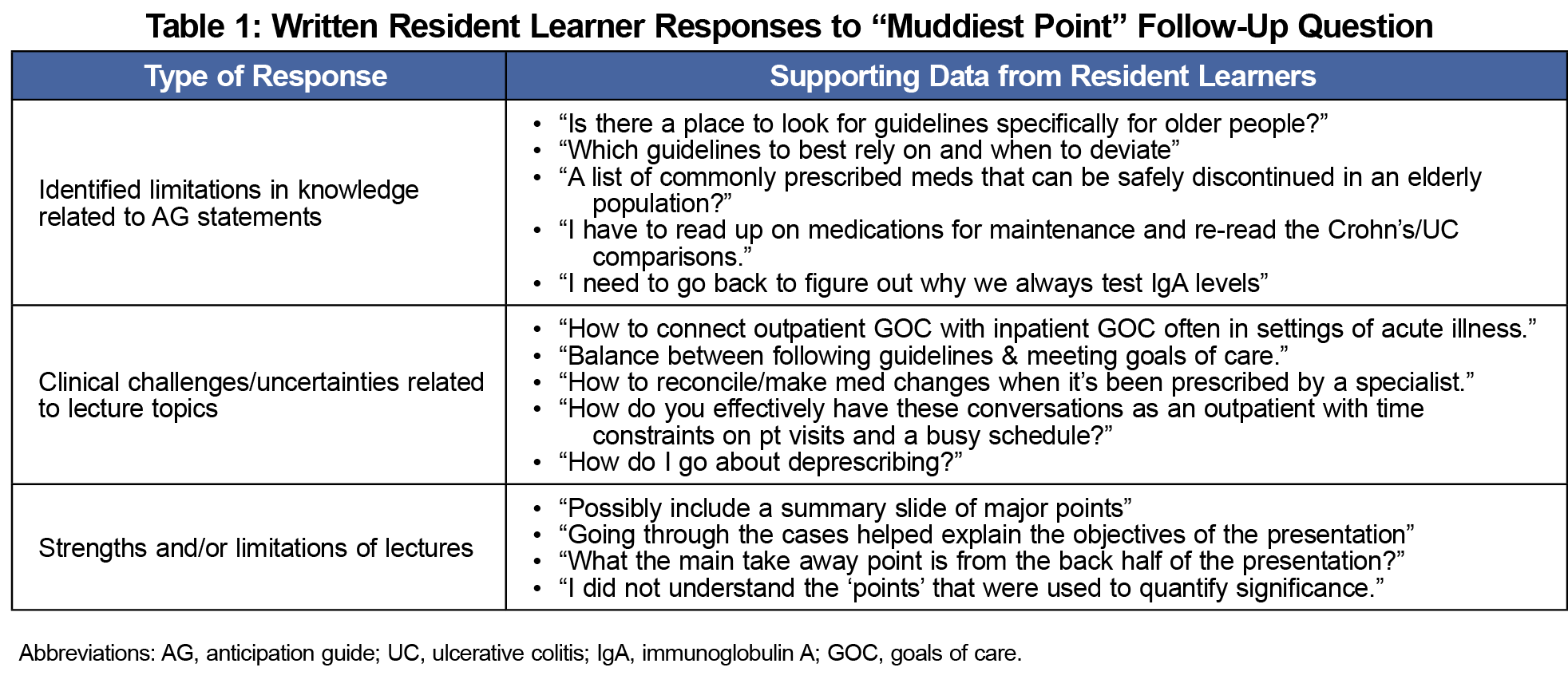
Of the 47 resident learners who attended the didactic conferences, 35 indicated change in knowledge or thinking on their anticipation guides. More importantly, residents were asked to reflect on how their knowledge or thinking had changed as demonstrated by the AG in order to identify the “muddiest point” of the lecture. Motivated by the AG statements, this reflection allowed learners to further identify gaps in knowledge and/or remaining areas of uncertainty after instruction. Responses fell into three general categories: identified limitations in knowledge related to AG statements, clinical challenges/uncertainties related to lecture topics, and insight into strengths and/or limitations of the lectures. Table 1 provides further detail regarding residents’ written responses to the follow-up question.
For chief resident instructors, reviewing AG responses afforded insight into the effectiveness of their instruction. As one chief resident instructor commented in her reflective journal,
“returning to the AG and reviewing correct answers made me more aware of whether the learning objectives were met. [This] gave me greater confidence that their knowledge base had grown.”
When resident learners identified limitations of the talks, the instructors leveraged this input to improve their teaching, leading to changes in instruction that were discussed in the reflective journals and supported through observation of the lectures. Changes included using specific language during lectures to focus attention on previously identified areas of uncertainty (eg, “This is the part of the talk that is generally not as clear so I want to spend some time here”), prompting discussion around AG responses at the conclusion of instruction, and constructing follow-up e-mail communication to address noticeable gaps in knowledge or uncertainty.
Anticipation guides hold promise for GME, particularly in the resident didactic conference. Aligned with constructivist theories of education, results suggest that learners benefit from their use by comparing beliefs and assumptions and actively constructing knowledge before and after instruction. This helps learners become aware of how their knowledge and thinking have changed and provides a point of departure for reflection on learning. Such reflection can aid learners in identifying any remaining uncertainty and/or gaps in knowledge. For instructors, AG response sheets afford valuable insight into achievement of learning objectives and indicate areas that may have been unclear to learners. Such formative assessment can inform future instruction or prompt instructors to focus on areas of identified challenge. Chief resident instructor responses also emphasized the need to include specific interaction around anticipation guides to facilitate an in-the-moment awareness of achievement. This may include asking learners to share how their thinking has changed and, subsequently, to support such changes with evidence from instruction.
Limitations of our study include a single context (resident-led didactic conferences) as well as learners from a single program. Additionally, demographic data including program year were not collected to protect the identity of the participants. Thus, we cannot make claims as to how resident trainee’s level may have affected AG responses. Finally, as with all qualitative analysis, researcher bias may affect interpretations, though data methods triangulation aids in mitigating this bias. Despite these limitations, we believe the AGs may effectively be implemented across programs and conference formats (eg, morning report, noon conference, etc).
References
- Liu Z-X, Grady C, Moscovitch M. Effects of prior-knowledge on brain activation and connectivity during associative memory encoding. Cereb Cortex. 2017;27(3):1991-2009.
- Wetzels SAJ, Kester L, van Merrienoer JJG. Adapting prior knowledge activation: Mobilisation, perspective taking, and learners’ prior knowledge. Comput Human Behav. 2011;27(1):16-21. doi:10.1016/j.chb.2010.05.004
- Downey MT, Long KA. Teaching for historical literacy: Building knowledge in the history classroom.Taylor & Francis Group; 2015. doi:10.4324/9781315717111
- Duffelmeyer FA. Effective anticipation guide statements for learning from expository texts. J Read. 1994;37(6):452-457.
- Graffam B. Active learning in medical education: strategies for beginning implementation. Med Teach. 2007;29(1):38-42. doi:10.1080/01421590601176398
- Yell MM, Scheurman G, Reynolds K. The anticipation guide: motivating students to find out about history. Soc Educ. 2004;68(5):361-363.
- Antonnaci PA, O’Callaghan CM. Promoting literacy development: 50 research-based strategies for K-8 learners.Sage Publications; 2011.
- Adams AE, Pegg J, Case M. Anticipation guides: reading for understanding. Math Teach. 2015;108(7):498-504. doi:10.5951/mathteacher.108.7.0498
- Blackburn BR, Witzel BS. Rigor in the RTI and MTSS classroom: Practical tools and strategies.Taylor & Francis Group; 2018. doi:10.4324/9781315639406
- Merkley DJ. Modified anticipation guide. Read Teach. 1996/1997;50(4):365-368.
- Pegg J, Adams A. Reading for claims and evidence: using anticipation guides in science. Sci Scope. 2012;36(2):74-78.
- Fenty NS. Using anticipation guides to support comprehension of science informational text. Intervention Sch Clin. 2019;54(3):141-148. doi:10.1177/1053451218767902
- ACGME. Common program requirements (Residency).Accreditation Council for Graduate Medical Education; 2018.



There are no comments for this article.