Introduction: Interprofessional education (IPE) and collaborative practice increasingly inform accreditation standards for pharmacy and medical education, grounded in evidence of benefits to patients and learners. Optimizing models that meaningfully provide this type of practice remains a challenge. This study examines the impact of inpatient collaboration between pharmacy students and family medicine residents on perceptions of interprofessional care.
Methods: Pharmacy students and family medicine residents were invited to participate in an IPE experience during their medicine rotation, in which student-resident pairs worked collaboratively on patient care for a block rotation. We used a Student Perceptions of Physician-Pharmacist Interprofessional Clinical Education Instrument (SPICE-2) survey instrument and included an opportunity for open comments by participants. We performed statistical analysis using paired t tests.
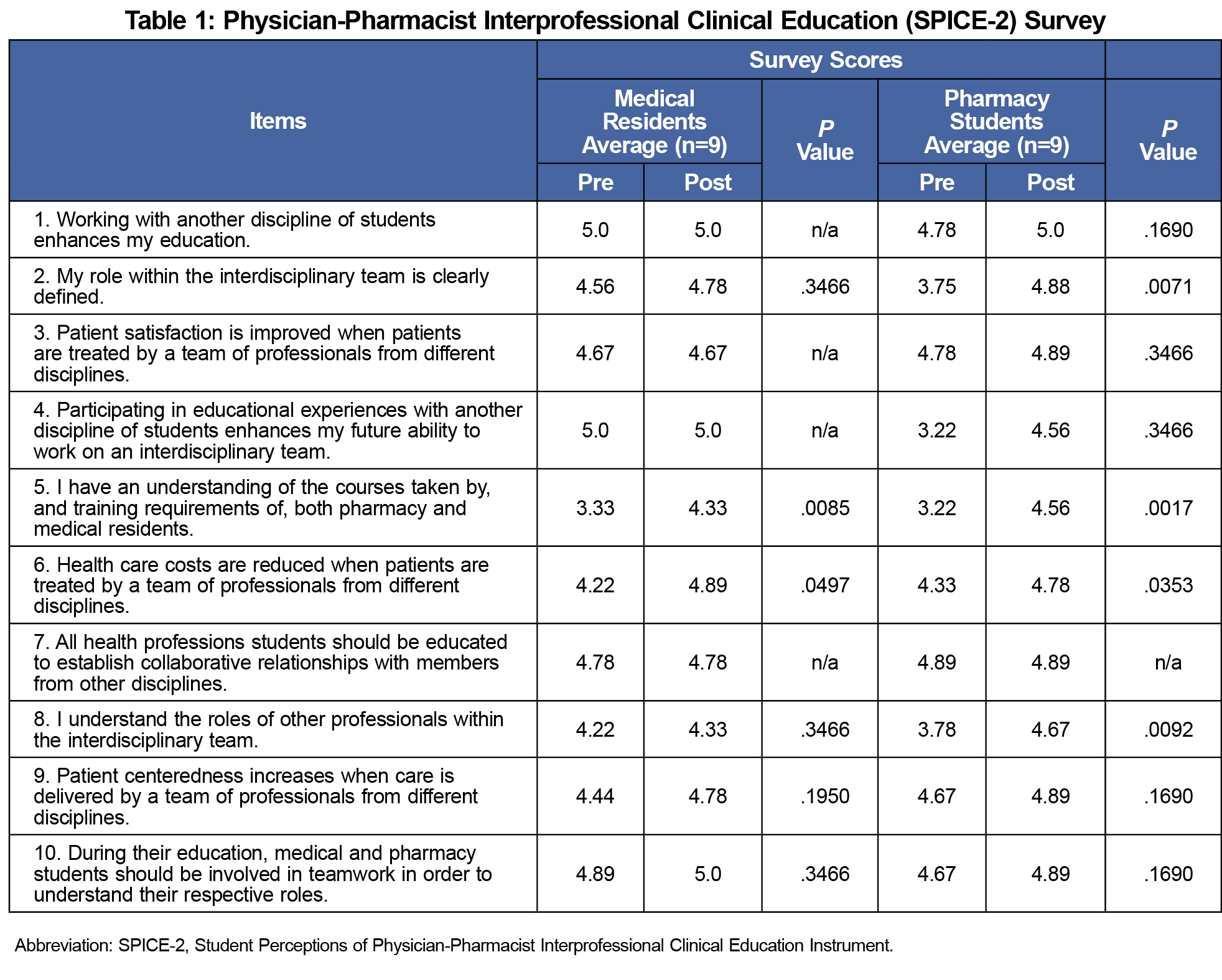
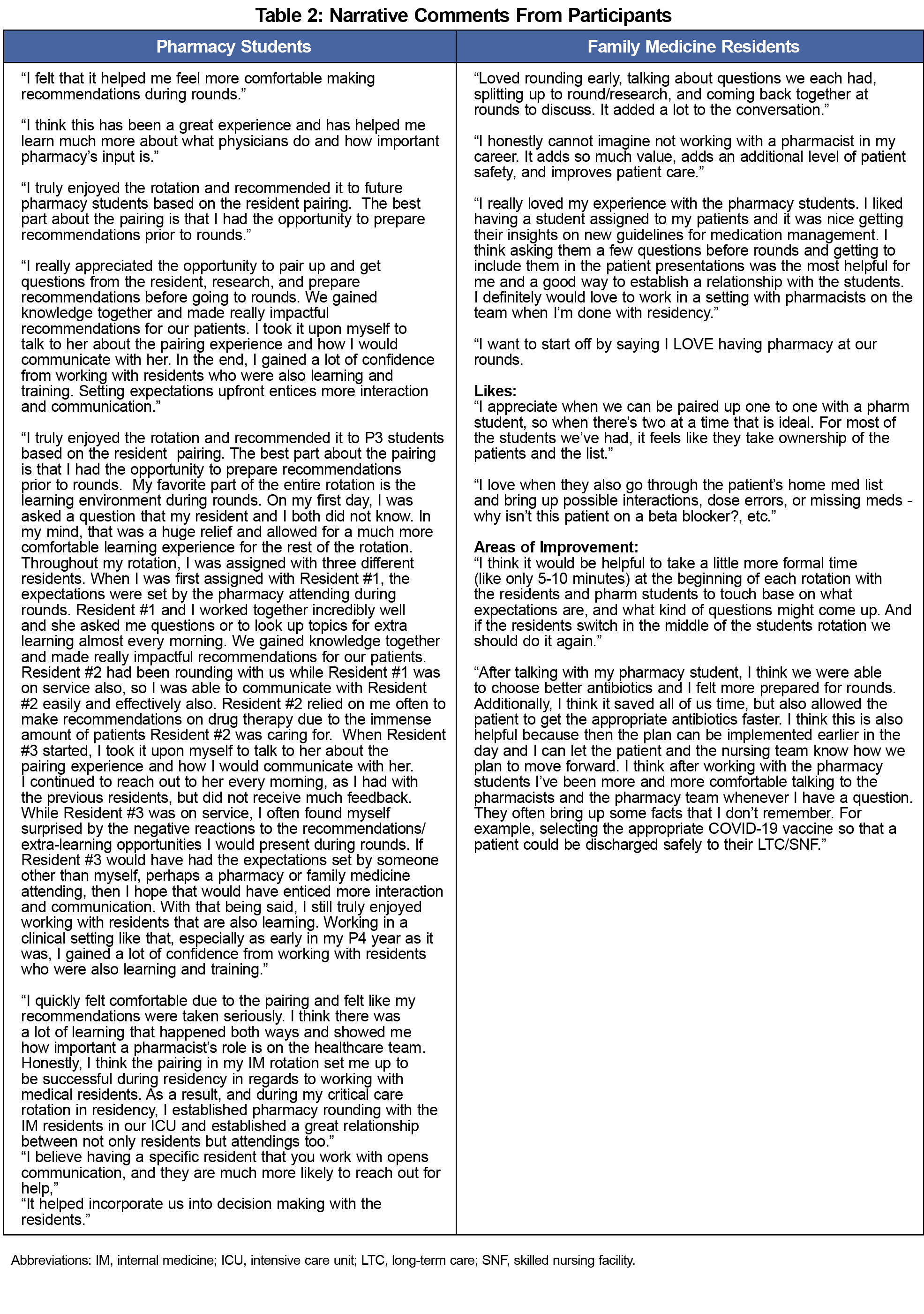
Results: We observed statistically significant changes (P<.05) in four of the 10 survey items for pharmacy students and two out of 10 in family medicine residents. Narrative comments provided by both students and residents were positive regarding the IPE experience.
Conclusion: This pilot provides preliminary evidence to support an IPE care model that integrates pharmacy students by pairing them with family medicine residents on an inpatient adult family medicine teaching service. Implementation of a paired-IPE model changed both professions' perception of their roles within the team and appreciation of training requirements. Larger studies could be done to further evaluate the outcomes of this and similar models.
Patient care continues to trend toward increased collaboration between pharmacists and physicians, with multiple studies demonstrating benefits from physician-pharmacist management of a variety of disease states.1-3 The Accreditation Council for Pharmacy Education (ACPE) and the Accreditation Council for Continuing Medical Education (ACCME) both require interprofessional education (IPE) and collaboration, with the ACPE affirming that “interprofessional interaction is paramount to successful treatment of patients."4,5 Additionally, the Accreditation Council for Graduate Medical Education (ACGME) in Family Medicine (FM) lists interprofessional teamwork as a core measure.6 The challenge, however, lies in creating training experiences where such collaboration is meaningful.7
While some literature has evaluated the use of integrating resident pharmacists into an FM residency site, less is known about integrating pharmacy students.8 In 2016, Kostoff et al placed pharmacy students into an FM residency clinic to examine interprofessional collaboration and satisfaction between pharmacy students (n=52) and medical residents (n=22).9 In the study, perceptions were assessed using the Scale of Attitudes Toward Physician-Pharmacist Collaboration (SATP2C). The researchers noted that pharmacy integration resulted in high levels of collaboration and perceived benefit by medical residents. In a similar approach, Nwaesi et al paired student pharmacists (n=18) and student physicians (n=18) in the inpatient setting with intent to evaluate study participants’ perceptions of the program.10 Student pharmacists and student physicians were involved in both prerounds as well as teaching rounds. Participants were given a pre- and post- Student Perceptions of Physician-Pharmacist Interprofessional Clinical Education Instrument (SPICE-2) survey in order to assess perceptions. Nwaesi et al reported positive changes to interprofessional collaboration and clinical education, despite high baseline IPE exposure.
The objective of our study was to describe and assess the impact of a structured IPE involving pharmacy students and FM residents on an inpatient adult FM teaching service. To our knowledge, this represents the first such investigation aimed at assessing perceptions of interprofessional care.
This prospective study occurred during one academic year at a community hospital and the methods of this pilot received Institutional Review Board exemption by the University of Wyoming as an educational improvement project. Investigators included a faculty pharmacist and faculty physician, both with IPE exposure. Objectives and expectations were communicated verbally and in writing and participation was voluntary.
On the first day, two fourth-year pharmacy students were individually paired with either a postgraduate year-one (PGY-1) or PGY-2 FM resident on a 3 or 4-week adult medicine rotation. Pharmacy students were present at the site 5 days per week, and practiced under the guidance of a pharmacist preceptor. At the beginning of each day, pharmacy students would perform a brief check-in with their resident, after which each independently developed a care plan to be reconciled while rounding with the remainder of the health care team. The interprofessional team was composed of the attending physician, pharmacist preceptor, FM residents, pharmacy students, and one or two registered nurses dedicated to optimizing transitions of care. Other activities included a weekly didactic presentation by the attending physician and a weekly presentation given by the pharmacy students.
To assess baseline perceptions of benefit, participants anonymously completed the SPICE-2 instrument, which contains survey questions based on interprofessional teamwork, roles/responsibilities for collaborative practice, and patient outcomes from professional practice.11,12 While many instruments exist, SPICE-2 has been validated in a diverse population of medical and pharmacy students. SPICE-2 uses a 5-point Likert scale, where 1 is “strongly disagree” and 5 is “strongly agree.” Participants completed the SPICE-2 again at the end of the rotation. Responses were collected by the attending pharmacist. We used GraphPad Prism to perform statistical analysis using paired t tests, with significance level set at P=.05. We also gathered optional narrative comments about the experience from participants.
Nine pharmacy students and nine FM residents completed the SPICE-2 presurvey. Over a single academic year, a total of 18 participants were invited and all 18 participants consented to participate. The pre- and postsurveys were completed by 100% of participants.
Pharmacy students showed a significant increase (P<.05) postexperience in understanding of their role within the team, their role being clearly defined, understanding of the training requirements of both professionals, and the reduction in health care costs when patient care involves a team consisting of different professions (Table 1). FM residents similarly showed significant increases (P<.05) in their understanding of the training requirements and the reduction in health care costs (Table 1). Narrative comments provided a constructive element of the experience (Table 2).
In this study, pharmacy students were paired with FM residents on an inpatient adult FM teaching service. Baseline perceptions from pharmacy students showed some understanding that interprofessional collaboration enhances education and patient-centered care, consistent with other studies on perceptions of IPE.9,10,13 Despite high baseline perceptions from FM residents, significant increases were shared by both groups regarding understanding one another’s education and training, as well as the financial benefits of interdisciplinary teams. Understanding of team roles significantly increased in the pharmacy students, consistent with findings from Nwaesei and colleagues in their study involving pairing pharmacy and medical students,10 as well as others.8,9 This was not seen within the FM residents, which is consistent with other evidence that physicians continue to underestimate the scope of possible pharmacy involvement on teams.14 However, higher IPE exposure in the FM residents may contribute to a lesser degree of change. Given that our narrative comments suggest paired-IPE had a positive impact on this dynamic, future studies could be powered to assess for small changes in these perceptions as well as to further optimize this educational model.
While comments were generally positive, we want to highlight the impact of variation in expectation-setting identified by one pharmacy student. This student experienced different levels of engagement between residents, and attributed this to a lack of clear guidance provided to that resident by a pharmacy or FM attending. This causality cannot be established and this element of the intervention was not being directly studied, but the experience suggests an opportunity for modeling by supervisors. The interprofessional communication involved in expectation setting itself may be responsible for some of the increased understanding and appreciation of the other professional’s role and responsibilities that characterized this pharmacy student’s other interactions.
Our study is limited by small sample size, single community-hospital setting, and lack of comparison group. The FM residents generally held positive perceptions of interactions with pharmacy, possibly influenced by senior residents who have historically worked with pharmacy trainees. This may skew the results to lack a demonstration of a large difference when evaluating the pre- and postsurveys and account for high initial attitudes. While participation was voluntary, FM residents and pharmacy students may have been influenced to participate for fear of retribution if they did not participate, as demonstrated by the 100% participation rate. Finally, the study is at risk of selection bias due to only including pharmacy students and FM residents in a small program with 21 total residents.
This study provides preliminary evidence to support an integrated role for pharmacy students through pairing with medical residents in an inpatient setting. The paired-IPE experience changed both professions’ understanding of training requirements and financial benefits of interdisciplinary management. Positive narrative responses suggest additional benefits may be demonstrable with larger groups or through optimization of the model. Sustained collaboration over time may better educate future physicians and more fundamentally empower pharmacists, leading to improvements in educational experiences, collaborative practice, and patient care.
Acknowledgments
Presentations: This study was presented at the American Society of Health-System Pharmacists National Pharmacy Preceptors Conference, October 2020 (virtual).
References
- Gums TH, Carter BL, Milavetz G, et al. Physician-pharmacist collaborative management of asthma in primary care. Pharmacotherapy. 2014;34(10):1033-1042. doi:10.1002/phar.1468
- Hwang AY, Gums TH, Gums JG. The benefits of physician-pharmacist collaboration. J Fam Pract. 2017;66(12):E1-E8.
- Sisson EM, Dixon DL, Kildow DC, et al. Effectiveness of a pharmacist-physician team-based collaboration to improve long-term blood pressure control at an inner-city safety-net clinic. Pharmacotherapy. 2016;36(3):342-347. doi:10.1002/phar.1710
- Accreditation standards and key elements for the professional program in pharmacy leading to the doctor of pharmacy degree. Accreditation Council for Pharmacy Education. 2015. Accessed November 8, 2020. https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf
- The ACCME Accreditation Requirements. Accreditation Council for Continuing Medical Education. Accessed November 8, 2020. https://www.accme.org/sites/default/files/202004/626_20200430_Accreditation_Requirements.pdf
- Accreditation Council for Graduate Medical Education and American Board of Family Medicine. The Family Medicine Milestone Project. Accessed November 8, 2020. http://www.acgme-nas.org/assets/pdf/Milestones/FamilyMedicineMilestones.pdf
- Murphy JE, Liles AM, Bingham AL, et al. Interprofessional education: Principles and application. An update from the American College of Clinical Pharmacy. J Am Coll Clin Pharm. 2018;1(1):e17-e28. doi:10.1002/jac5.1025
- Lounsbery JL, Moon J, Prasad S. Assessing collaboration between family medicine residents and pharmacy residents during an interprofessional paired visit. Fam Med. 2015;47(5):397-400.
- Kostoff MD, Shin TR. Integration of pharmacy students into family medicine residency clinics. Fam Med. 2016;48(10):805-808.
- Nwaesei AS, Jacob BC, Peasah SK, Perkins JJ, Hogan M. A Structured approach to intentional interprofessional experiential education at a non-academic community hospital. Am J Pharm Educ. 2019;83(9):7365. doi:10.5688/ajpe7365
- Shrader S, Farland MZ, Danielson J, Sicat B, Umland EM. A systematic review of assessment tools measuring interprofessional education outcomes relevant to pharmacy education. Am J Pharm Educ. 2017;81(6):119. doi:10.5688/ajpe816119
- Zorek JA, Fike DS, Eickhoff JC, et al. Refinement and validation of the student perceptions of physician-pharmacist interprofessional clinical education instrument. Am J Pharm Educ. 2016;80(3):47. doi:10.5688/ajpe80347
- Theodorou J, Rotz M, Macphail L, et al. Designing and evaluating an interprofessional practice experience involving dental and pharmacy students. Am J Pharm Educ. 2018;82(6):6298. doi:10.5688/ajpe6298
- Rakvaag H, SØreide GE, Meland E, Kjome RL. Complementing or conflicting? How pharmacists and physicians position the community pharmacist. Pharm Pract (Granada). 2020;18(3):2078. doi:10.18549/PharmPract.2020.3.2078



There are no comments for this article.