Introduction: Primary care research is an important field of study within medicine, but little research has characterized medical students’ projects on this topic. Second-year medical students at the Keck School of Medicine (KSOM) of University of Southern California are required to complete a research project on a topic of their choice. This study seeks to describe the scope of primary care medical student research conducted by KSOM medical students and specifically Primary Care Program (PCP) pipeline students. The PCP consists of students with a vested interest in primary care, and who we hypothesize are more likely to complete a primary care project.
Methods: To assess students’ primary care (PC) research output, we reviewed and sorted 1,408 KSOM abstracts between 2014 and 2020 into PC or non-PC. PC projects were then recategorized into more specific PC topics. χ2 analysis determined significance at P<.05.
Results: We reviewed abstracts from 1,408 KSOM medical students (n=122 PCP; 1,286 non-PCP). Results revealed that the number of PC research projects conducted by 122 PCP students (67.2%, n=82) was statistically significantly higher than by 1,286 non-PCP students (14.7%, n=189, P<.00001). The most common PC research topics (n= 271) were education (patient/medical, n=71, 26%), health diversity/disparities (n=60, 22%), mental health/psychiatry/behavioral science (n=58, 21%), and community medicine (n=48, 18%).
Conclusions: Our study describes the breadth and scope of Keck medical student PC research. Supporting PC research efforts by medical students may increase the proportion of students conducting PC research, students choosing PC careers, and faculty producing PC scholarship.
Many students choose to conduct primary care research (PCR) projects. PCR can broadly be defined as research in the context of primary care (PC). More specifically, it includes basic, clinical, health services, health systems, and educational research.6 PCR recognizes the health system’s multifaceted nature, the socioenvironmental factors impacting patients, and provides evidence for quality improvements and health education.7-10 PC evidence regularly informs global clinical guidelines.11 Engaging students in scholarship advances research output and may encourage interest in PC specialties.12 This is crucial because the United States will lack up to 50,000 primary care physicians by 2030.12 Despite its importance, there is limited literature on medical student PCR projects. One of the few published studies, from the University of New South Wales, found that 15.5% of students conducted PCR projects, with common themes being mental health and/or substance abuse, older adult care, common chronic diseases, and health issues facing diverse communities.13
At the Keck School of Medicine (KSOM) of University of Southern California (USC), second-year medical students must complete a required scholarly project (RSP), that culminates in an abstract and poster forum. These KSOM faculty-mentored research projects can be in a discipline of each student’s choice and many students choose projects based on existing mentors, research interests, and research fairs.
Among KSOM medical students, those interested in PC can apply to be part of the Primary Care Program (PCP) at matriculation.14 This pipeline program has grown since 2011 from 12 to 32 students per year and provides longitudinal PC experiences, including exposing students to PC community-based clinics, lifestyle counseling, PC skills-based teaching, and mentorship. PCP students may be more likely to complete a PCR project because of their predisposed interest in PC and access to PC mentors.
Our study seeks to describe the scope of PCR conducted by KSOM medical students, and specifically look at PCR projects completed by both PCP and non-PCP students.
Each year, approximately 186-second year KSOM students complete an RSP. All RSP abstracts are compiled into an annual book. The abstracts from 1,408 individual students were reviewed from 2014 to 2020 by two study team members independently and characterized as PC or non-PC research based on title and content. PCR projects must have met the PC definition, specifically including basic, clinical, health services, health systems, and educational research in the PC context.6 Non-PC projects included research conducted in the hospital and about diseases commonly addressed by specialists (ie, neuro-oncology, tumors, etc). The interrater reliability for PC vs non-PC categorization was 91%.
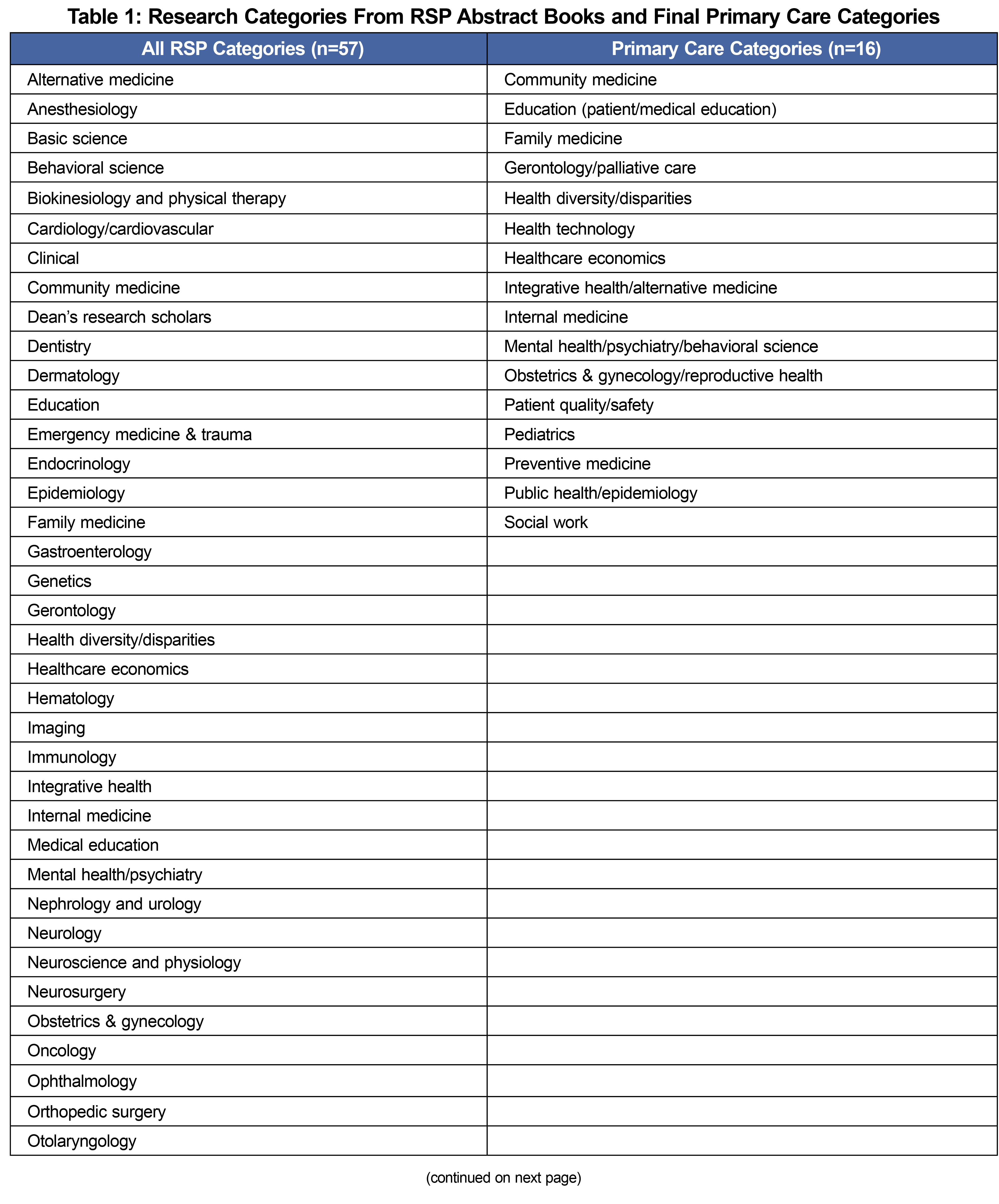
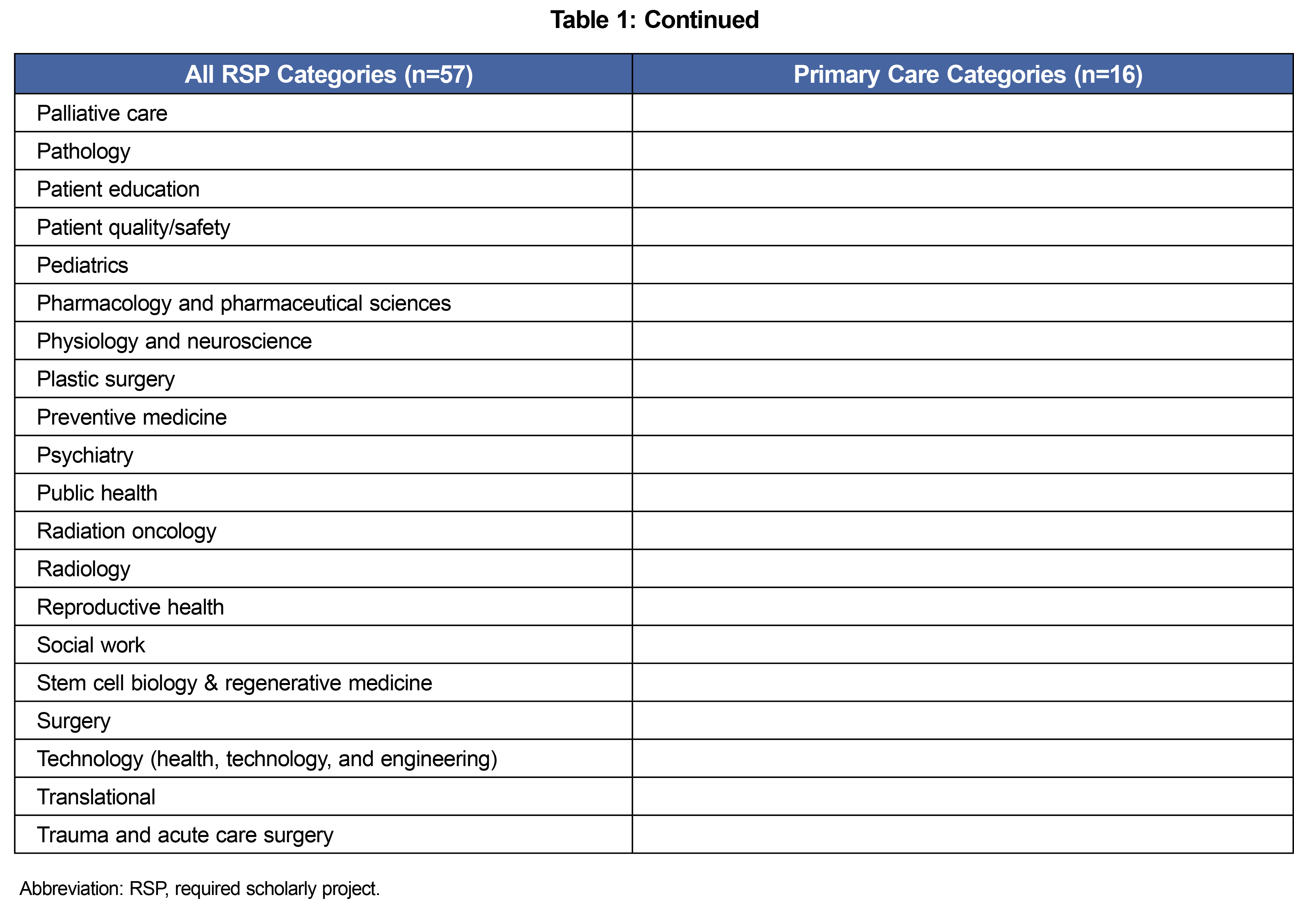
PCR projects were then recategorized into one to two distinct PCR topics using a priori categorization. The final 16 PC topics were derived from the 57 initial categories in the RSP abstract books (Table 1). Non-PC categories (ie, gastroenterology, neurology, etc) were excluded. Two study team members collaboratively decided upon PC topic recategorization. After recategorization, we separated PCR projects conducted by PCP students for analysis.
χ2 analysis determined significance at P<.05. USC’s institutional review board classified the research as exempt.
We reviewed 1,408 individual KSOM student RSPs and 271 students (19.2%) completed PCR projects. Among the 122 PCP students, 67.2% (n=82) completed a PCR project and among the 1,286 non-PCP students, 14.7% (n=189) completed a PCR project (P<.00001).
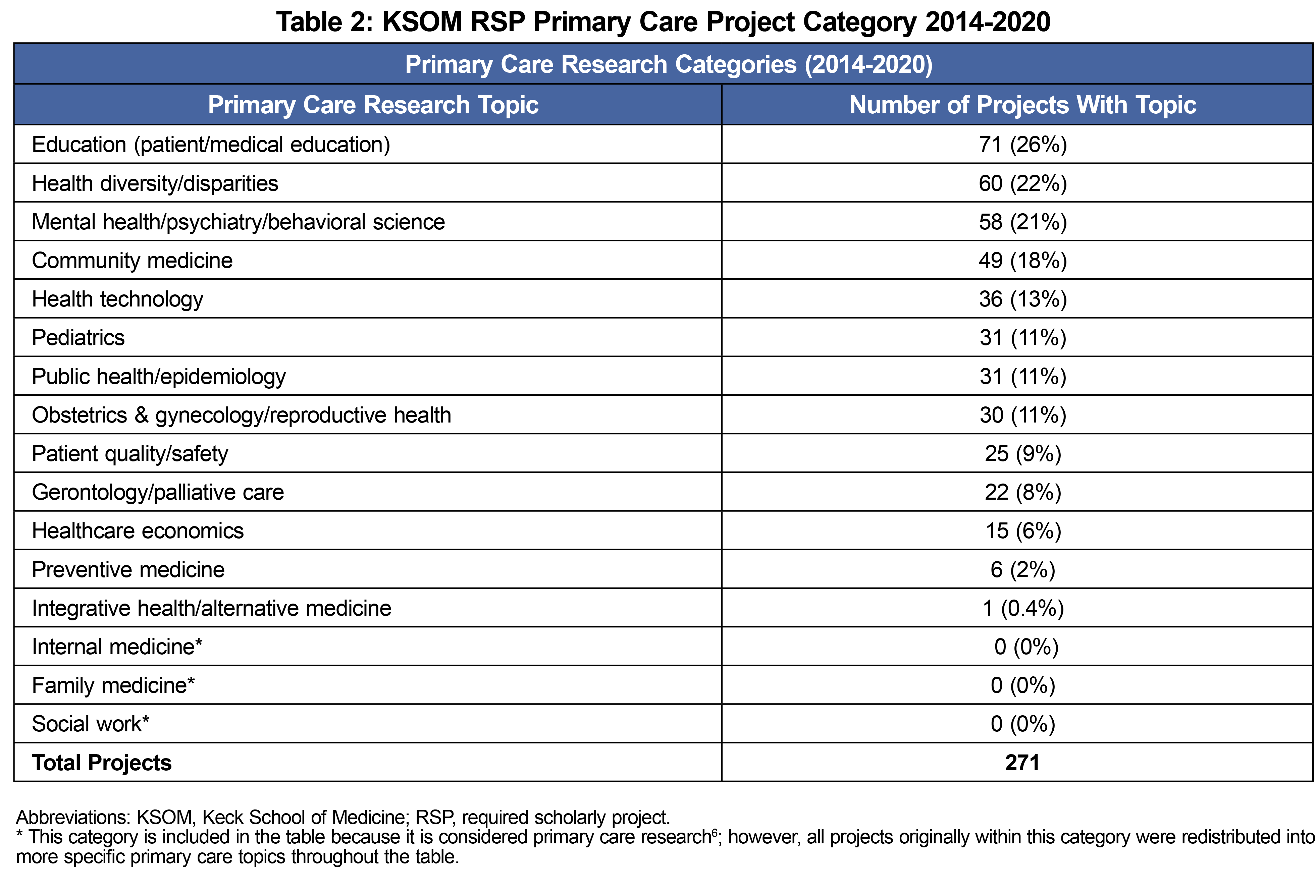
We categorized the PCR projects by topic(s). Among 271 PCR projects, 435 topic assignments were made, indicating that just under half of the abstracts received two categorizations. The most common PCR topics (n=271) were education (patient/medical education, n=71, 26%), health diversity/disparities (n=60, 22%), mental health/psychiatry/behavioral science (n=58, 21%), and community medicine (n=48, 18%, Table 2).
PCR is broad and addresses the health needs of the general population.7,8 Despite its importance, however, there is a significantly lower rate of PCR output when compared to more specialty-focused disciplines.15
In order to foster PCR, it is important for primary care physicians to be equipped with research skills, which is not typically a focus of residency training.16,17 Providing PCR opportunities and support for students may increase the research pipeline. In this study, 14.7% (n=189) of non-PCP medical students and 67.2% (n=82) of PCP students conducted PCR projects. The proportion of PCR projects conducted by all KSOM medical students (19.2%, n=271) is similar to the University of New South Wales (15.5%), but may be higher because of the PCP.13
Describing the scope of PCR highlights its impact on patient and population needs. Among the PCR projects, education (patient/medical), health diversity/disparities, mental health/psychiatry/behavioral science, and community medicine were common topics. These topics represent PC’s broad pillars. Also consistent with New South Wales, a significant proportion of projects researched health diversity/disparities.13 Many projects also focused on two PC topics, showcasing the field’s multifaceted nature.
Our study had some limitations. Although care was taken to uniformly identify PCR topics, recategorization may have inadvertently misclassified some projects. We were not blinded to the abstract authors, which may have introduced unintentional bias. PCR projects were limited to two subcategorization topics, which we felt sufficiently categorized nearly all the abstracts. Finally, students were required to have a USC research sponsor/mentor, which may have limited community-based PCR opportunities.
This is one of the first studies to look at and further describe PCR conducted by US medical students. Future research would benefit from evaluating whether medical school investment into PCR can increase the proportion of students conducting PCR, choosing PC careers, and PC scholarship output. There may also be PCR topics not as readily available for medical students, such as clinic data internal metrics, that could be further explored. Supporting medical student PCR may help develop future primary care physicians with research skills utilized throughout their career.
References
- Collier AC. Medical school hotline: importance of research in medical education. Hawaii J Med Public Health. 2012;71(2):53-56.
- Nikiforova T, Carter A, Chang JC, DeFranco DB, Veldkamp PJ, Levine AS. Impact of a required, longitudinal scholarly project in medical school: a content analysis of medical students’ reflections. Med Sci Educ. 2021;31(4):1385-1392. Accessed March 25, 2022. doi:10.1007/s40670-021-01319-6
- . Medical student research requirement at US medical schools. Association of American Medcial Colleges. Accessed Jan 29, 2021. https://www.aamc.org/data-reports/curriculum-reports/interactive-data/medical-student-research-requirement-us-medical-schools
- King J Jr, Angoff NR, Forrest JN Jr, Justice AC. Joseph, Angoff N, Forrest J, Justice A. gender disparities in medical student research awards: a thirteen-year study from the yale school of medicine. Acad Med. 2017;93(6):1. doi:10.1097/ACM.0000000000002052
- Bierer SB, Chen HC. How to measure success: the impact of scholarly concentrations on students--a literature review. Acad Med. 2010;85(3):438-452. Accessed March 21, 2022. https://journals.lww.com/academicmedicine/Fulltext/2010/03000/How_to_Measure_Success__The_Impact_of_Scholarly.17.aspxdoi:10.1097/ACM.0b013e3181cccbd4
- Beasley JW, Starfield B, van Weel C, Rosser WW, Haq CL. Global health and primary care research. J Am Board Fam Med. 2007;20(6):518-526. Accessed August 17, 2022. doi:10.3122/jabfm.2007.06.070172
- Nottingham KL, Rush LJ, Beverly EA. Building primary care research capacity in a college of osteopathic medicine. J Am Osteopath Assoc. 2016;116(5):278-279. Accessed November 5, 2020. http://jaoa.org/article.aspx?articleid=2517489doi:10.7556/jaoa.2016.055
- The National Academies Press. Implementing high-quality primary care: Rebuilding the foundation of health care. Washington, DC: 2021.
- Westfall JM, Wittenberg H, Liaw W. Time to invest in primary care Research—Commentary on findings from an independent congressionally mandated study. J Gen Intern Med. 2021;36(7):2117-20. Accessed September 14, 2022. https://link.springer.com/content/pdf/10.1007/s11606-020-06560-0.pdf
- Bierman AS, Tong ST, McNellis RJ. Realizing the dream: the future of primary care research. Ann Fam Med. 2022;20(2):170-174. doi:10.1370/afm.2788
- Hobbs R. Is primary care research important and relevant to GPs? Br J Gen Pract. 2019;69(686):424-425. doi:10.3399/bjgp19X705149
- Spetz J, Coffman J, Geyn I. California's primary care workforce: Forecasted supply, demand, and pipeline of trainees, 2016-2030. Healthforce Center at UCSF. 2017. Accessed September 14, 2022. https://healthforce.ucsf.edu/publications/californias-primary-care-workforce-forecasted-supply-demand-and-pipeline-trainees-2016
- Uebel K, Pervaz Iqbal M, Hall J. Review of primary care research projects completed by medical students. Australian Journal of General Practice. 2020; 49(12):848-52. Accessed May 13, 2021. https://www1.racgp.org.au/ajgp/2020/december/a-retrospective-review-of-primary-care-research-pr
- Keck family medicine primary care initiative. University of Southern California Keck School of Medicine. Accessed Aug 17, 2022. https://primarycare.usc.edu/
- Hajjar F, Saint-Lary O, Cadwallader JS, et al. Development of primary care research in north america, europe, and australia from 1974 to 2017. Ann Fam Med. 2019;17(1):49-51.
- Harper D. Family medicine Researchers—Why? who? how? when? Family Medicine. 2021;53(7):647-649. /familymedicine/2021/july-august/harper-2021-0225/. Accessed Aug 16, 2021. doi:10.22454/FamMed.2021.629549
- Khalaf AJ, Aljowder AI, Buhamaid MJ, Alansari MF, Jassim GA. Attitudes and barriers towards conducting research amongst primary care physicians in Bahrain: a cross-sectional study. BMC Fam Pract. 2019;20(1):20.



There are no comments for this article.