Objectives: We sought to assess self-care perception consistency between patients with type 2 diabetes mellitus and their physicians and characterize the psychosocial parameters influencing their respective perceptions.
Methods: We conducted a study of 627 patients with type 2 diabetes and their physicians throughout 12 family medicine residency clinics in Texas to analyze their respective perceptions of patient self-care. We utilized linear regression testing.
Results: There was a lack of consistency in self-care perception between patients and physicians 31.2% of the time. Patient self-care perception was best predicted by the patients’ diabetes distress scores (P<.001) and last HbA1c (P<.001).
Conclusion: Measuring a patient’s diabetes distress may help physicians better understand a patient’s self-care perception. By understanding a patient’s self-care perception, the physician may be able to explore these notions of positive or negative self-care perception and even gently correct them when necessary. This may allow physicians to better align themselves with the patient, provide behavioral health interventions, and better target and communicate effective plans.
Practical Implications: We suggest periodic assessment of diabetes distress and self-care perception to inform the need for education to improve self-efficacy.
Managing type 2 diabetes (T2D) relies heavily on patient self-care behaviors that are associated with better glycemic control.1 Self-efficacy is defined as a patient’s self-recognized capacity to positively impact their health through actions.2-4 As self-efficacy is malleable, proposed interventions for treatment of T2D have included behavioral approaches to develop more favorable patient illness perceptions.5,6 Effective patient-physician relationships are associated with more positive patient illness perceptions.7 Therefore, we postulate that if both patients and physicians share similar perceptions of the success of the patient’s self-care, they will be better aligned to collaboratively create an optimal care plan.
To understand the patient-physician relationship in the context of T2D self-care, we conducted a study of patients with T2D and their physicians to assess their respective perceptions and resulting concordance of patient self-care. We further define this concordance as “Self-care Perception Consistency.” The purpose of this study is to understand how consistent patient and physician perceptions of patient self-care are in primary care settings.
Design
This study utilized a cross-sectional design using survey data collected by the Residency Research Network of Texas (RRNeT). RRNeT is a practice-based research network comprised of 12 family medicine departments across rural, urban, and suburban Texas.
Data were collected through a 71-item survey administered at nine RRNET-participating family medicine residency clinics. Inclusion criteria were a history of T2D and age between 18 years and 75 years. The survey was completed by the patient or administered to the patient in either English or Spanish. A total of 627 people completed all or part of the survey; 78 surveys were excluded because of failure to meet inclusion criteria. An additional 15 surveys were excluded because the patient did not answer the patient self-care question, leaving 534 surveys. Conversely, only 311 analogous physician surveys of comparison were completed. For general analysis, 534 patient surveys were utilized; for analysis requiring both patient and physician surveys, 311 patient-physician pairs surveys of comparison were used.
Information was collected on social determinants of health, quality-of-life, and diabetes distress to understand a patient’s psychosocial status. Questions were adapted from validated surveys.8-10 Analogous questions were designed for a shorter, 10-item physician survey to determine the physician’s perceptions of the patient’s socioeconomic status. The study was approved by the Institutional Review Board at each site where the research was performed.
Measures
Patients and physicians were asked to rate a patient’s self-care using a 4-point Likert scale-based response including “Poor,” “Kind of poor,” “Okay,” or “Great.” These responses were further dichotomized with the positive responses (Great, Okay) and the negative responses (Poor, Kind of poor). If patient and physician selections were both positive or both negative, a separate variable consistency was given a value of 1, otherwise, 0. Consistency was used to delineate subgroups analysis.
Scores were created to characterize the views of patients and their physicians. These included a modified Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE) score to assess social determinants of health, a quality-of-life score (ADDQoL), a modified diabetes distress score (DDS-17), and a physician survey score.8,9,10 The diabetes distress score was modified to reduce the 6-point Likert scale to a 4-point scale.9
The higher the quality-of-life score, the better quality-of-life the patient perceives; similarly, higher diabetes distress scores indicated more patient distress with T2D. Higher partial PRAPARE score indicate that the patient contends with more adverse social determinants of health. The 10-question physician survey was partially used to create the “physician score” referenced throughout this paper. The lower the physician score, the more disadvantaged the physician felt the patient to be.
We performed analysis using RStudio Desktop (v1.1.463); We considered P-values significant at <0.05. We used multivariate linear regression for analysis.
Self-care Perception Consistency
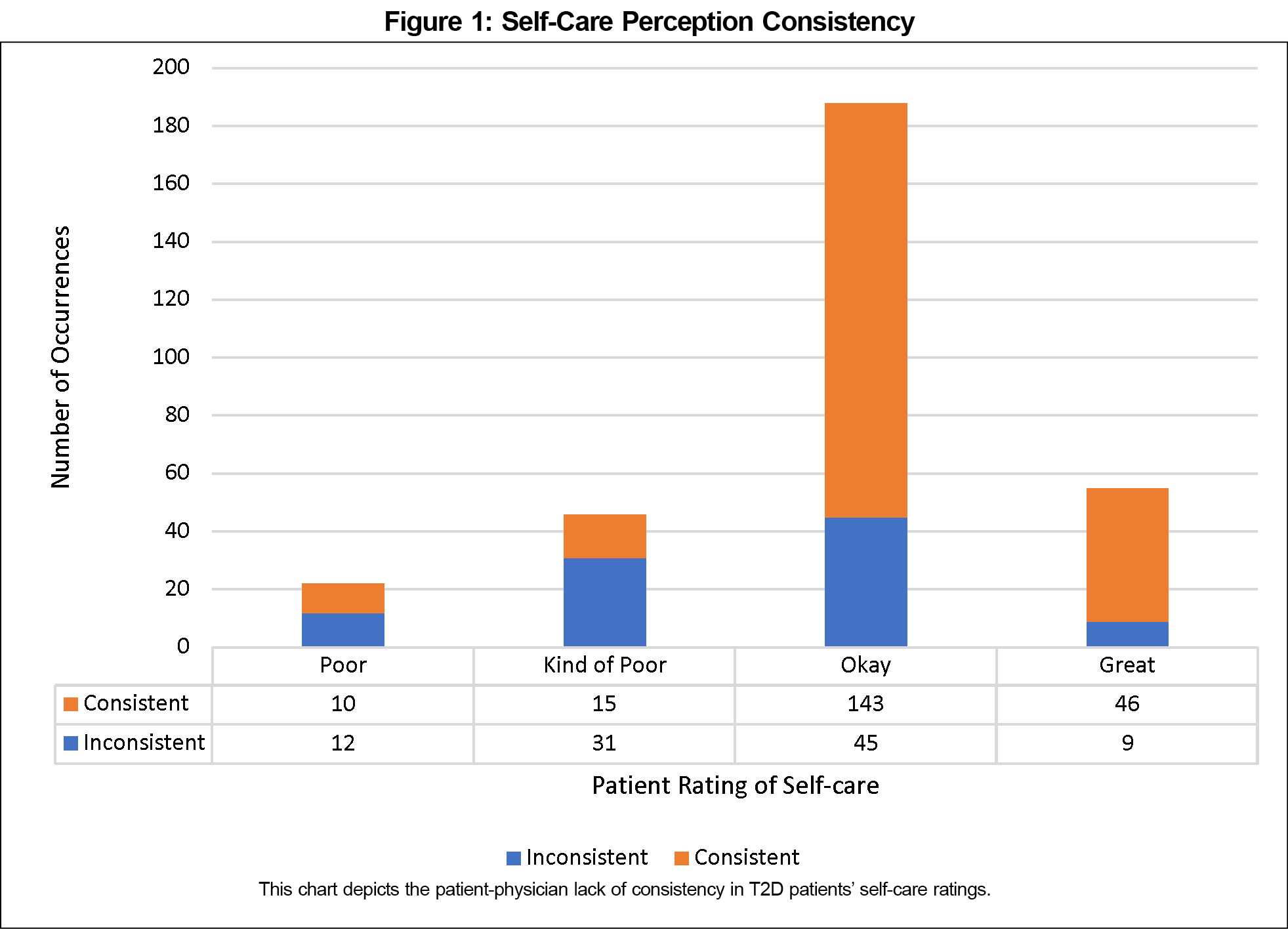
To characterize patient and physician perceptions of a patient’s self-care, the variable, consistency, was utilized. Patients and physicians were inconsistent in their perception of patient self-care 31.2% of the time (Figure 1).
Assessing Psychosocial Parameters and Patient Self-care Perception
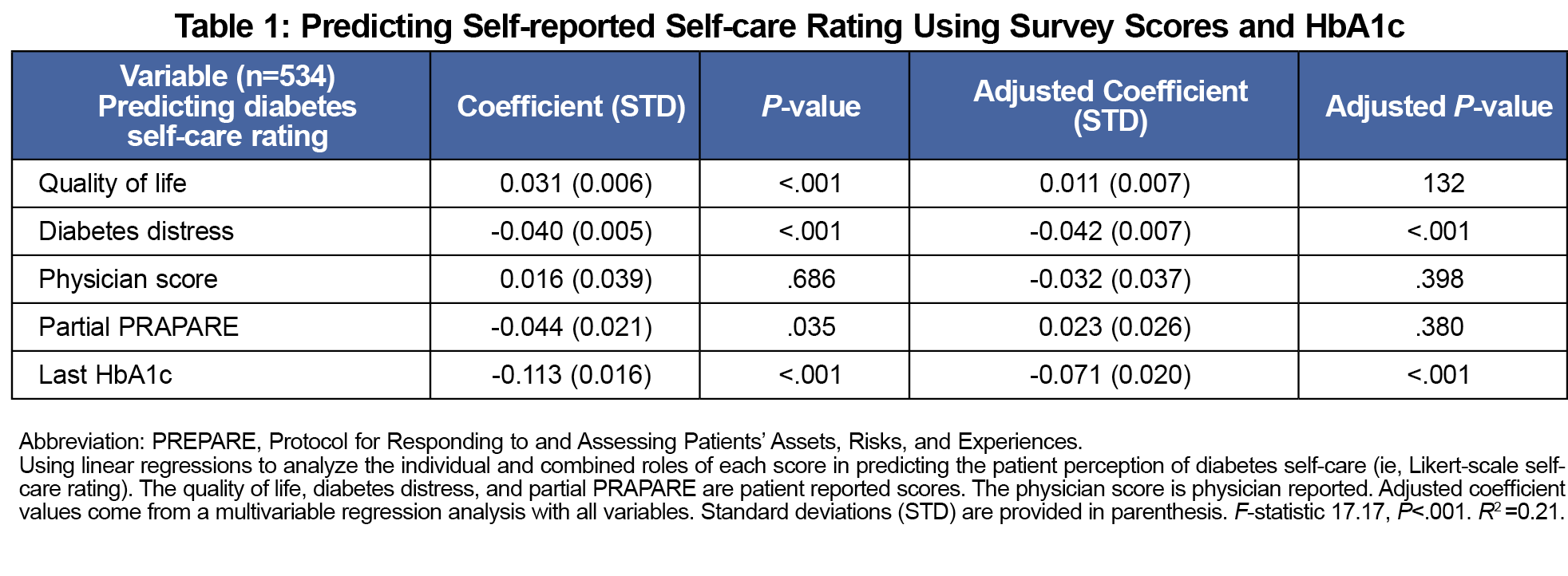
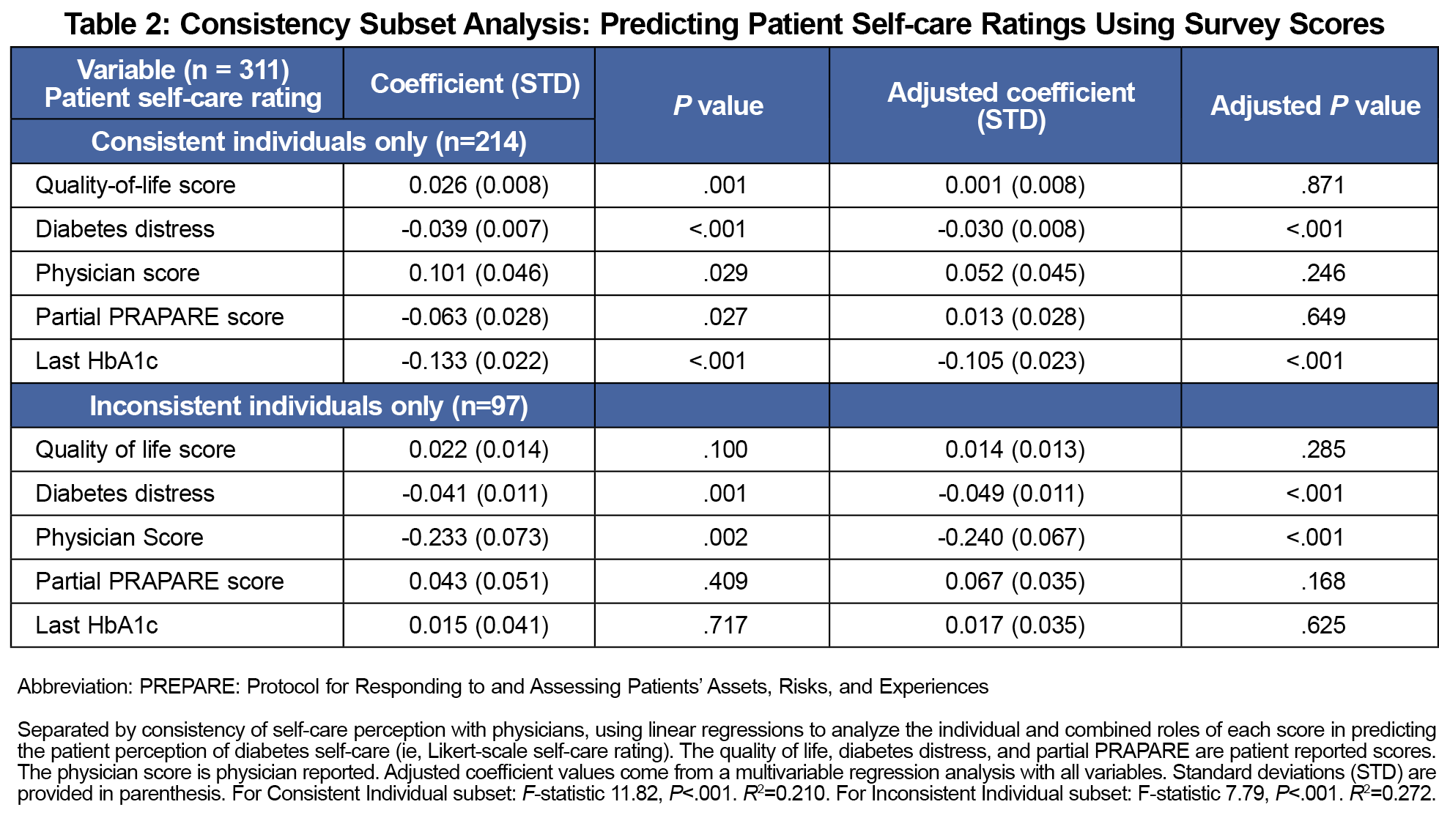
Next, the effects of psychosocial parameters on self-care rating were assessed using the quality-of-life, diabetes distress, physician, and partial PRAPARE scores. We used linear models to investigate the association between the scores and the patient self-care ratings. The best predictors of patient self-care rating (Table 1) were the self-reported diabetes distress score (P<.001) and the last HbA1c value (P<.001). To better characterize the self-care perception inconsistency, we repeated this analysis within the patient-physician consistent and inconsistent subgroups. Interestingly, the only difference in the subgroup analysis was that the physician score negatively predicted the patient self-care rating (P<.001, Table 2) in the inconsistent patient-physician self-care perception group (ie, the better the physician believed the patient is doing socioeconomically, the more likely the patient perceived their self-care to be negative).
Discussion and Conclusion
This study characterizes the lack of consistency between patients with T2D and their physicians regarding perceptions of patient self-care. Given the importance of physician-patient communication in management of chronic illnesses,11 there would ideally be consistency of self-care perceptions between patients and their physicians. However, results suggest there is an alarming lack of consistency 31% of the time. Notably, the patients’ perceptions of self-care are negatively correlated with HbA1c and elevated diabetes distress (Table 1), suggesting that knowing these may allow a physician to better understand a patient’s self-care perception.
This analysis assumes patient self-care rating should be used as the standard for the physician to meet. The Common-Sense Model (CSM) of Self-Regulation posits that health actions and outcomes exist in a feedback loop where previous experiences inform future outcomes.12 Aljasem et al found that self-efficacy, defined as “the feeling of control over one’s illness” explained 4%-10% of the variance in self-care behaviors,4 consistent with other literature.6,13,14 We used the CSM framework to suggest that just as self-efficacy affects self-care behaviors, patient perceptions of their self-care may likely affect their beliefs of self-efficacy. Therefore, regardless of the accuracy of patient self-care beliefs, physicians need to accurately understand patient self-care perceptions to apply educational interventions that improve patient self-efficacy. In other words, achieving self-care perception consistency informs appropriate application of interdisciplinary education by social work, behavioral health, and nursing personnel.
This study has limitations. As a cross-sectional, quantitative survey study, this study is only able to define correlation. As this study was completed at resident training sites, this study’s generalizability to other health care models is limited. There is also the potential of selection bias as an unknown percentage of patients agreed to complete the survey. Furthermore, this survey was not targeted at detailing patient self-care and barriers or enablers of self-care. The 4-point Likert scale response for self-care can be considered vague and difficult to define similarly between every patient and physician. Additionally, this study is not able to quantify the impact of self-care perception consistency on patient diabetes management. Of note, the R2 is low given that the dependent variable, self-care rating, is not perfectly continuous as a Likert-scale that creates a statistical limitation for the study. Further study of diabetes distress and self-care perception in its impact on patient-physician relationships and glycemic control is warranted.
Achieving diabetes control is important to patients and physicians. Enhancing the discussion to improve a patient’s ability to achieve that control is paramount to patients’ health. This study suggests that diabetes distress may theoretically influence glycemic control through its relation to self-care perception, ultimately influencing self-efficacy as predicted by the CSM of self-regulation. A possible method of aligning patient and physician perceptions may be directly asking about diabetes distress and self-care perception.15,16 This study adds to our understanding of the patient-physician interaction that affects diabetes treatment.
Acknowledgments
The authors thank the Residency Research Network of Texas for working together on this project to compile data across all the sites, especially the many summer fellows who assisted in data collection, entry, and cleaning.
Financial Support
This project was funded with the help of the Texas Academy of Family Physicians Foundation. This project was also supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant UL1 TR002645. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Ethics Statement
All studay participants were provided written informed consent. This study obtained IRB approval from UT Southwestern Medical Center.
Data Statement
A full copy of study data is available by contacting the corresponding author at CruzI@uthscsa.edu.
References
- Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metab Disord. 2013;12(1):14. doi:10.1186/2251-6581-12-14
- Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143-164. doi:10.1177/1090198104263660
- Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006;29(4):823-829. doi:10.2337/diacare.29.04.06.dc05-1615
- Aljasem LI, Peyrot M, Wissow L, Rubin RR. The impact of barriers and self-efficacy on self-care behaviors in type 2 diabetes. Diabetes Educ. 2001;27(3):393-404. doi:10.1177/014572170102700309
- Lee SF, Teh XR, Malar LS, Ong SL, James RP. The associations of illness perception with metabolic control (HbA1c) among type 2 diabetes mellitus patients in a district hospital. Int J Pharm Pract. 2018;26(5):442-449. doi:10.1111/ijpp.12413
- Kugbey N, Oppong Asante K, Adulai K. Illness perception, diabetes knowledge and self-care practices among type-2 diabetes patients: a cross-sectional study. BMC Res Notes. 2017;10(1):381. doi:10.1186/s13104-017-2707-5
- Bridges HA, Smith MA. Mediation by illness perceptions of the association between the doctor-patient relationship and diabetes-related distress. J Health Psychol. 2016;21(9):1956-1965. doi:10.1177/1359105315569094
- National Association of Community Health Centers. “PRAPARE.” http://www.nachc.org/research-and-data/prapare/. Accessed Feb 8, 2019.
- Polonsky WH, Fisher L, Earles J, et al. Assessing psychosocial distress in diabetes: development of the diabetes distress scale. Diabetes Care. 2005;28(3):626-631. doi:10.2337/diacare.28.3.626
- Bradley C, Todd C, Gorton T, Symonds E, Martin A, Plowright R. The development of an individualized questionnaire measure of perceived impact of diabetes on quality of life: the ADDQoL. Qual Life Res. 1999;8(1-2):79-91. doi:10.1023/A:1026485130100
- Stweart MA. “Effective physician-patient communication and health outcomes: a review.” CMAJ. 1995. 1;152(9):1423-33. PMCID: PMC1337906.
- Leventhal H, Phillips LA, Burns E. The Common-Sense Model of Self-Regulation (CSM): a dynamic framework for understanding illness self-management. J Behav Med. 2016;39(6):935-946. doi:10.1007/s10865-016-9782-2
- Nie R, Han Y, Xu J, Huang Q, Mao J. Illness perception, risk perception and health promotion self-care behaviors among Chinese patient with type 2 diabetes: A cross-sectional survey. Appl Nurs Res. 2018;39(39):89-96. doi:10.1016/j.apnr.2017.11.010
- Mc Sharry J, Moss-Morris R, Kendrick T. Illness perceptions and glycaemic control in diabetes: a systematic review with meta-analysis. Diabet Med. 2011;28(11):1300-1310. doi:10.1111/j.1464-5491.2011.03298.x
- Shahady E, O’Grady E. Diabetes distress: a common occurrence in patients unable to control their diabetes. Consultant. 2015;55:428-439. Accessed October 15, 2021. https://www.consultant360.com/articles/diabetes-distress-common-occurrence-patients-unable-control-their-diabetes
- American Diabetes Association. Standards of Medical Care in Diabetes-2020Abridged for Primary Care Providers. Clin Diabetes. 2020;38(1):10-38. doi:10.2337/cd20-as01



There are no comments for this article.