Introduction: As the prevalence of chronic diseases increases worldwide, there is a need for educating future physicians in the use of lifestyle medicine to treat and prevent diseases. Any addition to the undergraduate medical curriculum requires a strategic educational approach with consideration for efficiency. This study aims to identify priorities for lifestyle medicine interventions in the undergraduate medical curriculum.
Methods: Third-year medical students (N=115) were surveyed on their beliefs about lifestyle medicine and their confidence in lifestyle medicine skills. The survey consisted of seven items to which students responded with how closely they agreed via a 5-point Likert scale. Descriptive statistics were reported.
Results: Most medical students entering their clinical years understand the value of lifestyle medicine in patient care (100%) and want to learn the skills and knowledge involved (98.2%). The value of lifestyle medicine counseling skills during the limited patient-doctor time was least universally acknowledged among third-year medical students (93.9%). Third-year medical students are most confident in being able to obtain a comprehensive lifestyle history (3.6±0.8) and least confident in setting clear, personalized, lifestyle change goals (3.1±0.9).
Conclusion: Future interventions to increase confidence in lifestyle medicine skills should focus on educating students on setting lifestyle change goals, personalizing prescriptions, and motivational interviewing for use in clinical care.
As the prevalence of chronic diseases continues to rise worldwide,1, 2 there is a growing need for physicians to manage these conditions by targeting lifestyle risk factors.3 Lifestyle medicine is an evidence-based science in which changes in lifestyle such as nutrition, activity, sleep, smoking, and other behaviors are recommended to prevent, treat, and reverse the progression of chronic diseases.4
Medical providers are not prescribing lifestyle changes for managing or preventing chronic diseases because of lack of knowledge, skills, education, time, confidence, or system support.5-8 Data available on nutrition training shows that most medical schools offer less than 20 hours on nutrition training, falling short of the 25 hours recommended by the Institute of Medicine.9 A recent systematic review on lifestyle medicine curricula in undergraduate medical education identified 23 curricular examples, averaging less than 14 hours in total.10 As a result, lifestyle medicine is not yet standard of care for most physicians.
A 2018 American Medical Association resolution supported legislation to incentivize and provide funding for the inclusion of lifestyle medicine in medical education.11 Due to current trends in undergraduate medical curriculum where preclinical time is shortened for additional clinical time,12 any additions need to be carefully designed for efficiency. The purpose of this study was to identify lifestyle medicine interventions in undergraduate medical education by determining which aspects of lifestyle medicine students least value and which skills students feel least confident in.
At the University of Central Florida College of Medicine (UCF), lifestyle medicine concepts are taught as a component of other courses in both the preclinical (2 years) and clinical (2 years) curriculum with no dedicated course. The preclinical curriculum includes sessions relevant to lifestyle medicine such as physiology of exercise and nutrition; lifestyle change recommendations for the management and prevention of obesity, diabetes, and heart disease; and history taking and motivational skills for lifestyle changes.
We obtained institutional review board approval from the University of Central Florida for a quality improvement project to assess the beliefs and confidence of third-year medical students in lifestyle medicine at the beginning of their clinical education years. Data presented here represent the needs assessment intervention. Completion of an online survey was required for the entire class of students (N=115) at the beginning of their third year.
The principal investigators developed a 7-item survey using both the published lifestyle medicine competencies4 and their professional expertise in the field of lifestyle medicine and medical education. The survey was content-validated by a group of medical students and a group of lay persons. This survey was delivered online and was deployed on a course management platform. The full survey and the Likert scales are available on the STFM Resource Library.13 We reported descriptive statistics using Microsoft Excel.
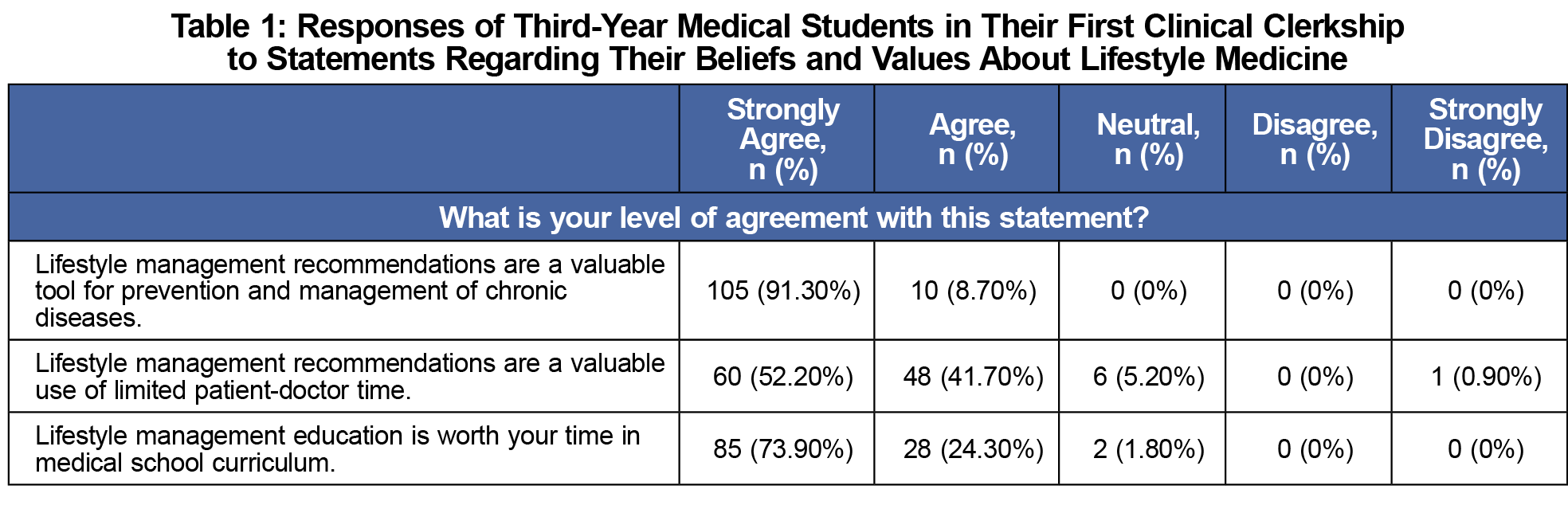
Beliefs About Lifestyle Medicine (Table 1)
One hundred percent of students agreed or strongly agreed that lifestyle management recommendations are valuable in preventing and/or managing chronic diseases; 93.9% of students agreed or strongly agreed that lifestyle management recommendations are a valuable use of limited patient-doctor time, and only 0.9% strongly disagreed with the statement. More than 98% of students agreed or strongly agreed that lifestyle management education is worth their time in medical school curriculum.
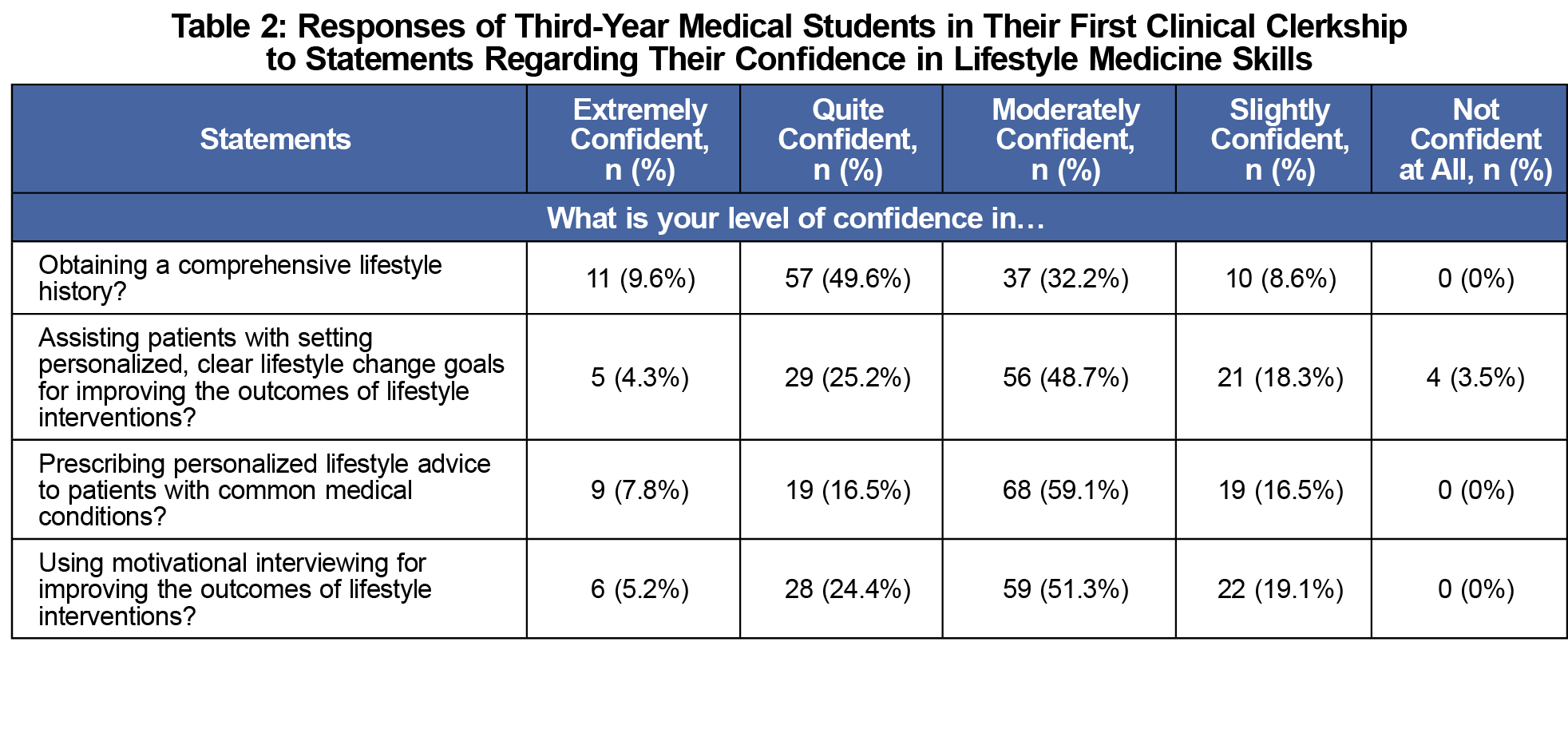
Confidence in Lifestyle Medicine Skills (Table 2)
More than 49% of students reported being confident in obtaining a comprehensive lifestyle history and no student reported being not confident at all; 48.7% of students reported being moderately confident in assisting patients with setting personalized lifestyle goals for improving lifestyle intervention outcomes and only 3.5% of students reported not being confident. More than 59% of students reported being moderately confident in prescribing lifestyle advice to patients and no student reported being not confident at all. Fifty-one percent of students reported being moderately confident in using motivational interviewing to improve lifestyle intervention outcomes and no student reported being not confident at all. Students reported highest confidence in obtaining a comprehensive lifestyle history, with a mean score of 3.6 and a standard deviation of 0.8. Students reported confidence on a Likert scale of 1-5, with 5 meaning they were extremely confident. Students reported lowest confidence in assisting patients with setting personalized lifestyle goals, with a mean score of 3.1 and standard deviation of 0.9 on the same Likert scale.
Our results show that, at the beginning of their clinical training, most third-year medical students understand the value of lifestyle medicine in patient care and want to learn the skills and knowledge involved. However, a small percentage of students are concerned that lifestyle medicine is not a valuable use of limited patient-doctor time, which may limit their interest in learning about lifestyle medicine and their use of lifestyle medicine in their future clinical practice. Interestingly, students rated the value of lifestyle medicine highly. This suggests that current students may work to promote efficient health care systems to make room for lifestyle medicine skills and practices. This is in line with the recommendation of a new health care model from the American Medical Association.11
Students are most confident in their skills for obtaining a comprehensive lifestyle history and least confident in setting clear personalized lifestyle change goals. Students’ lower to moderate confidence in personalized advice, motivational interviewing, and goal setting for lifestyle changes all suggests a high need for educational interventions in these categories. These gaps are similar to those reported by physicians in practice,5, 6, 8 which suggests that educational interventions may also be helpful for physicians already in practice.
Adding elements to an undergraduate medical curriculum that is going through a transformation involving less class time is an extraordinary challenge.12 Therefore, we must find innovative ways to integrate lifestyle medicine into current sessions with maximal curricular efficiency. We specifically encourage integration into the clinical curriculum when students can practice these skills with real patients. As modeling lifestyle medicine skills to trainees at clinical sites is desirable,14 the interventions should include training at clinical sites. Practicing clinical teachers report a lack of confidence in demonstrating these skills due to insufficient practical experience.4,15,16 Therefore, there is also a need for training the trainers so medical students can observe and learn lifestyle medicine skills from competent and confident physician educators. Faculty development interventions will require adequate resources: dedicated time assigned for both the trainer and clinical preceptor and materials for teaching and assessing.
In conclusion, future educational interventions should focus on educating students on setting lifestyle change goals, personalizing prescriptions, and motivational interviewing. The approach and data presented here could be utilized by other institutions seeking to develop or optimize their lifestyle medicine curriculum. Policy makers should use these data as a call to action for generating medical systems to treat the current crisis of unhealthy behaviors.
Acknowledgments
Acknowledgments: The authors thank Mathew Robinson for contributing to the data analysis for this project.
References
- Marrero SL, Bloom DE, Adashi EY. Noncommunicable diseases: a global health crisis in a new world order. JAMA. 2012;307(19):2037-2038. doi:10.1001/jama.2012.3546
- Kaiser AB, Zhang N, Der Pluijm WV. Global prevalence of type 2 diabetes over the next ten years (2018-2028). Diabetes. 2018;67(Supplement 1).
- Ezzati M, Riboli E. Behavioral and dietary risk factors for noncommunicable diseases. N Engl J Med. 2013;369(10):954-964. doi:10.1056/NEJMra1203528
- Lianov L, Johnson M. Physician competencies for prescribing lifestyle medicine. JAMA. 2010;304(2):202-203. doi:10.1001/jama.2010.903
- Foster GD, Wadden TA, Makris AP, et al. Primary care physicians’ attitudes about obesity and its treatment. Obes Res. 2003;11(10):1168-1177. doi:10.1038/oby.2003.161
- Flocke SA, Clark A, Schlessman K, Pomiecko G. Exercise, diet, and weight loss advice in the family medicine outpatient setting. Fam Med. 2005;37(6):415-421.
- Houlden RL, Yen HH, Mirrahimi A. The lifestyle history: a neglected but essential component of the medical history. Am J Lifestyle Med. 2017;12(5):404-411. doi:10.1177/1559827617703045
- Valero-Elizondo J, Aneni EC, Osondu CU, Grandhi GR, Virani SS, Nasir K. Gaps in provider lifestyle counseling and its adherence among obese adults with prediabetes and diabetes in the United States. Prev Med. 2019;129:105815. doi:10.1016/j.ypmed.2019.105815
- Kris-Etherton PM, Akabas SR, Bales CW, et al. The need to advance nutrition education in the training of health care professionals and recommended research to evaluate implementation and effectiveness. Am J Clin Nutr. 2014;99(5)(suppl):1153S-1166S. doi:10.3945/ajcn.113.073502
- Pasarica M, Boring M, Lessans S. Current practices in the instruction of lifestyle medicine in medical curricula. Patient Educ Couns. 2021.
- Trilk J, Nelson L, Briggs A, Muscato D. Including lifestyle medicine in medical education: rationale for American College of Preventive Medicine/American Medical Association Resolution 959. Am J Prev Med. 2019;56(5):e169-e175. doi:10.1016/j.amepre.2018.10.034
- Emanuel EJ. The inevitable reimagining of medical education. JAMA. 2020;323(12):1127-1128. doi:10.1001/jama.2020.1227
- Lessans SP, Kay D. Survey Tool Assessing Proficiency and Confidence of Third Year of Medical Students Regarding Lifestyle Medicine. Society of Teachers of Family Medicine Resource Library. 2022. Accessed May 31, 2022. https://resourcelibrary.stfm.org/viewdocument/survey-tool-assessing-proficiency-a?CommunityKey=2751b51d-483f-45e2-81de-4faced0a290a&tab=librarydocuments
- Pasarica M, Kay D. Teaching evidence-based lifestyle management in family medicine training. Educ Prim Care. 2018;29(1):60-61. doi:10.1080/14739879.2017.1402375
- Rogers LQ, Gutin B, Humphries MC, et al. Evaluation of internal medicine residents as exercise role models and associations with self-reported counseling behavior, confidence, and perceived success. Teach Learn Med. 2006;18(3):215-221. doi:10.1207/s15328015tlm1803_5
- Rogers LQ, Bailey JE, Gutin B, et al. Teaching resident physicians to provide exercise counseling: a needs assessment. Acad Med. 2002;77(8):841-844. doi:10.1097/00001888-200208000-00019



There are no comments for this article.