Introduction: Although human immunodeficiency virus (HIV) care is a recommended competency for family medicine training, many programs report a lack of HIV expertise among faculty. After the departure of faculty with HIV care experience, an interprofessional HIV quality improvement team (HIV-QIT) of physicians and pharmacists aimed to maintain on-site HIV care and retain learning opportunities for residents, using process improvement and panel reviews with a remote HIV specialist faculty member.
Methods: This study reports on a multicycle quality improvement pilot project with pre- and postintervention chart reviews between December 2019 and May 2021. All patients received primary care and HIV-QIT chart reviews on-site. We compared patients with integrated HIV care on-site to those receiving external HIV specialty care. Primary outcomes included virologic suppression, CD4 count ≥200 cells/mm3, and adherence to guideline-recommended HIV care. In cycle 1 (January-June 2020), the HIV-QIT reviewed patient charts and sent guideline-based recommendations to physicians. In cycle 2 (July 2020-May 2021), the HIV-QIT implemented several HIV-specific processes, including decision support updates, note templates, order sets, and reference materials. Sustained process improvements included HIV panel chart audits every 3 to 6 months and subsequent provider education.
Results: Of 29 patients, more than half (55%, n=16) received integrated HIV care at the primary care site. We found no significant difference in care quality measures between primary and specialty care. Barriers to care completion included missed or canceled follow-up visits, on-site phlebotomy service closures, and declined HIV services.
Conclusions: The HIV-QIT maintained on-site HIV treatment and retained experiential learning opportunities through process improvement and specialist-supported care recommendations to primary care physicians.
Advances in care have transformed human immunodeficiency virus (HIV) from a fatal disease into a chronic condition. HIV workforce shortages and limited access to HIV specialists highlight the need to integrate HIV care into primary care practice.1–3 The American Academy of Family Physicians has recommended that residents achieve competency in creating HIV guideline-based treatment plans.4 However, in a 2013 survey of family medicine residency program directors, only 21% reported having faculty with HIV care expertise.5 The longitudinal remote consultation method used in Project ECHO (Extension for Community Healthcare Outcomes) has increased community provider confidence in treating HIV.6 Additionally, an HIV multidisciplinary care model can improve treatment outcomes and increase retention of patients living with HIV in primary care settings.7–9
Prior evaluations have documented that patients prefer integrated HIV and primary care, but infectious diseases specialists have reported variable comfort providing primary care services.2,10 Family medicine residencies are well-equipped for complex discussions regarding immunizations, cancer screening, and cardiovascular risk management, but may lack experience with HIV-specific recommendations.
UPMC Shadyside Family Health Center (SFHC) is an urban family medicine residency training practice located near several specialized HIV care sites, but without on-site HIV expertise after losing two faculty physicians trained in HIV care. To maintain patient care, we developed an interprofessional HIV quality improvement team (HIV-QIT) of faculty physicians, family medicine residents interested in HIV, and clinical pharmacists to optimize and standardize HIV care within our practice. The team received remote supervision quarterly from an external HIV specialist (credentialed by the American Academy of HIV Medicine) family physician practicing in a nearby family medicine residency and a comprehensive HIV primary care site. The HIV-QIT format was informed by the Ryan White model and Project ECHO, although not affiliated with either national program.11,12 We aimed to maintain on-site integrated HIV treatment quality, as compared with external specialist HIV care, and to retain experiential learning opportunities using process improvement and specialist-supported care recommendations to primary care physicians during an 18-month intervention.
We completed a multipronged quality improvement project with pre- and postintervention chart reviews comparing care of patients who received HIV care from primary care providers at SFHC (integrated HIV care) to patients who received primary care at SFHC but HIV care at other sites (specialty HIV care). We included patients who had an HIV diagnosis, positive HIV antibody, or viral load results and who attended an SFHC office visit within 2 years. We excluded patients transferring primary care elsewhere before the baseline assessment (n=21). Baseline demographic data, including patient-reported sex, race, and ethnicity, were collected in December 2019 from electronic health record (EHR, EPIC software) entries, with limited gender options prior to upgrades in 2022.
We completed two plan-do-study-act (PDSA) cycles in January through June 2020 and July 2020 through May 2021. PDSA is an iterative problem-solving model used for process improvement, including evaluating effectiveness of an implemented change.13
PDSA Cycle 1 (January–June 2020)
An HIV-QIT champion assigned patients for review and scheduled team meetings. HIV-QIT members individually reviewed and precharted on each patient, then presented to the HIV specialist during the meeting. After discussion, HIV-QIT members sent recommendations for patients to their primary care physicians through EHR messages. Recommendations were based on national Department of Health and Human Services (DHHS) guidelines, with additional specialist input for community and health system resources.14 Example recommendations included confirmation of hepatitis B immunity, dual-energy x-ray absorptiometry (DXA) screening, where to send patients for follow-up anoscopy, and rarely, HIV therapy optimization. No funding was provided outside of existing salaries, and the HIV-QIT did not bill for services. Initial panel review required at least 30 minutes per patient, with subsequent quarterly reviews lasting approximately 4 hours (5-15 minutes/patient), including brief teaching discussions of clinical controversies.
Cycle 1 identified practice patterns and informed several system changes. For example, 48% of charts were missing HIV updates to the Epic EHR decision support tools because that addition required manual updates by providers. Lack of decision support has been identified as a barrier to lab testing adherence in other settings.15 The HIV-QIT requested and obtained a system-wide EHR update to automatically trigger the decision support tool with an HIV diagnosis entry as well as an update to the tool to include meningococcal immunization.
PDSA Cycle 2 (July 2020-May 2021)
SFHC implemented HIV-specific note templates, order sets, and reference materials; HIV care quality reporting and interprofessional panel monitoring with remote specialist consultation; a pooled EHR inbox; and pharmacist consults for antiretroviral therapy (ART).
Outcomes included virologic suppression and adherence to guideline-recommended HIV care. Where data was missing, the last observation was carried forward. The shifting patient population precluded paired tests. We analyzed data with descriptive statistics and χ2 using Fisher’s exact test. Baseline findings guided additional quality improvement efforts. The Institutional Quality Improvement Review Committee for our organization, which exists to ensure the ethical conduct of quality improvement projects, reviewed and approved this project.
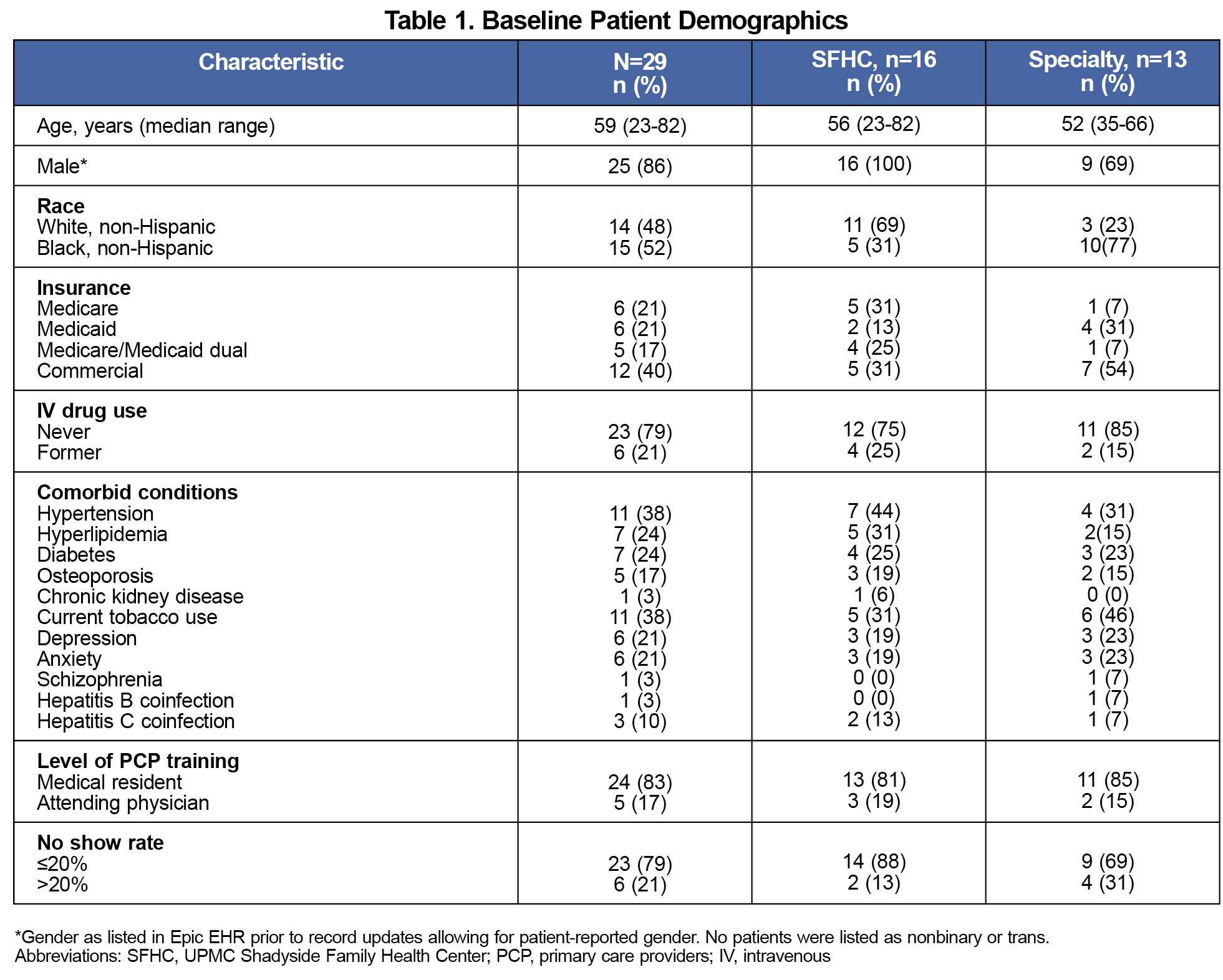
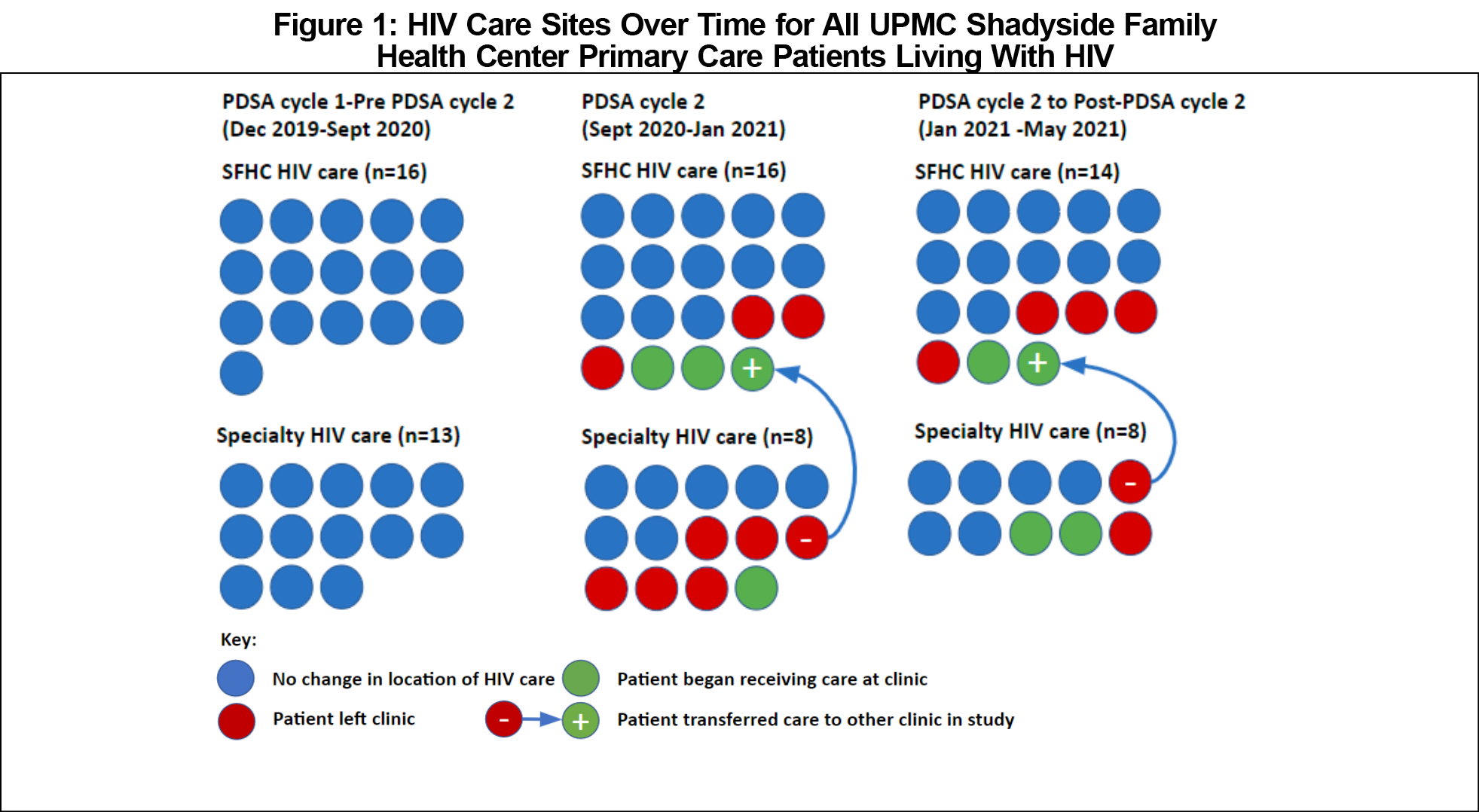
Apart from race and Medicare coverage, baseline demographic data were comparable between care sites. Of 29 eligible patients, approximately half were Black, 86% were men as listed in the EHR, and the median age was 59 (Table 1). All patients received primary care at SFHC, and more than half (55%, n=16) received integrated HIV care at SFHC. Thirteen patients received specialist HIV care at six local clinics. By the end of the study period, 13 patients left the SFHC practice and 6 joined, for a total of 22 patients reviewed in May 2021. Figure 1 depicts sites of HIV care over time.
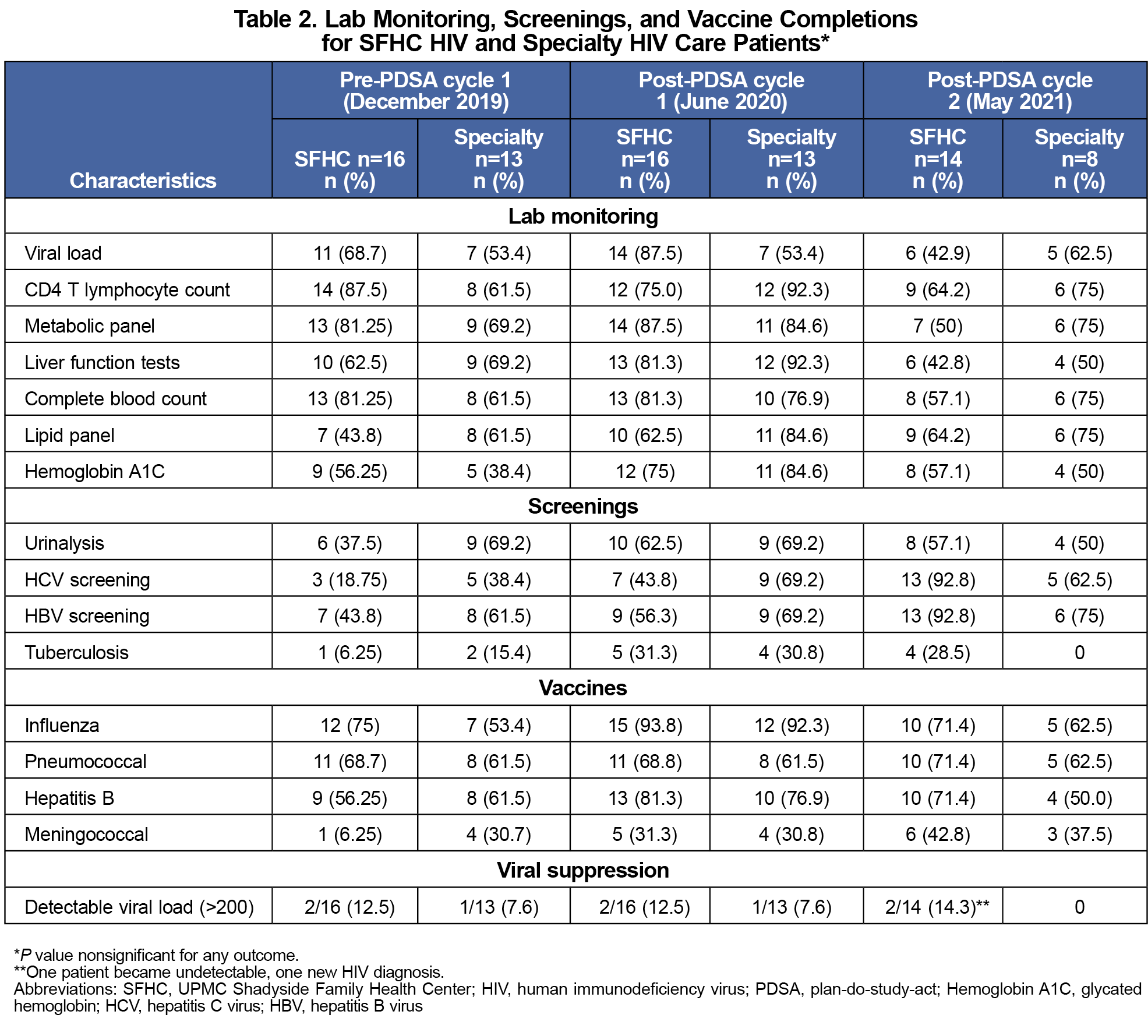
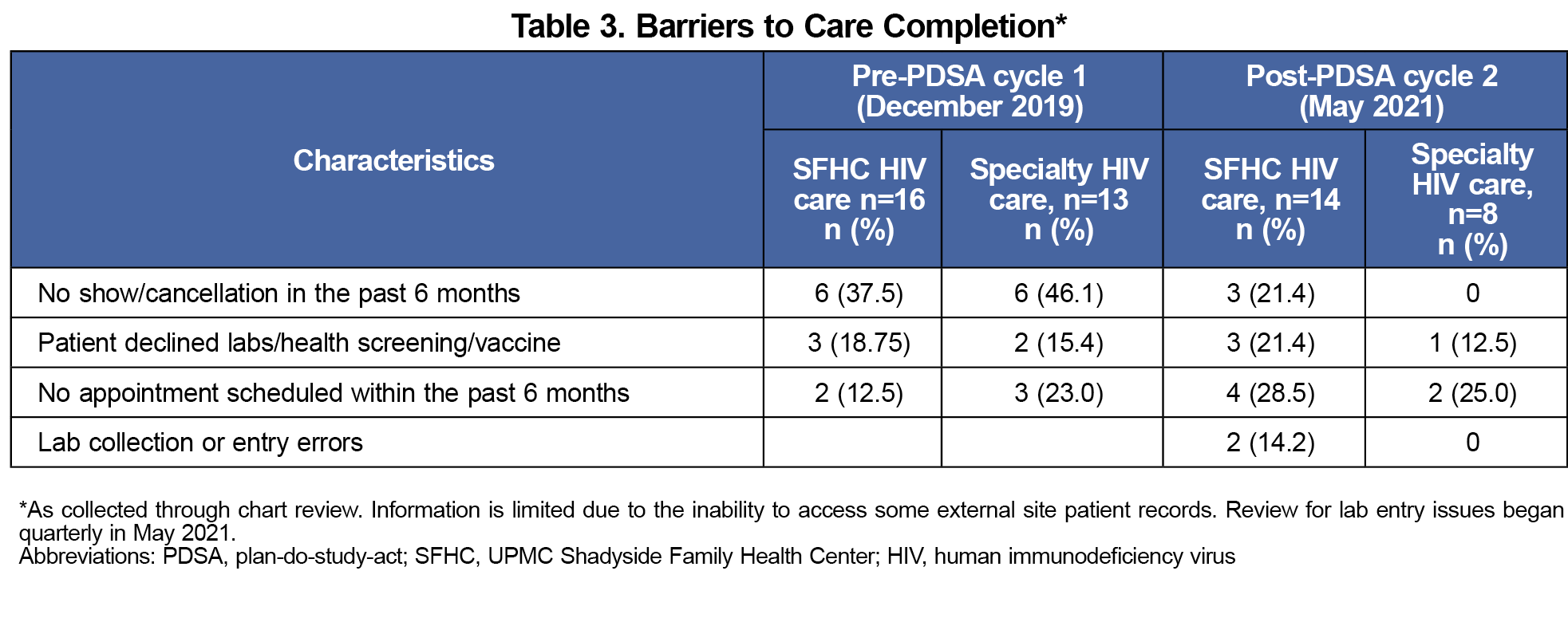
Care quality measures did not differ significantly between sites. Table 2 compares adherence to HIV guideline recommendations between sites. Testing completion rates for viral load, CD4 T lymphocyte count, liver function test, and complete blood count decreased between cycle 1 and cycle 2 for both sites. Hepatitis B virus and hepatitis C virus screening, and meningococcal vaccination rates increased at SFHC across all time points. Barriers to care completion include missed or canceled follow-up, shown in Table 3.
The HIV-QIT enabled SFHC to maintain on-site HIV treatment and retain experiential learning opportunities through process improvement and specialist-supported care recommendations. The HIV-QIT implementation did not improve viral suppression or adherence to care processes in a cohort of patients at the SFHC, but highlighted opportunities for continued improvement of HIV treatment and primary care, regardless of integrated or specialist HIV care.
We noted that most of the patients with Medicare coverage received care at SFHC. Overall, a higher proportion of SFHC patients were 55+ years old, which we attributed to the two prior SFHC faculty physicians maintaining longtime panels of patients living with HIV. We found an apparent difference in where Black and White patients receive HIV care. Race distribution differences did not appear to be related to other collected information and merit further investigation.
We observed no differences in measured targets between specialty or integrated primary care HIV services, though the small sample size limited the power of the study. We were unable to access clinical information for two specialty clinics outside our system, which may have resulted in care underestimations.
Barriers to care completion included missed or canceled follow-up and declined services. We found on-site phlebotomy important to timely lab test completion, particularly with this patient population’s monitoring burden. In mid-2020, on-site phlebotomy at SFHC was temporarily suspended without a reimplementation timeline. This and other COVID-19-related precautions decreased lab monitoring frequency, mirroring nationally observed trends for Ryan White providers in 2020.16 The reduction of COVID-19 precautions is expected to decrease patient barriers.
Ongoing remote HIV specialist support will be required for our project’s sustainability. Our site has been fortunate to work with a faculty member who directs a primary care HIV experience available to residents at three area family medicine residency programs. Time for panel reviews was not formally budgeted or offset for the supervising HIV specialist or any team members. A clinical pharmacist faculty member served as the primary supporting faculty, with resident champions shouldering administrative roles. Additional practice-based barriers to panel reviews included scheduling meetings and resident leadership turnover. The largest threat to ongoing HIV-QIT success is lack of secured time for the meetings, patient reviews, and the process of obtaining and cleaning report data.
The HIV-QIT approach in a family medicine residency maintained evidence-based HIV treatment, HIV-informed primary care, and resident HIV education without on-site faculty HIV expertise. We will continue interprofessional panel reviews, provider education, and monitoring of outcomes of the HIV-QIT. Next steps include incorporating social work and nurse care coordination at HIV-QIT panel reviews to address barriers to care completion. The HIV-QIT approach is a small-scale implementation influenced by the ECHO model and may be practical for other primary care residency sites to maintain integrated HIV care for small panels lacking physical access to specialists. This approach also provides critical HIV care training that resident physicians continue to use in future practice and may be adapted to additional care populations.
Acknowledgments
The authors acknowledge Dr Deborah McMahon, MD, for sharing her HIV data collection template and providing her expertise. They also thank Dr Norman Kolb, Dr Teiichi Takedai, and Dr Scott Brown for participating in HIV panel review and discussions, as well as Shannon Dudich for assisting with data collection.
Presentations:
Poster: American Society of Health-System Pharmacists Midyear Clinical Meeting, December 8-12, 2019, Las Vegas in NV.
Poster: American College of Clinical Pharmacists Virtual Poster Symposium, October 1-3, 2020.
References
- Gilman B, Bouchery E, Barrett K, et al. HIV Clinician Workforce Study. Mathematica Policy Research; 2013. Accessed July 18, 2023. https://www.mathematica.org/publications/hiv-clinician-workforce-study
- Cheng QJ, Engelage EM, Grogan TR, Currier JS, Hoffman RM. Who provides primary care? an assessment of HIV patient and provider practices and preferences. J AIDS Clin Res. 2014;5(11):366. doi:10.4172/2155-6113.1000366
- Wijesinghe S, Alexander JL. Management and treatment of HIV: are primary care clinicians prepared for their new role? BMC Fam Pract. 2020;21(1):130. doi:10.1186/s12875-020-01198-7
- Recommended Curriculum Guidelines for Family Medicine Residents: HIV Infection/AIDS.American Academy of Family Physicians; 2019, Reprint No. 273. https://www.aafp.org/students-residents/residency-program-directors/curriculum-guidelines.html
- Prasad R, D’Amico F, Wilson SA, et al. Training family medicine residents in HIV primary care: a national survey of program directors. Fam Med. 2014;46(7):527-531. https://www.stfm.org/familymedicine/vol46issue7/Prasad527
- Wood BR, Unruh KT, Martinez-Paz N, et al. Impact of a telehealth program that delivers remote consultation and longitudinal mentorship to community HIV providers. Open Forum Infect Dis. 2016;3(3):ofw123. doi:10.1093/ofid/ofw123
- Elgalib A, Al-Sawafi H, Kamble B, Al-Harthy S, Al-Sariri Q. Multidisciplinary care model for HIV improves treatment outcome: a single-centre experience from the Middle East. AIDS Care. 2018;30(9):1,114-1,119. doi:10.1080/09540121.2018.1479028
- Olea A Jr, Grochowski J, Luetkemeyer AF, Robb V, Saberi P. Role of a clinical pharmacist as part of a multidisciplinary care team in the treatment of HCV in patients living with HIV/HCV coinfection. Integr Pharm Res Pract. 2018;7:105-111. doi:10.2147/IPRP.S169282
- Sherer R, Stieglitz K, Narra J, et al. HIV multidisciplinary teams work: support services improve access to and retention in HIV primary care. AIDS Care. 2002;14(suppl1):S31-S44. doi:10.1080/09540120220149975
- Fultz SL, Goulet JL, Weissman S, et al. Differences between infectious diseases—certified physicians and general medicine—certified physicians in the level of comfort with providing primary care to patients. Clin Infect Dis. 2005;41(5):738-743. doi:10.1086/432621
- Agley J, Delong J, Janota A, Carson A, Roberts J, Maupome G. Reflections on Project ECHO: qualitative findings from five different ECHO programs. Med Educ Online. 26(1):1936435. doi:10.1080/10872981.2021.1936435
- Beane SN, Culyba RJ, DeMayo M, Armstrong W. Exploring the medical home in Ryan White HIV care settings: a pilot study. J Assoc Nurses AIDS Care. 2014;25(3):191-202. doi:10.1016/j.jana.2013.10.007
- Plan-Do-Study-Act (PDSA) directions and examples. In: AHRQ Health Literacy Universal Precautions Toolkit. Agency for Healthcare Research and Quality; content last reviewed September 2020. https://www.ahrq.gov/health-literacy/improve/precautions/tool2b.html
- Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents with HIV. Department of Health and Human Services; March 23, 2023. Accessed July 18, 2023. https://clinicalinfo.hiv.gov/en/guidelines/adult-and-adolescent-arv
- Landovitz RJ, Desmond KA, Gildner JL, Leibowitz AA. Quality of care for HIV/AIDS and for primary prevention by HIV specialists and nonspecialists. AIDS Patient Care STDs. 2016;30(9):395-408. doi:10.1089/apc.2016.0170
- Dawson L, Kates J. Delivering HIV Care and Prevention in the COVID Era: A National Survey of Ryan White Providers. KFF; December 16, 2020. Accessed July 18, 2023.https://www.kff.org/hivaids/issue-brief/delivering-hiv-care-prevention-in-the-covid-era-a-national-survey-of-ryan-white-providers



There are no comments for this article.