Introduction: Performing clinical procedures is an essential component of family medicine (FM) residency training. A referral-based procedure clinic was established at our institution in 2014, and a yearly 2-week rotation was established for residents. The objective of this study was to determine the effect of a procedure clinic rotation on the numbers of procedures performed during residency training.
Methods: We conducted a retrospective review on graduating FM residents from 2009 to 2019. Data collected include type and number of procedures performed each postgraduate year. We analyzed data as mean number of procedures per resident per year. We conducted statistical comparison with Wilcoxon-Mann-Whitney two-sample rank-sum tests.
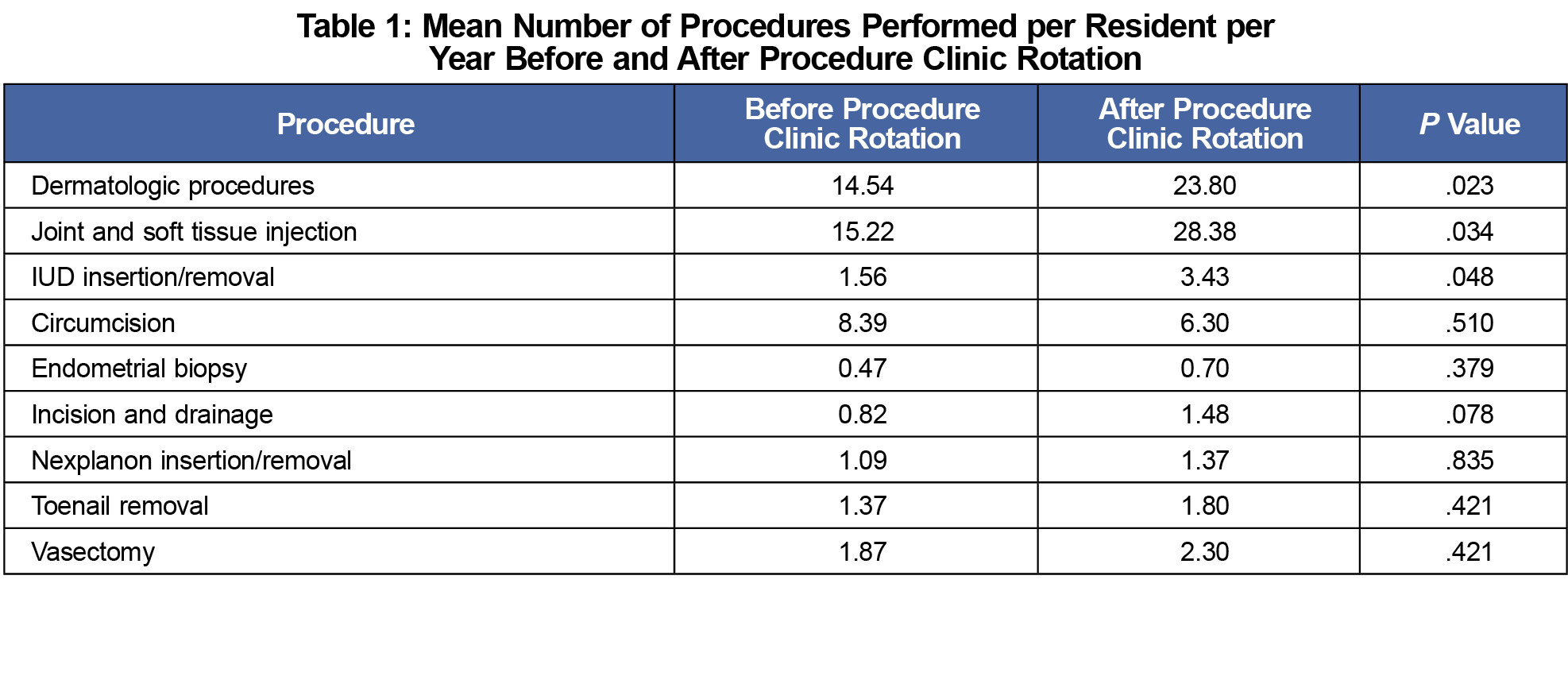
Results: Residents who participated in the procedure clinic rotation performed significantly more dermatologic procedures per year, joint and soft tissue injections and intrauterine device (IUD) insertions and removals, but did not perform significantly more circumcisions, endometrial biopsies, incision and drainages, subdermal contraceptive implant procedures, toenail removals, or vasectomies.
Conclusion: The establishment of a 2-week procedure clinic rotation for FM residents was associated with a significant increase in dermatologic procedures, joint and soft tissue injections, and IUD procedures. Further research can explore the impact of this rotation on procedural competency and confidence.
Performing procedures is an essential component of family medicine (FM) training.1 Guidelines from the Accreditation Council for Graduate Medical Education (ACGME) outline competencies including performing “all medical, diagnostic and surgical procedures considered essential for the area of practice.”2 Additionally, the Society of Teachers of Family Medicine (STFM) maintains a list of procedures required in family medicine residencies, known as “Category A” procedures.1
Procedural training remains important. Graduates of rural FM programs have greater self-reported competence in procedures when compared to urban programs, likely due to increased exposure.3 Family physicians who perform procedures report increased job satisfaction.4 Patients expect their primary care provider (PCP) to perform procedures, which helps maintain continuity, a cornerstone of primary care.5 Having a focus on procedural training also positively correlates with successful resident recruitment.6
There are challenges to performing procedures, including having the necessary equipment and office space to perform them. Providing residents procedural experience in continuity clinic can be challenging due to resident schedules and the broad scope of training.7,8 Attaining confidence in a procedure involves observing the steps and performing the procedure under supervision until residents are confident with proceeding autonomously.9 Another barrier is preceptors may not feel comfortable supervising a procedure if they have performed it infrequently in their own practice.10 One program trialed skills workshops, however these did not ultimately improve performance.11 At our FM residency training program, procedures were previously only performed during outpatient resident continuity clinic, where residents would face many of the previously-mentioned challenges.
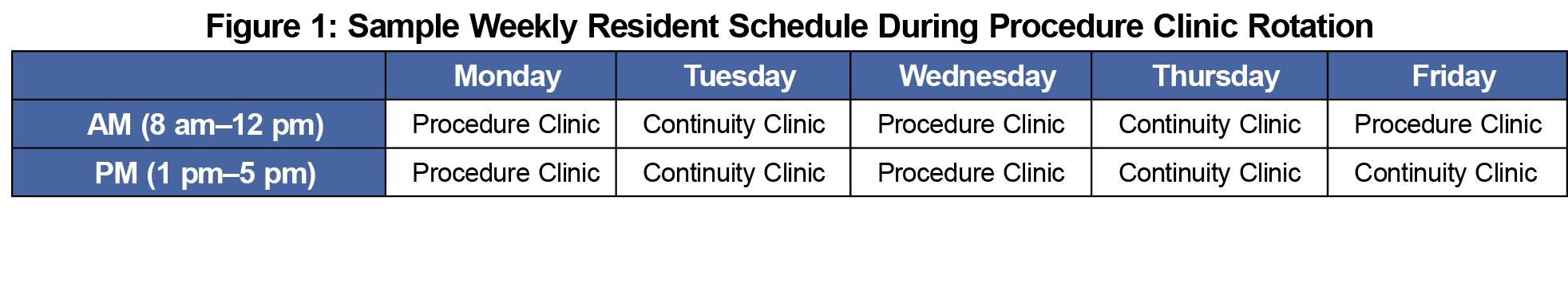
Our institution developed a referral-based procedure clinic in 2014 to streamline procedural care, staffed by family medicine and internal medicine physicians. This was a centralized location where referrals could be sent by PCPs. To improve the number of procedures FM residents perform and overcome challenges in procedural training, an annual 2-week rotation was established in each year of training (postgraduate years 1, 2, and 3). A sample weekly schedule is outlined in Figure 1, with half of the week dedicated to procedure clinic and the other half to resident continuity clinic. This study aimed to determine the impact of this procedure clinic rotation on the number of procedures that FM residents performed during their residency.
We conducted a retrospective observational study on 2009-2019 graduates at a suburban FM residency program in Southeast Minnesota. This residency program is at a large major academic tertiary medical center, with over 280 residencies and fellowships offered. The resident continuity clinic is in a rural setting, and the procedure clinic rotation is located within the core tertiary medical center in an urban setting. Nongraduating residents were excluded. Data collected included the number and type of procedures performed, both prior to and after the establishment of the procedure clinic rotation. We obtained data from resident self-logged procedure records. The collected data were grouped into two cohorts: procedures performed before and after the establishment of the procedure clinic rotation in June 2014. We analyzed data by mean procedures per resident per year of training due to the 3-year training cycle of FM residency and to allow for the inclusion of the data of the 2015 and 2016 classes.
Procedures that were selected to be analyzed were the top-nine procedural categories performed in the clinic based on volume (Table 1). Procedures falling outside these categories including epistaxis management, fishhook removal, orthopedic splinting and reductions, thoracocentesis, lumbar puncture, chest tubes, and central lines were excluded from this study due to the infrequent nature of these procedures performed in this clinic. The organization’s ethics review board reviewed this study and deemed it to be exempt from the requirement for IRB approval as it did not meet criteria for research. The organization’s education research committee also approved this study. We analyzed data utilizing JMP medical software by SAS (SAS, Inc, Cary, NC). We conducted statistical comparison with Wilcoxon-Mann-Whitney two-sample rank-sum tests. We set statistical significance at P<.05.
Ninety-one graduated FM residents were included (51.6% female, 72.5% MD, 19.8% DO, 2.2% BMBS, 4.4% MB, BCh, 1.1% MBBS). Analyzed on a mean number of procedures per resident per year basis both before and after the procedure clinic rotation, residents performed significantly more dermatologic procedures, joint and soft tissue injections, and IUD insertions and removals after the establishment of the procedure clinic rotation (Table 1). No statistically significant increase in the number of incision and drainage procedures, Nexplanon insertion and removal, toenail removal, or vasectomy was noted (Table 1).
When the procedure clinic rotation was established, this was viewed as a valuable opportunity for residents to increase their procedural capabilities by increasing procedural exposure. A similar approach was outlined by Dor in 2014.12 As indicated in Table 1, this rotation met its objectives as residents performed a statistically significant higher mean number per resident per year of dermatologic procedures, joint and soft tissue injections, and IUD removal and insertions. The remaining types of procedures did not achieve significance likely due to the lower number of procedures performed. Neonatal circumcision was the only procedural type to have a nonstatistically significant decline after the procedure clinic rotation. At our institution, neonatal circumcisions are typically performed in the newborn nursery, and an increase in this procedure type was not expected. The structure of this rotation, with half of the week in procedure clinic and the other half in continuity clinic allowed residents to maintain continuity with their outpatient practice, while gaining valuable procedural experience.
Postrotation surveys were conducted, with 24 responses received. This rotation was ranked highly by residents, with 63% (15/24) indicating it to be one of the top 10% of learning experiences, 92% (22/24) reporting it improved their skills as family physician, and 88% (21/24) reporting it above average for ensuring appropriate case load, while ensuring quality patient care and education. One resident commented, “procedures are something we all value and getting the opportunity to do a large volume of them is a privilege.” Given improvement in procedural numbers and positive resident feedback, this rotation continues to be a part of the residency curriculum.
Given practice structure variations, this approach may be difficult to replicate in other centers. This study did not assess whether procedures performed during continuity clinic increased after the procedure clinic rotation. If a similar rotation is established by other programs, further research can be conducted on measuring impacts on procedural competency and confidence. Additionally, faculty feedback could also be collected on the value of this rotation. A subgroup resident analysis was not feasible given the overall lower number of residents but is a possibility for future research.
The establishment of an annual 2-week procedure clinic rotation for FM residents was associated with significant increase in the number of dermatologic procedures, joint and soft tissue injections, and IUD procedures performed during clinical training.
Acknowledgments
Presentations: This study was was presented at the Mayo Clinic Annual Family Medicine Research Forum in October 2020.
References
- Nothnagle M, Sicilia JM, Forman S, et al; STFM Group on Hospital Medicine and Procedural Training. Required procedural training in family medicine residency: a consensus statement. Fam Med. 2008;40(4):248-252.
- ACGME Program Requirements for Graduate Medical Education in Family Medicine 2020. Accreditation Council for Graduate Medcial Education. Accessed June 20, 2022. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/120_FamilyMedicine_2020.pdf
- Goertzen J. Learning procedural skills in family medicine residency: comparison of rural and urban programs. Can Fam Physician. 2006;52(5):622-623.
- Rivet C, Ryan B, Stewart M. Hands on: is there an association between doing procedures and job satisfaction? Can Fam Physician. 2007;53(1):93, 93, 1-5, 92.
- Norris TE, Cullison SW, Fihn SD. Teaching procedural skills. J Gen Intern Med. 1997;12 Suppl 2(Suppl 2):S64-70.
- Harper MB, Mayeaux EJ Jr, Pope JB, Goel R. Procedural training in family practice residencies: current status and impact on resident recruitment. J Am Board Fam Pract. 1995;8(3):189-194.
- Choby B, Passmore C. Faculty perceptions of the ACGME resident duty hour regulations in family medicine. Fam Med. 2007;39(6):392-398.
- Kogan JR, Holmboe ES, Hauer KE. Tools for direct observation and assessment of clinical skills of medical trainees: a systematic review. JAMA. 2009;302(12):1316-1326. doi:10.1001/jama.2009.1365
- Wearne S. Teaching procedural skills in general practice. Aust Fam Physician. 2011;40(1-2):63-67.
- Wickstrom GC, Kelley DK, Keyserling TC, et al. Confidence of academic general internists and family physicians to teach ambulatory procedures. J Gen Intern Med. 2000;15(6):353-360. doi:10.1046/j.1525-1497.2000.04109.x
- MacKenzie MS, Berkowitz J. Do procedural skills workshops during family practice residency work? Can Fam Physician. 2010;56(8):e296-e301.
- Dor K. Utilization of a referral-based procedure clinic to improve procedure training and assessment in a family medicine residency. J Grad Med Educ. 2014;6(2):358-359. doi:10.4300/JGME-D-14-00063.1



There are no comments for this article.