Background: In March 2020 with the onset of the COVID-19 pandemic, clinical rotations abruptly ceased, and telemedicine became an alternative to in-person patient care. This study investigates factors associated with long-term adoption of telemedicine during family medicine clerkships.
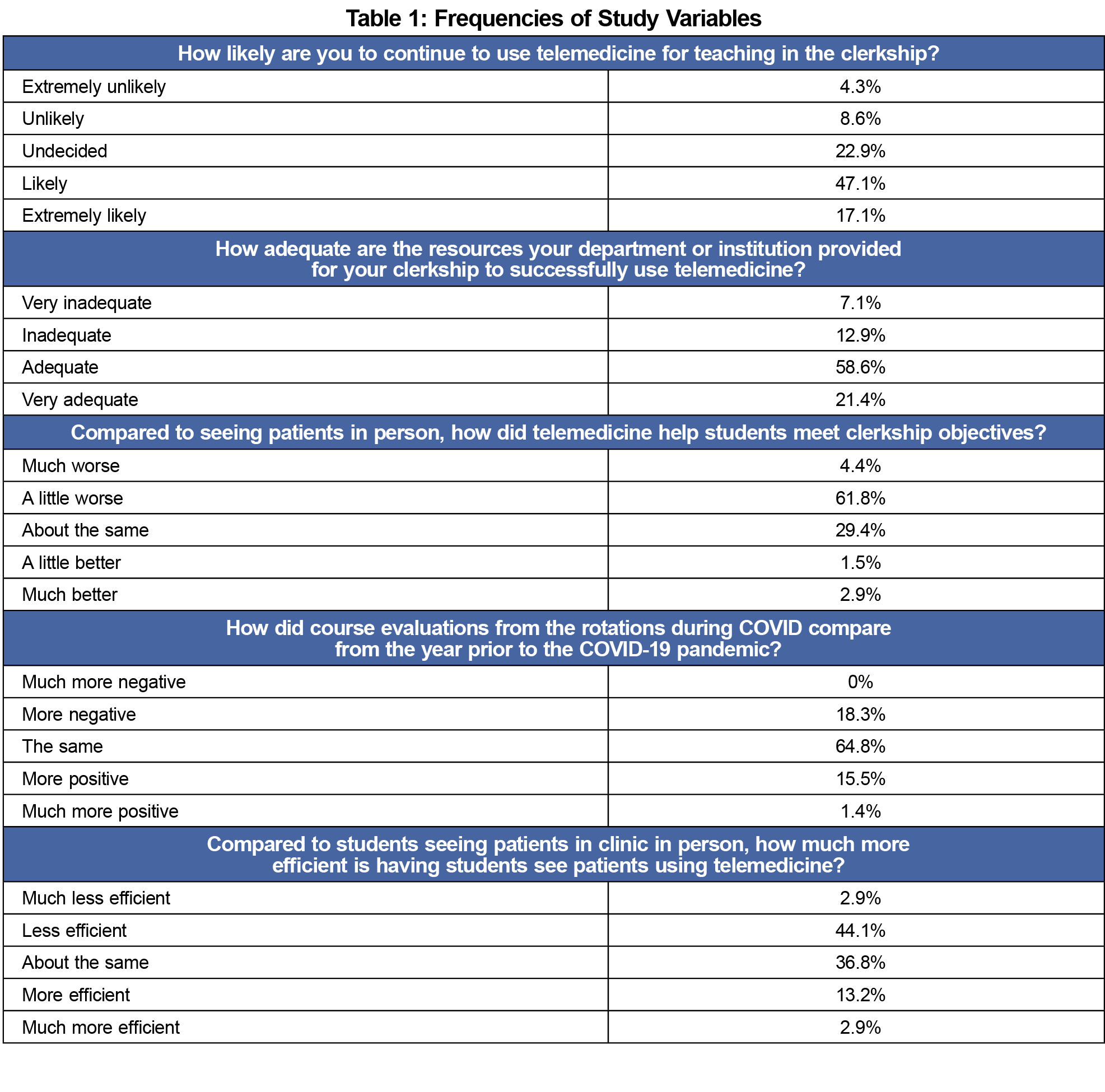
Methods: Data were gathered from the 2021 CERA survey of family medicine clerkship directors. Participants answered questions about the use of telemedicine in the clerkship, adequacy of telemedicine resources, how well telemedicine visits helped students meet course objectives, quality of course evaluations, efficiency of students seeing patients using telemedicine, and likelihood of continuing use of telemedicine once in-person visits are reinstated.
Results: The response rate was 48.8%. While most clerkship directors did not use telemedicine prior to the COVID-19 pandemic with their own patients, most had medical students utilize telemedicine during the pandemic. Clerkship directors were more likely to continue having students use telemedicine in the clerkship if it helped them meet clerkship objectives, if telemedicine visits were efficient, and if course evaluations were positive. Adequacy of resources was not associated with likelihood of retaining telemedicine in the clerkship.
Conclusions: Family medicine clerkship directors will likely continue to have students see patients via telemedicine, particularly if feedback is positive. Family medicine educators need to develop and evaluate new telemedicine curriculum for learner benefit, patient acceptability, and overall care quality.
Medical student education profoundly changed in March 2020, when the Association of American Medical Colleges (AAMC) recommended temporarily suspending medical student clinical activities due to the COVID-19 pandemic, requiring rapid development of alternative methods of medical education.1-3 In 2017-2018 about 60% of medical school curricula4 had a component of telemedicine. Since the onset of the pandemic, we can reasonably expect that medical schools incorporated at least some form of telemedicine in clinical rotations. Some studies completed since the pandemic began found that utilizing telemedicine in the clerkship can help students gain clinical knowledge, practice communication skills, and meet clerkship learning objectives.5,6
Some COVID-related changes clerkship directors made, such as increasing online resources and using clinical simulation, may become permanent if they are beneficial.1,7 Organizations are encouraging, or even requiring, telemedicine skills and training for medical students8,9 and residents.10 We have an obligation to prepare our students for this new, dynamic health care landscape. Our study investigates the use of telemedicine in the family medicine clerkship during the COVID-19 pandemic and factors associated with its long-term adoption in the clerkship curriculum.
Survey
Data were gathered as part of the 2021 Council of Academic Family Medicine’s (CAFM) Educational Research Alliance (CERA) survey of family medicine clerkship directors.11 Annual surveys go to all clerkship directors of medical schools accredited by Liason Committee for Graduate Medical Education (US allopathic medical schools) or Committee on Accreditation of Canadian Medical Schools (Canadian medical schools). Final survey questions were modified following pilot-testing.
The survey was emailed to 147 US and 16 Canadian clerkship directors in April and May, 2021. Invitations to participate included a personalized letter signed by CAFM organization presidents and a link to the survey via SurveyMonkey. Three US emails were undeliverable and were removed, resulting in 160 delivered invitations. Nonrespondents received three weekly requests, one final request at 2 days before closing the survey, and a personal email to verify their clerkship director’s status, check accuracy of email addresses, and encourage participation. Five clerkship director changes were identified, and new clerkship directors were invited to complete the survey. The study was approved by the American Academy of Family Physicians Institutional Review Board in April, 2021.
Survey Questions
Demographic questions included gender, ethnicity, and race of clerkship directors; and length and type of clerkship. Participants answered questions about (1) the use of telemedicine (defined as remote care of patients using a computer, tablet, or phone where the provider and patient can see and interact with each other) in the clerkship, (2) adequacy of telemedicine resources, (3) how well telemedicine visits helped students meet course objectives, (4) quality of course evaluations, (5) efficiency of students seeing patients using telemedicine, and (5) likelihood of continuing telemedicine once in-person visits are reinstated.
Analyses
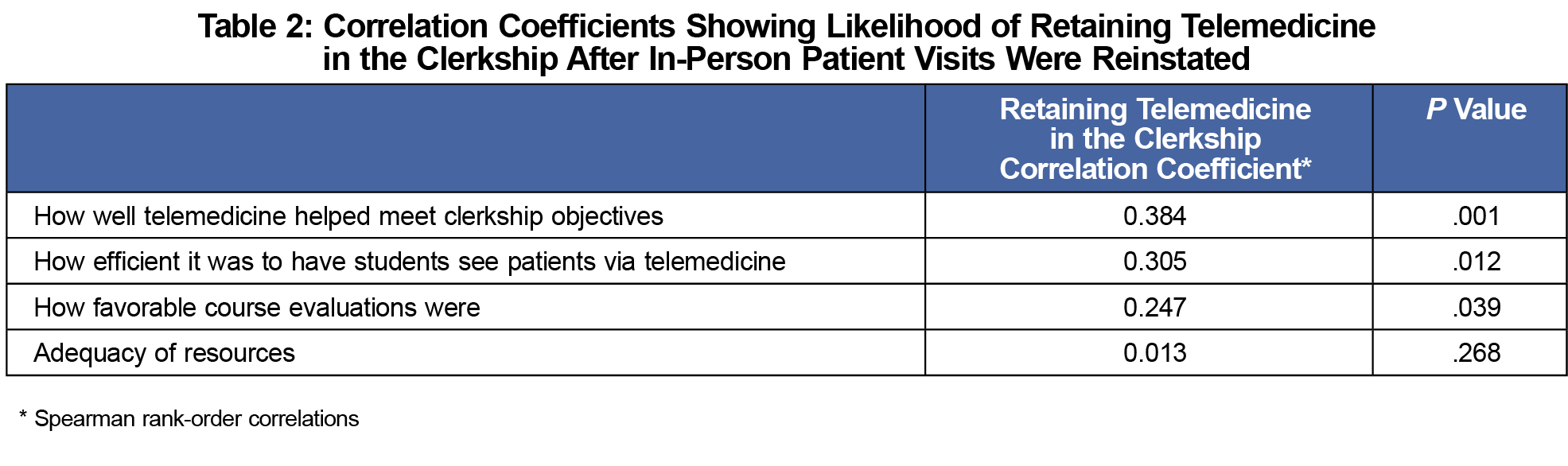
We used descriptive statistics to summarize study variables. Spearman rank-order correlations for ordinal data determined associations between likelihood of continuing telemedicine (extremely unlikely to extremely likely) and adequacy of telemedicine resources (very inadequate to very adequate), how well telemedicine helped students meet objectives (much worse to much better), course evaluations (much more negative to much more positive), and efficiency of students seeing patients using telemedicine (much less efficient to much more efficient).
A total of 78 out of 160 (48.8%) family medicine clerkship directors responded to the survey. Most respondents were female (56.8%), White (73.1%), and non-Hispanic or non-Latino (95.6%). Most clerkships (69.3%) were block only rather than longitudinal or a combination, and were either 4 (36.5%) or 6 (26.9%) weeks long. Prior to the COVID-19 pandemic, 91.5% of clerkship directors reported using telemedicine with fewer than 5% of their own patients indicating telemedicine was not widely used. However, at the start of the pandemic (March 2020-June 2020), 80.6% began having medical students use telemedicine. Most clerkship directors (81.7%) reported evaluations were the same or better than those received prior to COVID-19, and 47.0% of clerkship directors thought that having students conduct telemedicine visits was less efficient than in-person visits. Only 16.1% found telemedicine to be more efficient than in-person visits (Table 1).
Correlations were positive between likelihood of retaining telemedicine in the clerkship and how well telemedicine helped meet course objectives, how efficient it was to have students see patients via telemedicine, and how favorable course evaluations were (Table 2).
Clerkship directors rarely saw patients via telemedicine before the COVID-19 pandemic, but most had their students using it to see patients during the pandemic. More than half of clerkship directors reported they would continue using telemedicine for teaching in the family medicine clerkship, similar to findings from a study of internal medicine clerkship directors during the same time frame.12 The likelihood of continuing telemedicine in clerkship teaching increased if it was efficient, and its use helped meet clerkship objectives and maintain positive course evaluations. Others reported clerkship objectives can be met using telemedicine,6 and that such changes would be made permanent if they were positive for student learning.1 Since the onset of the pandemic, 13% to 17% of outpatient visits across specialties are done via telemedicine, and many patients report they will continue to utilize telemedicine visits in the future.13 However, telemedicine is unlikely to completely replace in-person visits where students can physically see and interact with patients.2
This study was limited by a low response rate that may limit generalizability to all clerkships. Low response rates are a challenge with CERA surveys, but the demographic data from our study were not vastly different from the previous year’s survey of clerkship directors that had a higher response rate.1 Also, telemedicine technology is evolving rapidly, and platforms used at the time of this survey may have become easier to use. Regardless of the platform utilized, it appears that some form of telemedicine will continue to be part of patient care.2 If telemedicine is going to become part of the educational experience, medical educators need to develop and evaluate new telemedicine curriculum for learner benefit, patient acceptability, and overall care quality.14 The AAMC created a report on telemedicine competencies,15 and these data support the need to determine best practices for integrating telemedicine into clinical practice and address competencies related to telemedicine teaching in medical school curricula to prepare future physicians.4
References
- Everard KM, Schiel KZ. Changes in family medicine clerkship teaching due to the COVID-19 pandemic. Fam Med. 2021;53(4):282-284. doi:10.22454/FamMed.2021.583240
- Lee IR, Kim HW, Lee Y, et al. Changes in undergraduate medical education due to COVID-19: a systematic review. Eur Rev Med Pharmacol Sci. 2021;25(12):4426-4434.
- Jumreornvong O, Yang E, Race J, Appel J. Telemedicine and medical education in the age of COVID-19. Acad Med. 2020;95(12):1838-1843. doi:10.1097/ACM.0000000000003711
- Pourmand A, Ghassemi M, Sumon K, Amini SB, Hood C, Sikka N. Lack of telemedicine training in academic medicine: are we preparing the next generation? Telemed J E Health. 2021;27(1):62-67. doi:10.1089/tmj.2019.0287
- Cain R, Shafer Klink D, Yunus S. Telemedicine implementation in family medicine: undergraduate clerkship during COVID-19 pandemic. Med Educ. 2020;54(11):1064-1065. doi:10.1111/medu.14313
- Hayes JR, Johnston B, Lundh R. Building a successful, socially-distanced family medicine clerkship in the COVID crisis. PRiMER Peer-Rev Rep Med Educ Res. 2020;4:34. doi:10.22454/PRiMER.2020.755864
- Weiner S. No classrooms, no clinics: medical education during a pandemic.AAMC; 2020.
- Galpin K, Sikka N, King SL, Horvath KA, Shipman SA; AAMC Telehealth Advisory Committee. Expert consensus: telehealth skills for health care professionals. Telemed J E Health. 2021;27(7):820-824. doi:10.1089/tmj.2020.0420
- Kelly J. AMA encourages telemedicine training for medical students, residents.American Medical Association; 2016.
- Association of American Medical Colleges. Telehealth Competencies Across the Learning Continuum.AAMC New and Emerging Areas in Medicine Series; 2021.
- Seehusen DA, Mainous AG III, Chessman AW. Creating a centralized infrastructure to facilitate medical education research. Ann Fam Med. 2018;16(3):257-260. doi:10.1370/afm.2228
- Henschen BL, Jasti H, Kisielewski M, Pincavage AT, Levine D. Teaching telemedicine in the COVID-19 era: a national survey of internal medicine clerkship directors. J Gen Intern Med. 2021;36(11):3497-3502. doi:10.1007/s11606-021-07061-4
- Bestsennyy O, Gilbert G, Harris A, Rost J. Telehealth: a quarter-trillion-dollar post-COVID-19 reality?McKinsey & Company; 2021.
- Bhatia RK, Cooley D, Collins PB, Caudle J, Coren J. Transforming a clerkship with telemedicine. J Osteopath Med. 2021;121(1):43-47. doi:10.1515/jom-2020-0131
- Association of American Medical Colleges. New and Emerging Areas in Medicine Series: Telehealth Competencies Across the Learning Continuum. AAMC; March 2021. Accessed July 15, 2022. https://store.aamc.org/downloadable/download/sample/sample_id/412/



There are no comments for this article.