Purpose: Research evaluating the well-being of rural family physicians is limited, resulting in minimal understanding of how to prepare family medicine residents to succeed in rural practice postresidency. Our study aimed to investigate factors associated with maintaining wellness within rural family medicine practices and highlight interventions that rural family physicians identify as important to promote wellness among those seeking future employment in rural settings postresidency.
Methods: Forty-eight rural family physicians completed an online survey with qualitative and multiple-choice items including the Mini-Z about physician demographics, burnout, and wellness. We conducted data analysis using NVivo 12 software for qualitative analyses and R 3.6.1 software for descriptive statistics.
Results: The majority of participants reportedly maintained wellness in rural family practice (maintenance of wellness=79.17%; denied burnout=62.26%). Burnout rates were similar to the national burnout rates for family physicians (37.74% vs 46%). Participants identified multiple residency interventions that could be implemented to prepare rural family physicians to succeed.
Conclusions: This study highlights factors that are associated with the maintenance of wellness among rural family physicians. This is the first study to investigate rural family physician perspectives on residency interventions that may have positive outcomes on wellness postresidency.
The percentage of physicians in the United States with at least one symptom of burnout and decreased satisfaction with work-life balance has increased over time.1 This has led to an increase in focus on physician wellness within graduate medical education in order to encourage better physician health and productivity long-term.2,3 As America continues to face a shortage of rural physicians, including family physicians, increased focus on improving rural physician well-being is necessary in order to aid in retention.4,5 The limited research on rural physician wellness has shown that rural physicians often have poorer retention rates which has been attributed in part to lower job satisfaction and increased work hours.6 Unfortunately, there has been minimal research focused on the wellness of rural family physicians or strategies to prepare FM residents to maintain wellness upon entering the workforce in rural settings.6
The American Academy of Family Physicians has called for family medicine residency programs to prepare residents for all aspects of rural practice.7 However, there has continued to be limited research on factors that result in retention and wellness for family physicians choosing to practice in rural settings postresidency. Martini et al reported that around one-third of family medicine residents (27%) report burnout in their review, suggesting that residents may be leaving residency already feeling unwell.8 Our study aimed to investigate factors associated with maintaining wellness within rural family practices and highlight interventions that rural family physicians identify as important to promote wellness among those seeking future employment in rural settings postresidency.
The research study was approved by the Institutional Review Board at Texas A&M University prior to study initiation.
Participants
We identified rural family physicians based on the Health Resources and Services Administration (HRSA) qualifications for rurality.9 We used snowball sampling beginning with alumni and colleagues from the authors’ family medicine residency program along with contacting state academies of family medicine. We excluded individuals from participation based on incomplete survey data or entering a work zip code that was not defined by HRSA qualification for rurality. Seventy-nine participants initiated the survey with 48 participants completing the entire survey (53 participants were included in the assessment of physician burnout based on data completion of those items). See Table 1 for demographic information.
Materials and Design
A 47-item, internet-based survey was developed and administered via Qualtrics (Qualtrics, Provo, UT).
Demographic Items. The survey’s demographic questions included income, age, sex, religion, children, marital status, and zip code (for the purposes of ensuring rurality within the Federal Office of Rural Health Policy framework). Additional questions were related to work-life balance and employment characteristics.
Mini-Z. The Mini-Z consists of 11 items assessing burnout including individual and systemic factors that contribute to decreased well-being.10 The Mini-Z has been validated internally, with an overall Cronbach α of 0.8, and externally for overall ability to measure stress and predict burnout.10-12 Nine of the 11 items (excluding the atmosphere at work item and free response of stressors items) were chosen from the Mini-Z for the survey in the present study due to brevity in measuring burnout.11 We used the single item regarding defining burnout from the Mini-Z to report burnout among participants.
Residency/Postresidency Well-being Items. The survey also included free-text response items (eg, items related to stressors, personal strategies for maintaining wellness, and job satisfaction during and postresidency) and two binary items evaluating residency involvement in well-being. We also included a rank-order item that assessed rural family physicians’ subjective importance of various residency wellness initiatives, identified through a review of the wellness literature, in preparing resident physicians to maintain wellness postresidency in rural practices.
Data Analysis. We used NVivo 12 software (QSR International, Cambridge, MA) for both an automated and manual content analysis for common thematic elements in the free-text response items in a process adapted from Zhang and Wildemuth to include NVivo 12’s automated capabilities.13 Two of the authors reviewed the automated content analysis. One author performed an independent manual content analysis that was reviewed by a second author for confirmation of content themes. We used R sofware version 3.6.1 for all descriptive statistics of the multiple-choice responses.
The majority of participants did not report burnout (62.26%). Most participants reported maintaining wellness postresidency (79.17%).
Reported Methods for Maintaining Wellness
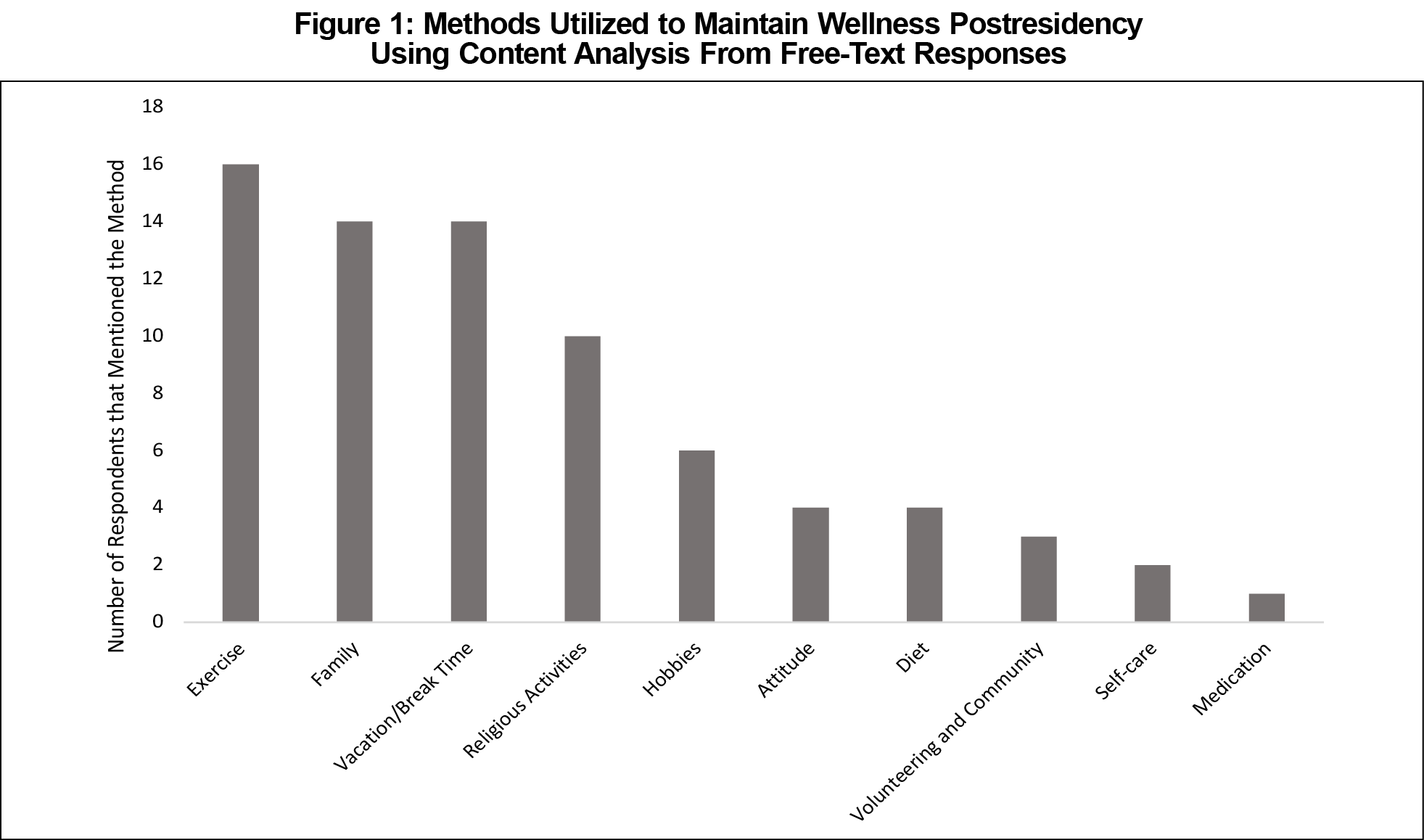
The reported methods employed for wellness maintenance are shown in Figure 1.
Residency Program Interventions for Maintaining Wellness Postresidency
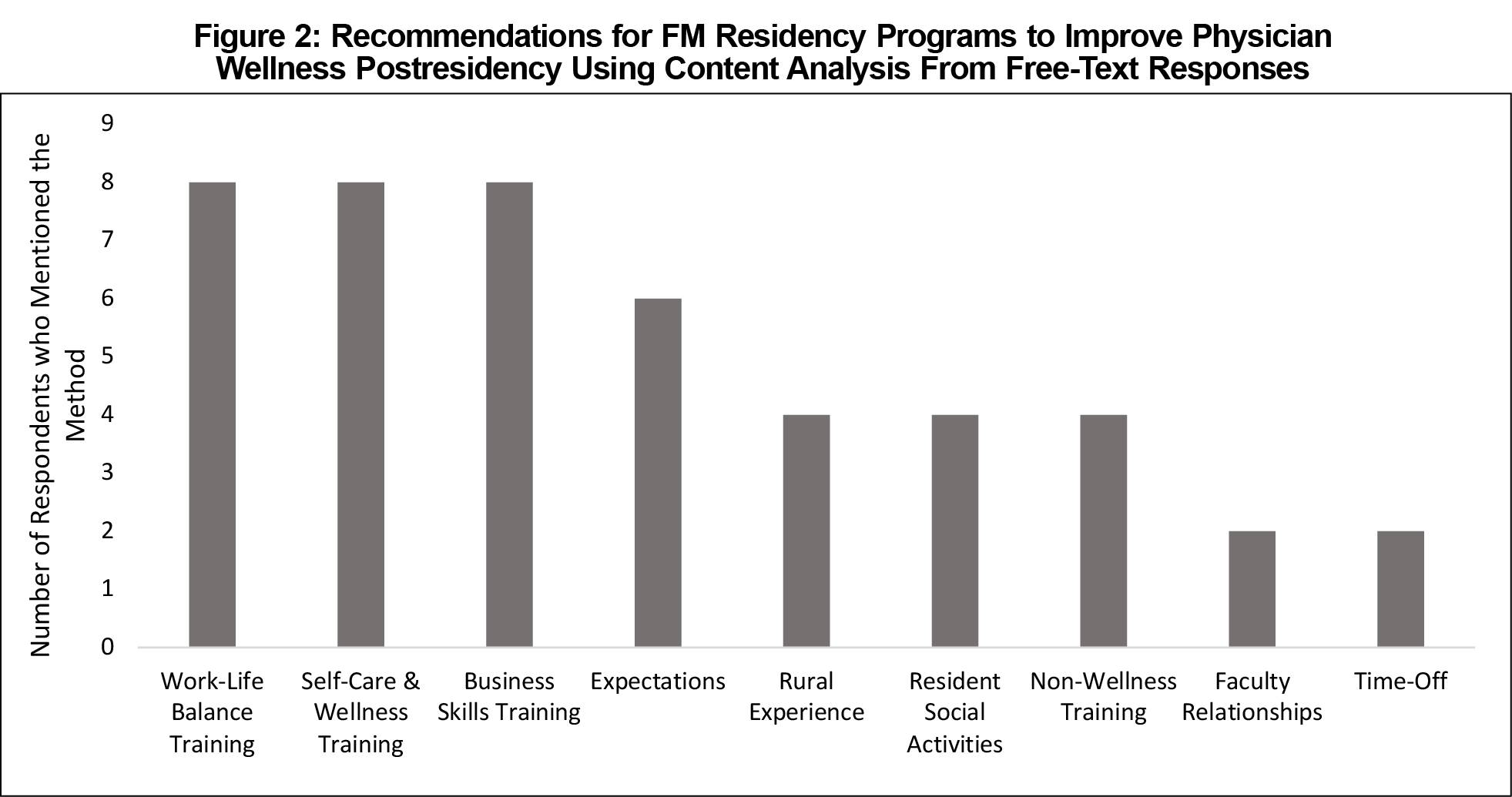
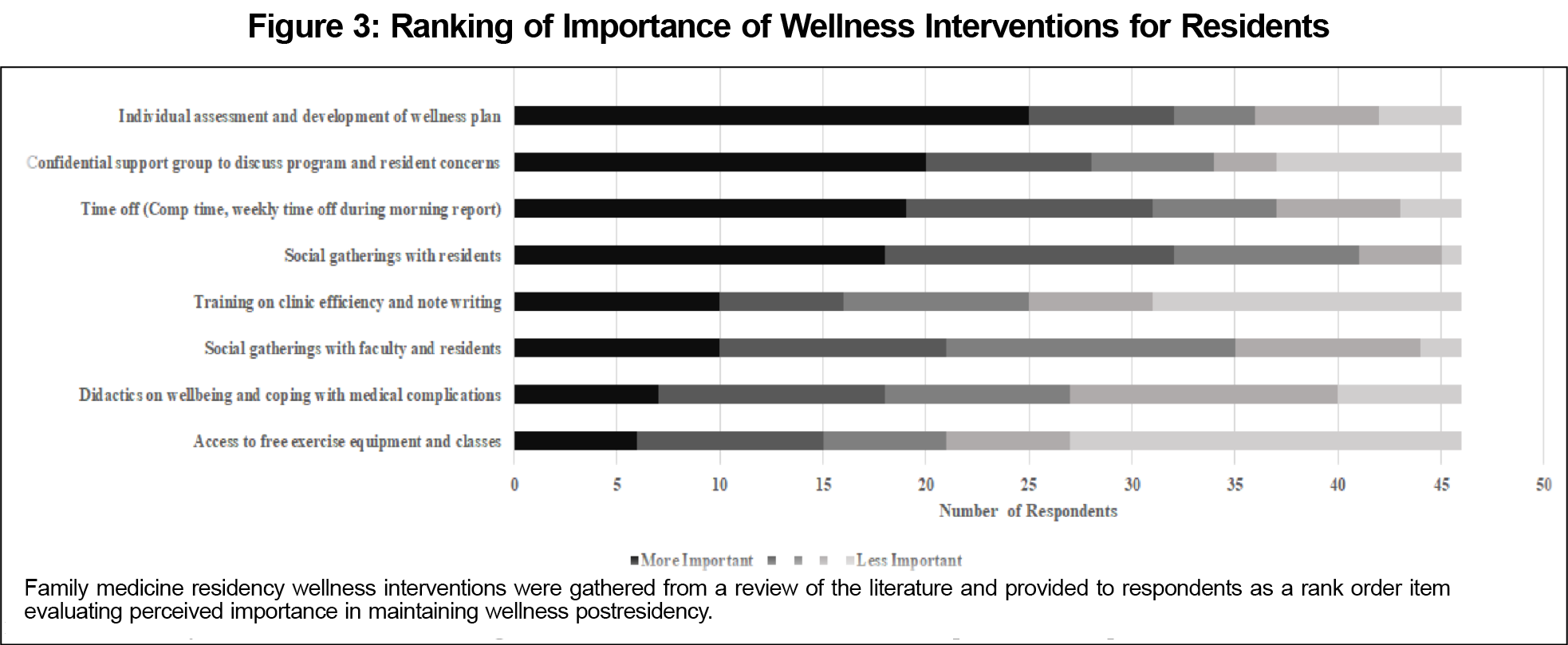
Most participants (95.8%) endorsed a belief that there is a role for residency programs to prepare family physicians to maintain satisfaction and/or well-being with their jobs in rural practice. See Figure 2 (qualitative responses) and Figure 3 (rank-order item of wellness interventions) for recommendations for residency programs.
The rural family physicians sampled in the current study had similar levels of burnout compared to a larger sample of family physicians.14 In one large-scale, cross-sectional survey conducted by the American Medical Association in collaboration with Stanford University School of Medicine and the Mayo Clinic, 46% of family physicians reported experiencing burnout, compared to 37% in the present sample.14 Further, the majority of the sample in our study reported the ability to maintain wellness during their tenure in the rural locations.
The results suggest that family physicians who completed this survey believe family medicine residency programs have a potential role in preparing family physicians for rural practice. The majority of participants (95.8%) reported beliefs that residency programs should be involved with preparing family physicians for rural practice. Participants provided numerous strategies for residency programs to aid their graduating residents’ success postresidency.
The primary limitation of our study is generalizability due to the small sample size, homogeneity of the sample, inability to determine response rate, and potential selection bias. Future research expanding the population of our study could also allow for tests of statistical significance that may enhance the current findings. Overall, our study suggests that family physicians can maintain a sense of wellbeing in rural locations. The responses of family physicians in rural settings from the present study provide preliminary support that family medicine residency programs may be able to play a role in preparing physicians to maintain wellness while meeting the ever-growing demand for rural service delivery across the country. Future research expanding the results of this study could benefit the field as family medicine residency programs prepare future generations of rural physicians to maintain well-being postresidency.
Acknowledgments
The authors thank the Society of Teachers of Family Medicine’s Behavioral Science/Family Systems Educator Fellowship Steering Committee, small group mentors, and 2019-2020 fellows for their guidance and encouragement in the development of this research endeavor as part of the fellowship program.
Presentations: The content of the article was presented at the 2020 STFM Annual Conference, August 2020 (virtual).
References
- Shanafelt TD, Hasan O, Dyrbye LN, et al. Changes in burnout and satisfaction with work-life balance in physicians and the general US working population between 2011 and 2014. Mayo Clin Proc. 2015;90(12):1600-1613. doi:10.1016/j.mayocp.2015.08.023
- Buck K, Williamson M, Ogbeide S, Norberg B. Family physician burnout and resilience: A cross-sectional analysis. Fam Med. 2019;51(8):657-663. doi:10.22454/FamMed.2019.424025
- Noori S, Blood AG, Meleca J, Kennedy V, Engupta D. Current directions in medical student well-being. Col Med Rev. 2017;1(2).
- Rosenblatt RA, Hart LG. Physicians and rural America. West J Med. 1136;2000;173(5):348-351:348. doi:10.1136/ewjm.173.5.348
- Bodenheimer T, Pham HH. Primary care: current problems and proposed solutions. Health Aff (Millwood). 2010;29(5):799-805. doi:10.1377/hlthaff.2010.0026
- Haggerty TS, Fields SA, Selby-Nelson EM, Foley KP, Shrader CD. Physician wellness in rural America: a review. Int J Psychiatry Med. 2013;46(3):303-313. doi:10.2190/PM.46.3.e
- Rural practice, keeping physicians in (position paper). American Academy of Family Physicians. Accessed December 2, 2020. https://www.aafp.org/about/policies/all/rural-practice-keeping-physicians.html
- Martini S, Arfken CL, Churchill A, Balon R. Burnout comparison among residents in different medical specialties. Acad Psychiatry. 2004;28(3):240-242. doi:10.1176/appi.ap.28.3.240
- Federal Office of Rural Health Policy (FORHP) Data Files. US Health Resources & Services Administration. Published April 28, 2017. Accessed January 13, 2022. https://www.hrsa.gov/rural-health/about-us/definition/datafiles.html
- Linzer M, Poplau S, Babbott S, et al. Worklife and wellness in academic general internal medicine: results from a national survey. J Gen Intern Med. 2016;31(9):1004-1010. doi:10.1007/s11606-016-3720-4
- Linzer M, Visser MR, Oort FJ, Smets EM, McMurray JE, de Haes HC; Society of General Internal Medicine (SGIM) Career Satisfaction Study Group (CSSG). Predicting and preventing physician burnout: results from the United States and the Netherlands. Am J Med. 2001;111(2):170-175. doi:10.1016/S0002-9343(01)00814-2
- Shimotsu S, Poplau S, Linzer M. Validation of a brief clinician survey to reduce clinician burnout.J Gen Int Med. 2015;30(Supplement).
- Zhang Y, Wildemuth BM. Qualitative analysis of content. Accessed January 13, 2022. https://www.ischool.utexas.edu/~yanz/Content_analysis.pdf
- Shanafelt TD, Sinsky C, Dyrbye LN, Trockel M, West CP. Burnout among physicians compared with individuals with a professional or doctoral degree in a field outside of medicine. Mayo Clin Proc. 2019;94(3):549-551. doi:10.1016/j.mayocp.2018.11.035




There are no comments for this article.