Introduction: Family physicians use a variety of medications and techniques to perform intra-articular knee injections in the treatment of knee osteoarthritis. Currently, there is no consensus in the literature among the various specialties that perform joint injections for osteoarthritis of the knee regarding frequency of injections and injectate. The purpose of this study is to examine (1) the types of intra-articular knee injections used by family physicians for arthritis, (2) the most commonly used injectate, (3) the procedural approach, and (4) the maximum number of times the majority of family physicians would inject a single knee. Our study provides a descriptive epidemiology of current knee injection practices in the United States among family physicians.
Methods: Surveys were emailed to family physicians. We evaluated and analyzed responses.
Results: We received 360 responses, of which 317 family physicians indicated using intra-articular knee injections for pain. The majority (99%) used intra-articular injection steroid therapy in the treatment of knee osteoarthritis. About half (57.4%) of the family physicians would inject the same knee between one to five times.
Conclusion: This study provides an overview of current practices in intra-articular injections among family physicians in the United States and provides important information regarding injection practices. Given the lack of consensus and that current practice contradicts evidence in the literature, consideration should be given among all specialties who perform joint injections to create evidence-based clinical practice guidelines to optimize patient care.
Injections are common practice in the treatment of painful osteoarthritis; however, there is currently limited literature that addresses the prevalence of various injection types, uses, frequencies, and techniques among family physicians. The general algorithm for the treatment of knee arthritis includes nonoperative interventions including weight loss, pain medications, bracing, physical therapy, exercise programs, and injections.1 Yet, no consensus exists regarding the evidence and efficacy of these injections. For example, steroids are a common treatment for knee osteoarthritis, despite research demonstrating no improved pain at 2 years with triamcinolone versus saline injection, and loss of cartilage.2
This study examines current knee injection practices among family physicians as musculoskeletal complaints often initially present to the office of a family physician. The objective of this study was to explore current trends in intra-articular knee injections including type, frequency, and other details of current injection practice.
A 24-question survey was sent to family physicians via email. Our institution’s institutional review board determined the survey to be exempt from approval. We used a convenience sample to gather responses. The survey was distributed via listservs and an exact response rate could not be determined. The survey was specifically distributed to members of the Association of Family Medicine Residency Directors (AFMRD, with a membership of over 1,000 physicians) and the Texas Academy of Family Physicians (with a membership of over 8,000 physicians). The survey responses were collected from August 1, 2020 to September 30, 2020. The questions examined family physician demographics, location, type of medical training/medical practices, and various indications the physicians considered when performing intra-articular injections. We analyzed results using Microsoft Excel.
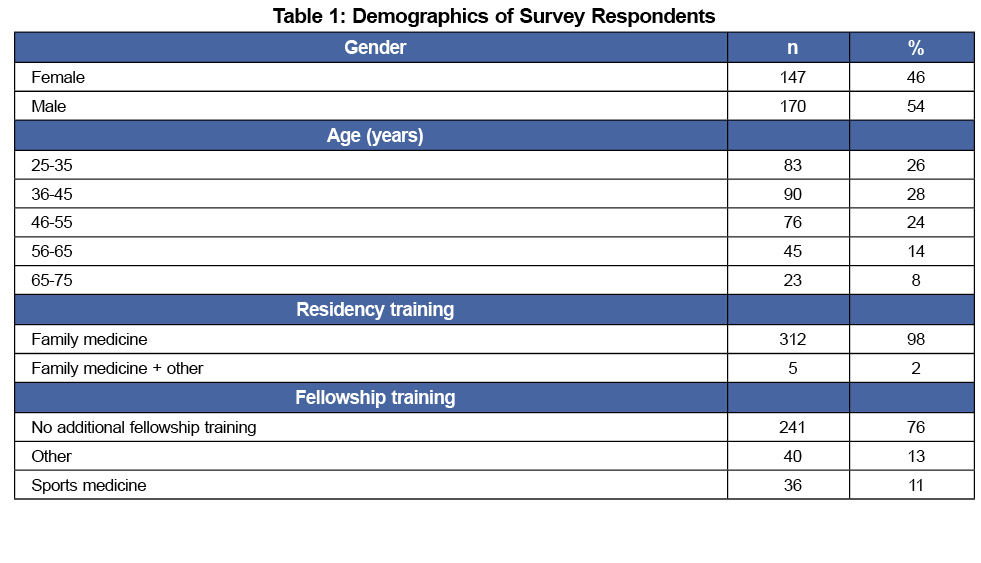
A total of 317 family physicians who had performed intra-articular knee injections were in the final study population. Approximately half (54%) of the respondents worked in an academic setting. Results are further summarized in Table 1.
There was a wide age range, from 25 to 35 years old (26.2%), 36 to 45 (28.4%), 46 to 55 (24.0%), 56 to 65 (14.2%), and 65 to 75 (7.3%). Approximately 7% of respondents had been in practice less than 1 year, 38.8% from 1 to 10 years, 22.4% from 10 to 20 years, and 31.5% for more than 20 years.
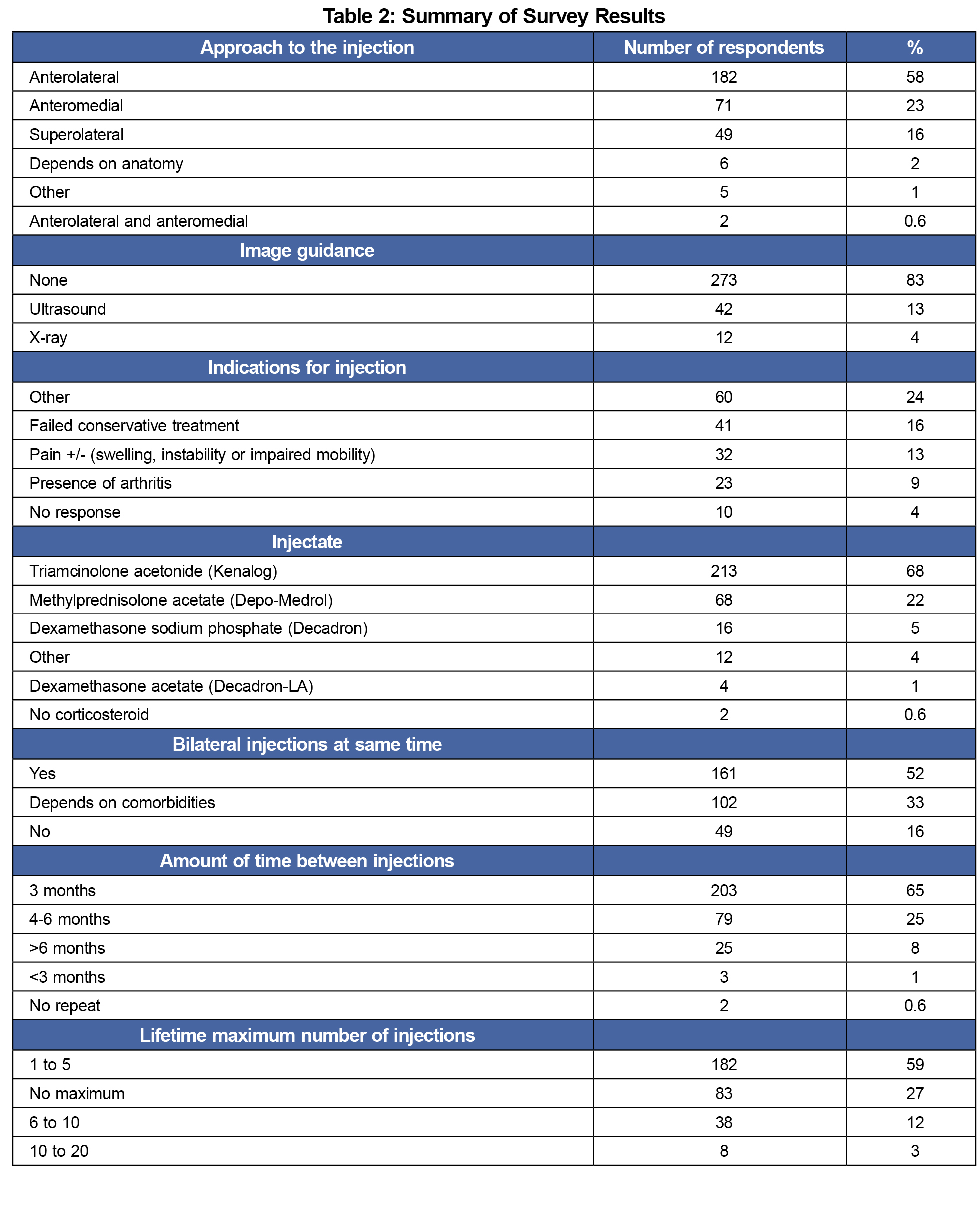
The proposed indications for injection therapy in individuals with knee arthritis were grouped into six categories, as shown in Table 2. Most family physicians (86.1%) did not use guided imaging. The anterolateral approach was the most favored (58%), followed by anteromedial (23.3%) and superolateral (15.5%). The most common injectate was triamcinolone acetonide (67.2%). Sixty-eight family physicians (21.5%) used methylprednisolone acetate, 16 (5%) used dexamethasone sodium phosphate, and four (1%) used dexamethasone acetate. The majority of family physicians used 40 mg triamcinolone acetonide with less than 4 mL of lidocaine as part of their injection cocktail.
Regarding timing and frequency of performing intra-articular knee injections, approximately half (50.8%) of family physicians would perform bilateral injections in the same clinical visit (Table 2). The majority (57.4%) would inject the same knee a lifetime maximum of one to five times (Table 2), requiring at least 3 months between injections in the same knee (64.0%, Table 2); 90.5% had no minimum time after injection to evaluation for arthroscopic surgery.
Our study provides a snapshot of family physician practices regarding joint injections. Understanding current practices among this population of clinicians is important because most nonoperative management, including intra-articular injections, will be done by family physicians prior to referral for surgical intervention.
Our study also highlights several gaps between evidence in the literature and current practice. For example, we found most family physicians chose to use triamcinolone acetonide (67.2%), followed by methylprednisolone acetate (21.5%, most likely due to the lipid solubility of triamcinolone acetonide versus the water-soluble methylprednisolone acetate3). Yet, some literature reports increased cartilage breakdown with triamcinolone vs placebo,2 and other literature notes methylprednisolone acetate and triamcinolone acetonide are equally effective in treatment of knee arthritis in those with chronic inflammatory knee arthritis.4 Also, while ultrasound-guided injection enhances injection accuracy and improves patient-reported outcomes,5 only 13% of family physicians reported using this technique. Smart et al found no definitive injection approach to knee arthritis injections.6 The majority of family physicians surveyed in this study do not have a finite number of steroid injections they will provide but are waiting 3 months between injections. Injection therapy has traditionally been used as a bridge for the time between arthritic pain onset and total knee arthroplasty.1 Most family physicians in the study will send for an evaluation for surgical evaluation, despite a recent intra-articular injection. However, Richardson et al found a statistically significant increase in periprosthetic joint infection in patients who received an intra-articular injection within 3 months of surgery.7
There are several limitations to this study. First, we did not collect information on why the family physicians had certain practice habits. Due to study design, which utilized a convenience sample, only a cross section of family physicians were surveyed. Addressing the above limitations as well as a comparison with injection practices among orthopedic surgeons and rheumatologists using a more robust sampling design to increase representativeness are future directions for this research.
The gaps between evidence and practice identified in this study and a general lack of consensus among the different specialties that perform intra-articular injection for knee osteoarthritis can be problematic if they lead to suboptimal patient care and potentially adverse patient outcomes such as increased cartilage breakdown and periprosthetic joint infection. They underscore a need to create evidence-based clinical practice that bridge specialties to optimize patient care. Future research needs to clarify evidence-based practice across the various specialties that perform joint injections as well as compare the risks to the benefits of this intervention.
Acknowledgments
The authors thank Christen Walcher and Jeffrey Susman for editing the manuscript.
References
- Ringdahl E, Pandit S. Treatment of knee osteoarthritis. Am Fam Physician. 2011;83(11):1287-1292.
- McAlindon TE, LaValley MP, Harvey WF, et al. Effect of intra-articular triamcinolone vs saline on knee cartilage volume and pain in patients with knee osteoarthritis: a randomized clinical Trial. JAMA. 2017;317(19):1967-1975. doi:10.1001/jama.2017.5283
- Skedros JG, Hunt KJ, Pitts TC. Variations in corticosteroid/anesthetic injections for painful shoulder conditions: comparisons among orthopaedic surgeons, rheumatologists, and physical medicine and primary-care physicians. BMC Musculoskelet Disord. 2007;8(63):63. doi:10.1186/1471-2474-8-63
- Kumar A, Dhir V, Sharma S, Sharma A, Singh S. Efficacy of methylprednisolone acetate versus triamcinolone acetonide intra-articular knee injection in patients with chronic inflammatory arthritis: a 24-week randomized controlled trial. Clin Ther. 2017;39(1):150-158. doi:10.1016/j.clinthera.2016.11.023
- Berkoff DJ, Miller LE, Block JE. Clinical utility of ultrasound guidance for intra-articular knee injections: a review. Clin Interv Aging. 2012;7:89-95. doi:10.2147/CIA.S29265
- Smart KMP. Approaches to intra-articular injections for "dry" knee osteoarthritis. The Journal of Musculoskeletal Medicine. May 2012 2012;29(4):114-117.
- Richardson SS, Schairer WW, Sculco TP, Sculco PK. Comparison of infection risk with corticosteroid or hyaluronic acid injection prior to total knee arthroplasty. J Bone Joint Surg Am. 2019;101(2):112-118. doi:10.2106/JBJS.18.00454



There are no comments for this article.