Objective: We sought to explore whether obstetrics and gynecology (Ob-Gyn) ambulatory clinic preceptors can maintain their clinical productivity with a learner (medical student) present.
Methods: We studied the productivity of five exemplary Ob-Gyn faculty over the 2016-2017 academic year. We used paired two-tailed t tests to compare physician productivity with and without a student. Faculty were interviewed and qualitative analyses were performed on faculty interview data to identify themes used to create sample best-practice workflows for student involvement in the clinic.
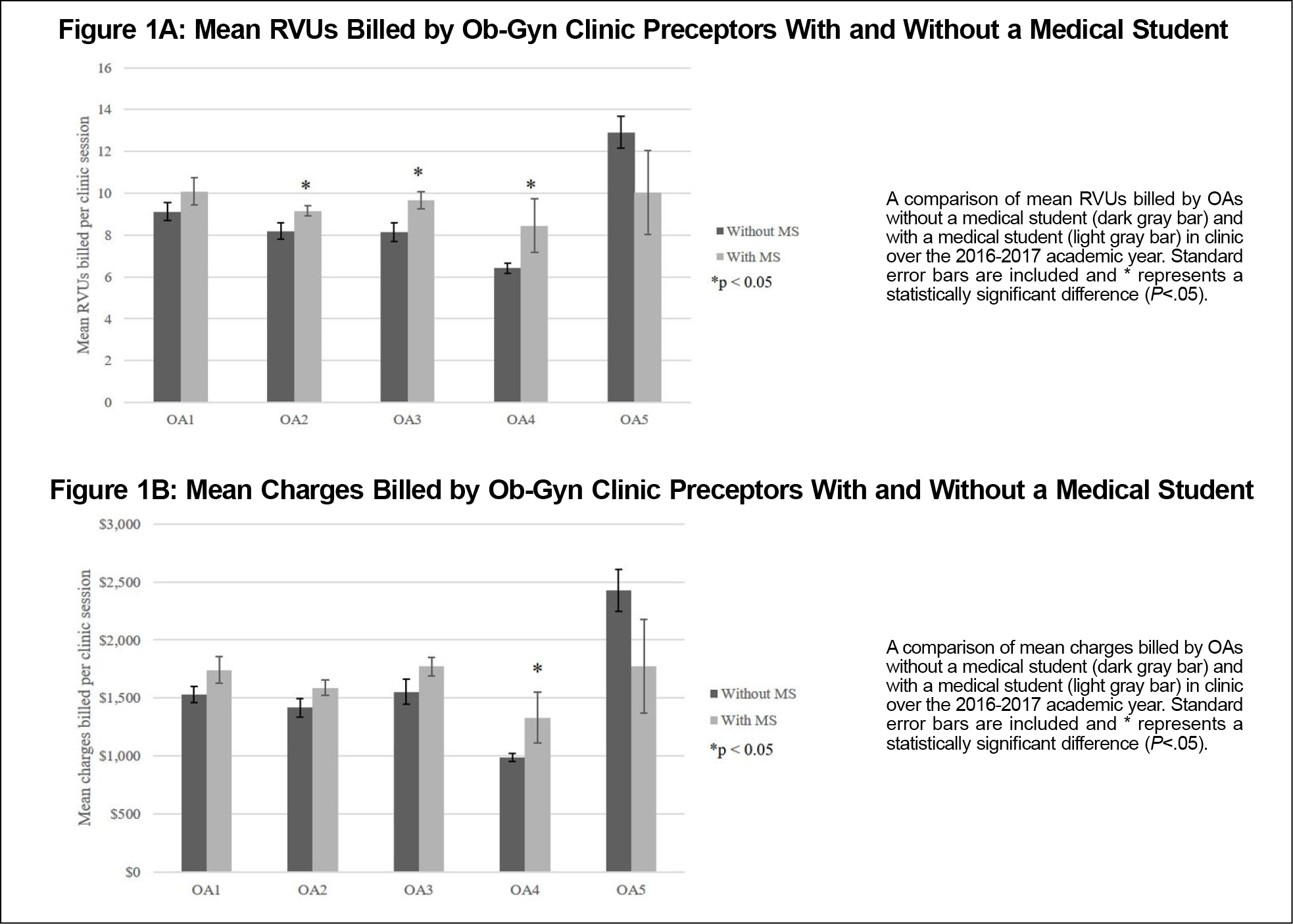
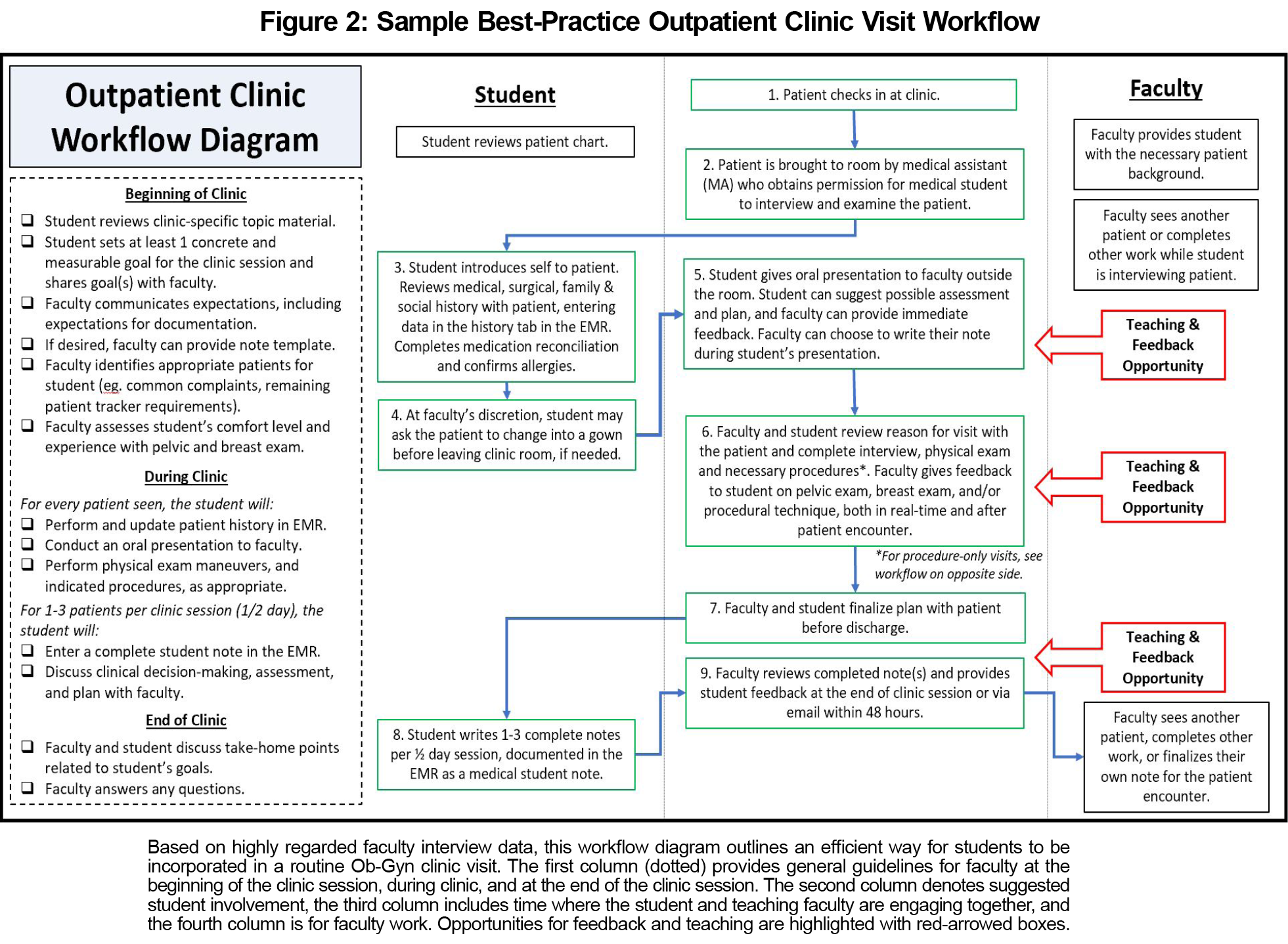
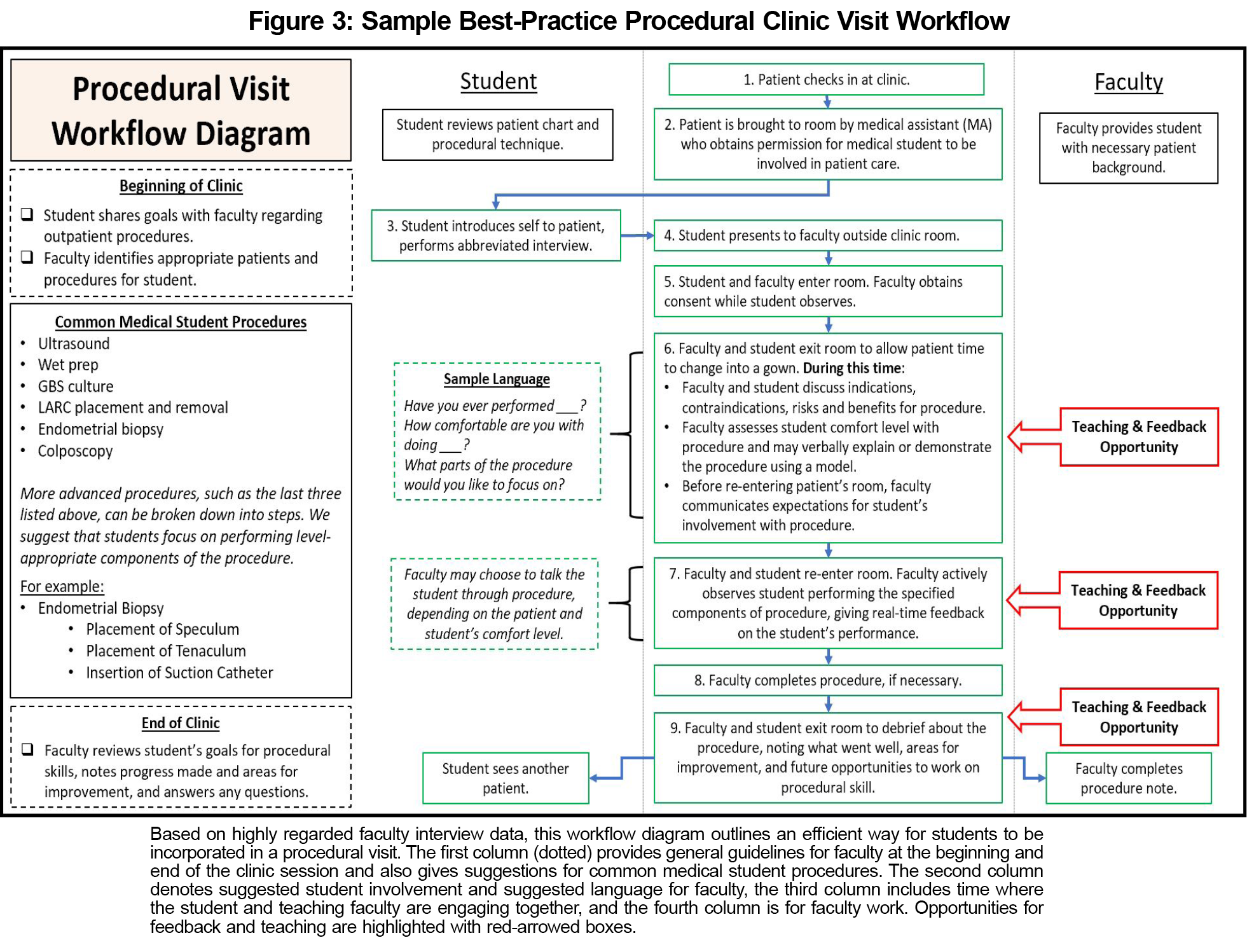
Results: Three faculty had significant increases in relative value units (RVUs) per clinic half-day when a medical student was present (11%-31% increase, P<.05). Four faculty had average increases in net charges billed per clinic half-day ranging from $172.39 to $343.14. One faculty preceptor had a decrease in RVUs and charges billed when a student was present, which was not statistically significant. Themes derived from faculty interviews regarding their incorporation of medical students in the clinic included setting expectations, allowing students to assist with clinic workflow, note-writing, and efficient use of time and clinic space. In an iterative feedback process, we developed ideal workflow models for student involvement during clinic visits with and without a procedure.
Conclusion: This mixed-methods pilot study suggests that medical students do not impede clinician productivity when utilized effectively in the outpatient setting. Further contemporary research is needed to assess the impact of learners on ambulatory clinician productivity in light of Medicare policy changes and modifications in medical education due to the COVID-19 pandemic.
Exposure to primary care through the ambulatory clinic is a required and essential component of medical education. In order to provide these experiences to medical students, busy outpatient faculty are tasked with maintaining their clinical productivity while simultaneously incorporating the student’s learning into their daily workflow.1 This can be especially challenging in the Ob-Gyn clinic due to its high volume of outpatient procedures and new physical exam techniques.
Research in the fields of neurology and emergency medicine suggest that it is possible to maintain financial productivity while being an excellent clinical teacher.2,3 This has not yet been studied in a primary care setting. Our study compared the financial productivity of Ob-Gyn clinic preceptors with and without the presence of a medical student. We hypothesized that skilled Ob-Gyn clinician educators would have similar techniques to incorporate learners in clinic and would be able to maintain financial productivity.
I. Calculating Faculty Productivity With and Without a Medical Student
We examined the productivity of five Ob-Gyn star clinic preceptors, who scored well on end-of-clerkship evaluations completed by medical students. Clinic schedules were not modified based on whether a medical student would be present.
As a proxy for financial productivity, we examined work relative value units (RVUs) and net charges in dollars on clinic days with and without a medical student. Ob-Gyn department financial analysts provided data from the 2016-2017 academic year (September 1, 2016-May 26, 2017). Work RVUs (herein denoted as “RVUs”) provide a standard for clinical services by which reimbursements are based, depending on the time, resources, and skill needed to complete a task.4,5
We used paired two-tailed t tests to calculate whether differences in clinician productivity on clinic days with and without a medical student were statistically significant (defined by P<.05). This study was determined by our institutional review board to be exempt from review.
II. Developing a Best Practice Model for Incorporating Students Into Clinic
We purposively chose to interview five highly-rated Ob-Gyn clinician-educators. We sought to identify their best practices for involving a medical student in the ambulatory setting. Each faculty member was asked five open-ended questions (see Supplementary Figure).
Coding of the interview data was performed independently by two study team members (S.W.Z. and S.P.) using the grounded theory approach to identify themes. Initial codes were compared and discrepancies were resolved. Potential best-practice clinic workflows were then created based on these themes (Figures 2 and 3). Workflows were reviewed by each of the five faculty in an iterative process until the entire group was in consensus with the proposed workflows.
I. Faculty Productivity With and Without a Medical Student
The five Ob-Gyn faculty preceptors (denoted as OA1-5) included in this part of the study were generalists. Faculty had 7-38 clinic half-day sessions with medical students (ranging from 13.2% to 60.7% of total clinic sessions, Table 1). They saw similar numbers of patients per session regardless of whether a medical student was present, except for OA3, who saw on average 0.9 more patients per clinic session with a student (P<.05).
Three out of five faculty had significantly greater mean RVUs billed per clinic session with a medical student, ranging from 11.78% to 31.73%, or an additional 1 to 2.1 work RVUS (Figure 1A). Charges mirrored the trend of RVUs; however, only one faculty preceptor, OA4, had a statistically significant increase in net charges when a student was present (Figure 1B). One faculty preceptor (OA5) had nonsignificant decreases in both productivity metrics when a medical student was present (22.29% decrease in RVUs, $655.55 decrease mean charge per half-day; P=.171 and .185).
II. Best Practices for Incorporating Students Into Clinic
Individual interviews with the five Ob-Gyn faculty yielded multiple themes and were used to design sample, best-practice clinic workflows (Figures 2 and 3):
- Incorporating the student in clinic (identified in four out of five faculty interviews): Medical students were introduced to clinic staff at the start of the clinic session. Medical assistants were asked to inquire whether patients felt comfortable having a student see them.
- Students assist in clinic workflow (identified in three out of five faculty interviews): Students were recommended to have patients change into a gown after interviewing them, as it both “sets expectations that the medical student will be doing the [pelvic] exam” and assisted with clinic workflow.
- “See one, do one” (identified in three out of five faculty interviews): Most faculty practiced the “see one, do one” technique for teaching procedures, where they first had a medical student observe them performing the procedure on a patient. The two faculty who did not practice the “see one, do one” technique explained and demonstrated the procedure outside the patient room, prior to allowing the student to perform it.
- Note-writing expectations (identified in four out of five faculty interviews): Faculty asked students to write notes on only one to three patients per clinic half-day session, and the majority recommended students to document directly in the electronic medical record (EMR).
- Efficient time/space use (identified in five out of five faculty interviews): Faculty described using a second room to see other patients while the student was with a patient or using the time to complete notes and inbox tasks.
This small, mixed-methods study suggests that medical students do not impede outpatient Ob-Gyn clinician productivity when utilized effectively. Our research is consistent with previous work that describes associations between higher faculty clinical productivity and superior teaching scores among trainees.2,3 We surmise that Ob-Gyn faculty were able to bill more RVUs with a medical student present because they had more complete history data to allow for appropriate coding of clinic encounters and increased billable counseling. Only one provider (OA3) saw a significantly greater number of patients when a medical student was present. In this case, higher clinician productivity may have resulted from easier accommodation of add-on and/or late patients. For the two out of three faculty who had statistically-significant increases in RVUs billed per clinic session but did not have significant increases in net medical charges per clinic session, we suspect that the discrepancy is due to the bundled payment model of reimbursement for key areas of episodic Ob-Gyn care (eg, prenatal care).
Since March 5, 2018, the Centers of Medicaid and Medicare Services (CMS) allowed for teaching physicians to verify any student documentation of the “physical exam and medical decision-making activities” of the service being billed without needing to redocument for the purpose of reimbursement.6 This policy change greatly expanded medical students’ capacity to document in the EMR, adding value to their role in primary care settings. One of the limitations of our study is the use of older data, which does not reflect the positive impact of the CMS policy change or the negative effect of the COVID-19 pandemic on student learners in the clinic. Our results are also limited in generalizability due to inclusion of a small number of faculty at a single institution over 1 academic year. The strength of this study is its mixed-methods approach with a qualitative thematic analysis that generated proposed clinic workflows both for procedural and nonprocedural outpatient visits. Future research should include a larger number of preceptors over a longer time frame, as well as examine the effect of medical students on other measures of outpatient clinician productivity, such as preceptor work after clinic time and time to note closure.
Acknowledgments
Acknowledgments: The authors acknowledge the assistance of Maryana Townsend, Ob-Gyn department administrator, in obtaining faculty schedules and productivity metric data, and the assistance of of Rebecca Slattery, Ob-Gyn clerkship manager, in obtaining medical student schedules. They also thank Dr Orlando Valle for his assistance with data collection and interviews.
References
- Christner JG, Dallaghan GB, Briscoe G, et al. The community preceptor crisis: recruiting and retaining community-based faculty to teach medical students-a shared perspective from the Alliance for Clinical Education. Teach Learn Med. 2016;28(3):329-336. doi:10.1080/10401334.2016.1152899
- Hemphill RR, Heavrin BS, Lesnick J, Santen SA. Those who can, do and they teach too: faculty clinical productivity and teaching. West J Emerg Med. 2011;12(2):254-257.
- Tanner JA, Rao KT, Salas RE, et al. Incorporating students into clinic may be associated with both improved clinical productivity and educational value. Neurol Clin Pract. 2017;7(6):474-482. doi:10.1212/CPJ.0000000000000394
- Jacobs JP, Lahey SJ, Nichols FC, et al; Society of Thoracic Surgeons Workforce on Coding and Reimbursement. How is physician work valued? Ann Thorac Surg. 2017;103(2):373-380. doi:10.1016/j.athoracsur.2016.11.059
- Beck DE, Margolin DA. Physician coding and reimbursement. Ochsner J. 2007;7(1):8-15.
- CMS Medicare Learning Network. Guidelines for Teaching Physicians, Interns, and Residents. Centers for Medicare and Medicaid Services. Accessed October 2021. https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/teaching-physicians-fact-sheet-icn006437.pdf