In outpatient primary care clinics, clinicians spend a significant amount of their time in electronic medical records (EMR) refilling prescriptions for patients.1 Such time spent refilling medications has shown to increase stress, increase time spent on non-face-to-face interactions with patients, and lead to decreased job satisfaction and higher burnout rates among clinicians.2,3 Streamlining medication management protocols is essential to improving outcomes for both patients and providers.4 To ease this burden, a variety of medication refill protocols have been implemented across primary care settings. These have included pharmacy-led refill protocols, verbal distribution, and diseased-based algorithms.1,5,6 Because standardized medication refill protocols can potentially limit medication errors,5 improve adherence,7 improve patient care outcomes, increase efficiency,8 and limit undue harm to patients,5 our quality improvement study aimed to evaluate the use of a multidisciplinary medication refill protocol to decrease the time to complete refill requests and improve consistency in management.
LEARNER RESEARCH
Implementation of a Multidisciplinary Medication Refill Protocol
Samia Khan, DO | Jessica J. F. Kram, MPH | Dennis J. Baumgardner, MD | Amanda G. Sessions, DO | Patrick Foss, MD | Carl Bellinger, DO | Fabiana Kotovicz, MD
PRiMER. 2023;7:31.
Published: 9/11/2023 | DOI: 10.22454/PRiMER.2023.418724
Introduction: Primary care clinicians spend significant time managing nonvisit activities, including processing of requests for prescription renewal. Delays in processing refills may lead to patient dissatisfaction and impact provider productivity. Having nonclinicians process refills can be more efficient and time-saving. We aimed to evaluate the use of a multidisciplinary medication refill protocol to decrease the time to complete refill requests.
Methods: We implemented nursing-driven management of refill requests within two family medicine residency clinics in Milwaukee, Wisconsin (Phase 1: single clinic implementation [March 2017–June 2019]; Phase 2: added second clinic prepandemic [June 2019–March 2020] and postpandemic [April 2020–December 2020]). The multidisciplinary refill protocol was created by faculty, residents, pharmacy, and nursing. Data were collected using electronic health record time stamps to determine when refill requests were initiated and filled by faculty, residents, and nurses. We used Mood’s median test to compare the median time for medication refill completion. We used Levene’s test to test for equal variance surrounding the median of each caregiver group. We used Fisher’s exact test or χ2 test with Yates’ correction for 2×2 contingency tables.
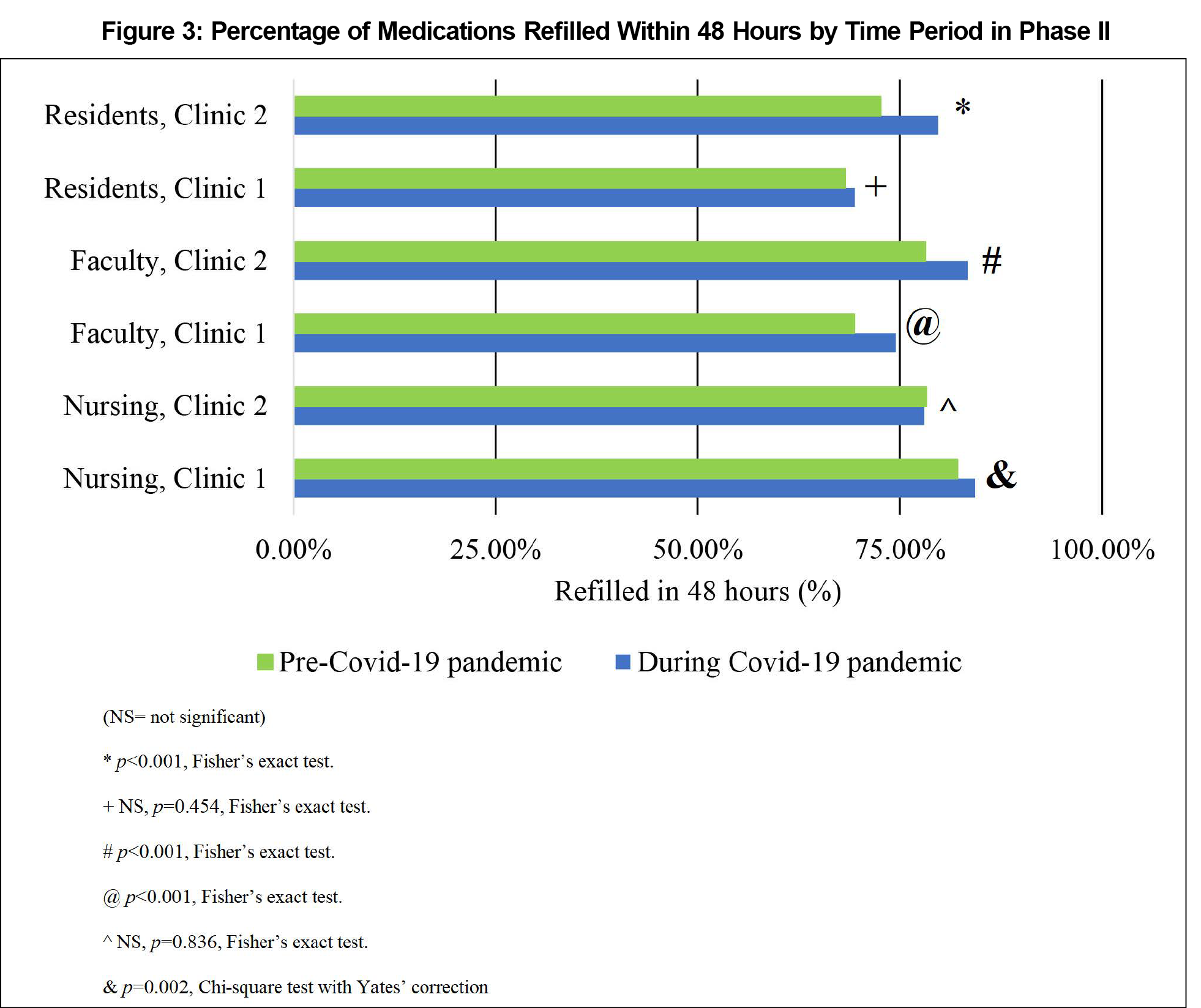
Results: In both phases, we identified a significant reduction in median time to refill completion (P<.001) and variability of time to refill completion (P<.001). Notably, in Phase 1, reduction in median refill time was most apparent among residents (383 vs 79 min postimplementation); and in Phase 2, the percentage of refills completed within 48 hours significantly increased between the pre-COVID-19 and COVID-19 pandemic among faculty and nursing in Clinic 1 and residents and faculty in Clinic 2 (all P’s<.001).
Conclusions: Implementation of a multidisciplinary refill protocol significantly improved time and predictability of refill completion in both phases.
Our study’s setting included two urban family medicine residency clinics in Milwaukee, Wisconsin. Combined, these were 62% Medicaid insured, and each patient population was 62% female.9 At the study’s onset, Clinic 1 had approximately 21,000 annual visits and was 26% White, 14% Black, 41% Hispanic, and 11% Asian; 12% were refugees; 9% were under 5 years old, and 16% were under 65 years old. Clinic 2 had approximately 13,000 annual visits and was 12% White, 70% Black, 9% Hispanic, and 7% Asian; 7% were refugees; 32% were under 5 years old, and 4% were under 65 years old.9
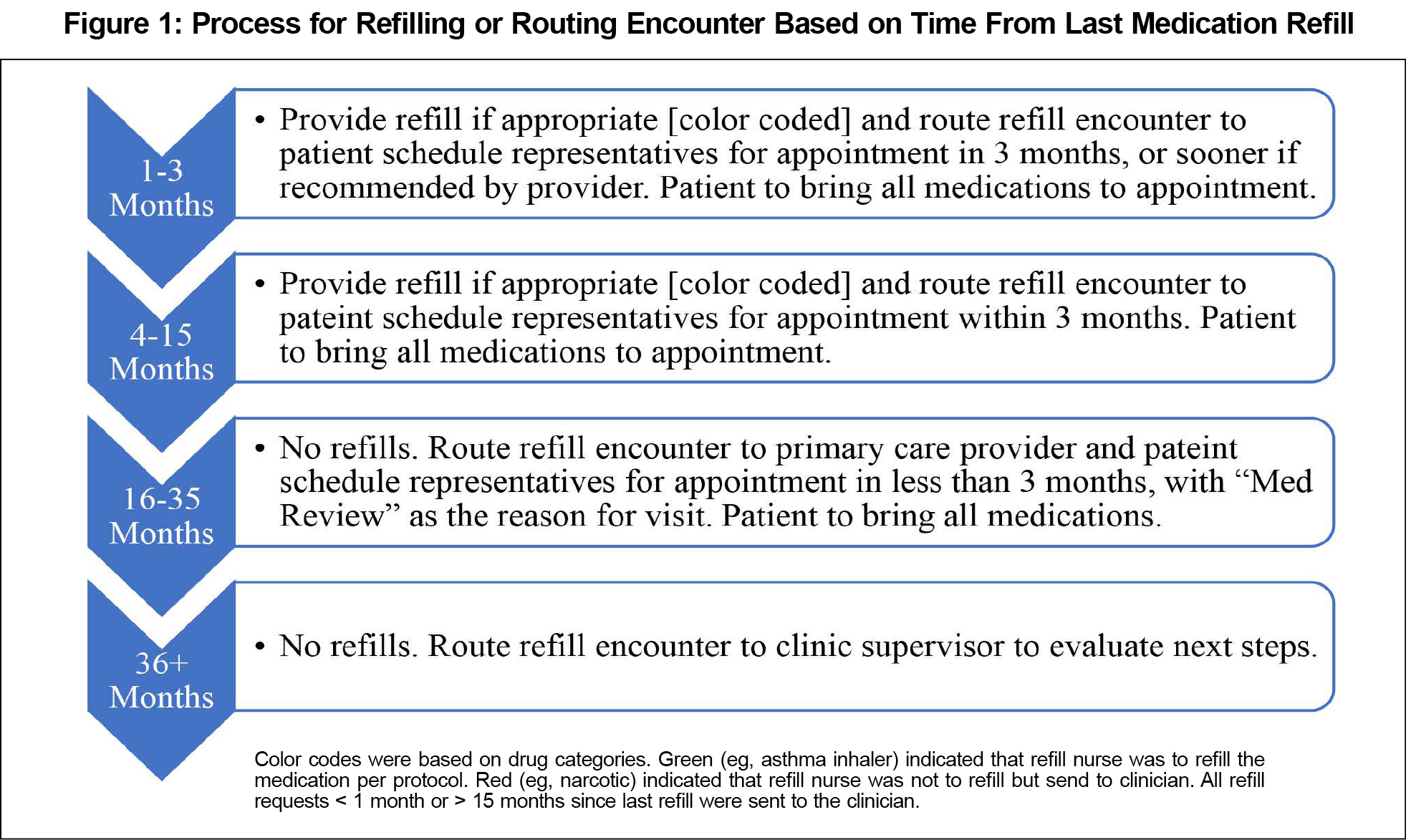
To allow for centralized, nursing-driven management of most prescription refills, we created a multidisciplinary medication refill protocol (Figure 1) in collaboration with faculty, residents, pharmacy, and nursing, based on Medicaid-covered medication categories in the State of Wisconsin, time of last refill, and time patient was last seen. The protocol initially was implemented in Clinic 1. Prior to implementation, refill requests were sent to primary care providers from different requestors, typically pharmacy and patients who contacted the call center. After protocol implementation, all requests were sent to a message pool for a dedicated refill nurse (a new position) to handle by protocol. Residents and faculty only received refill messages that the refill nurse could not handle without direct physician sign-off. Further, residents, faculty, or triage nurses received refill requests if additional concerns were raised upon initial chart review, the medication was excluded per the refill protocol, or the number of authorized refills by protocol were exhausted. Nurse triage also picked up requests delayed in the message pool.
Throughout our study, the Clinic 1 staff included eight faculty, 18 residents, two advanced care providers, and six nurses. Preimplementation data collection began in March 2017, and postimplementation data collection was completed by June 2019. We measured medication refill processing time (the time an EMR refill encounter was opened with a refill request to the time it was closed with refill approval or denial) in minutes and compared it to preprotocol implementation (March 2017–November 2017), during protocol adoption (December 2017–August 2018), and postprotocol implementation (September 2018–June 2019). We compared time for refill completion among three groups of caregivers (family medicine faculty, residents, and nursing).
In Phase 2, we expanded the protocol to Clinic 2, which included five faculty, 12 residents, one advanced care provider, and two nurses throughout our study. Focusing on outliers, we compared the time between refill opening and closure of a refill request (especially within 48 hours) between the two clinics prior to the SARS-CoV-2 (COVID-19) pandemic (June 2019–March 2020) and during the COVID-19 pandemic (April 2020–December 2020). Similarly, we compared time for refill completion among the three groups of caregivers.
All data were collected based on an EMR time stamp. If a medication refill request was initiated for multiple medications, these same data points were obtained for each subsequent medication. We used Mood’s median test to compare the median times for medication refill completion. We used Levene’s test to test for equal variance surrounding the median of each caregiver group. And we used GraphPad (Dotmatrix) software to make calculations of Fisher’s exact tests or χ2 tests with Yates’ correction for 2×2 to create contingency tables. We used Minitab version 13 (Minitab, LLC) statistical software for all other statistical analyses and considered P<.05 significant. This study was determined nonhuman subjects research by our Institutional Review Board.
Phase I
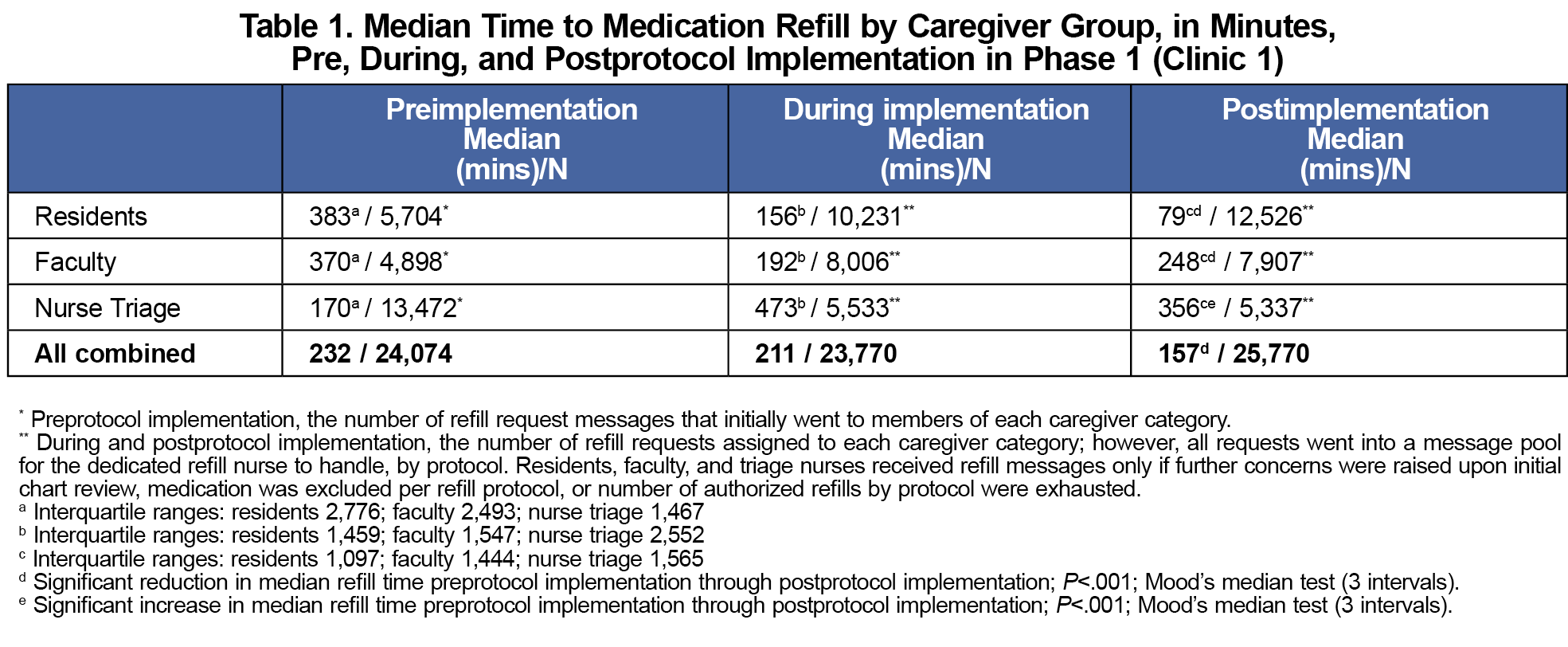
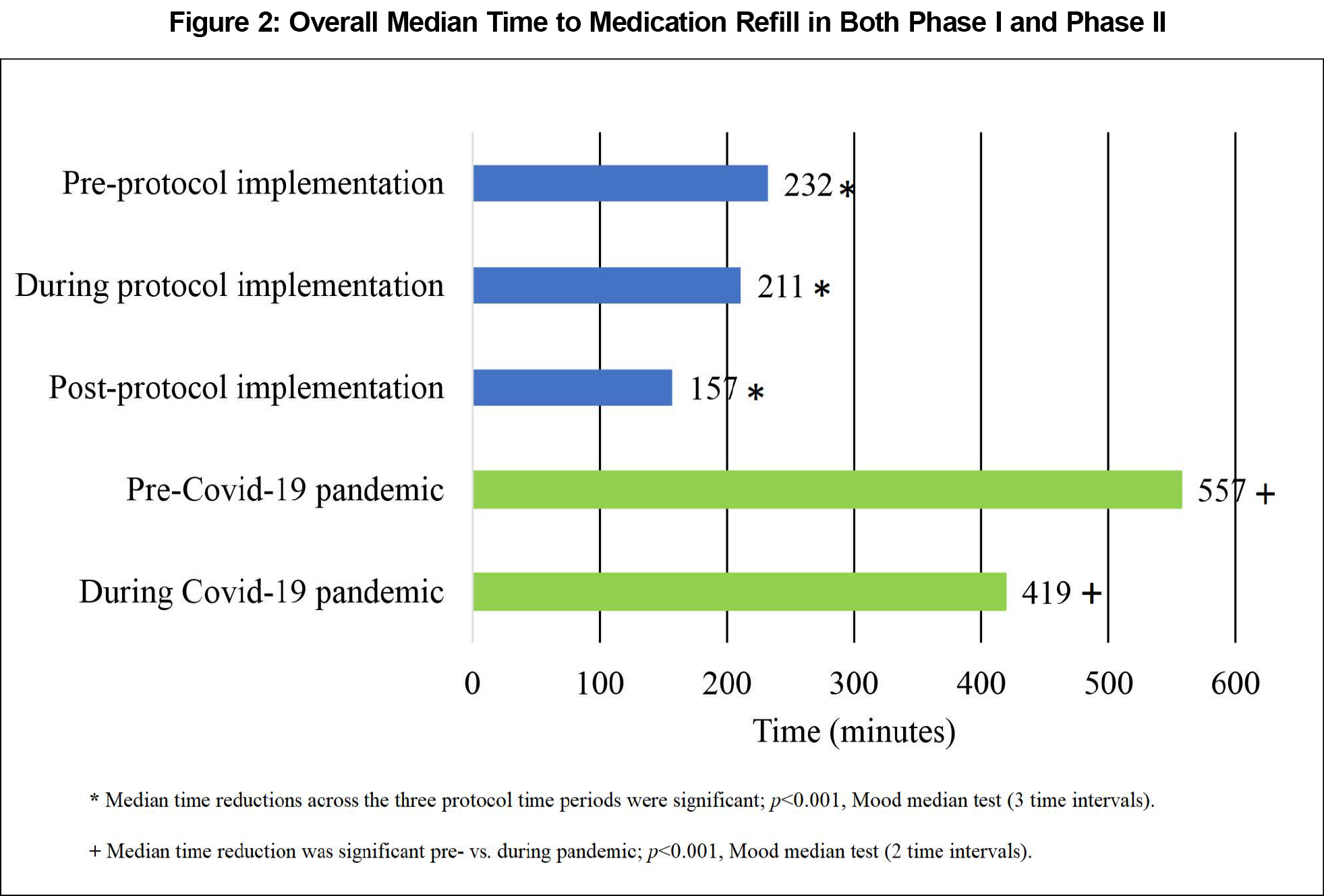
We identified a significant reduction in overall median time to refill completion across the three time periods (P<.001; Mood’s median test; Figure 2). Table 1 presents details of change in median refill time by time period and caregiver group. Response time standard deviations (SDs) had an overall reduction across groups with a preprotocol implementation mean SD of 14.5 days, 10.8 days during protocol adoption, and 6 days postprotocol. Using Levene’s test to test for equal variance surrounding the median of each caregiver group, we revealed a significant reduction (test statistic=125.3; P<.001).
Phase II
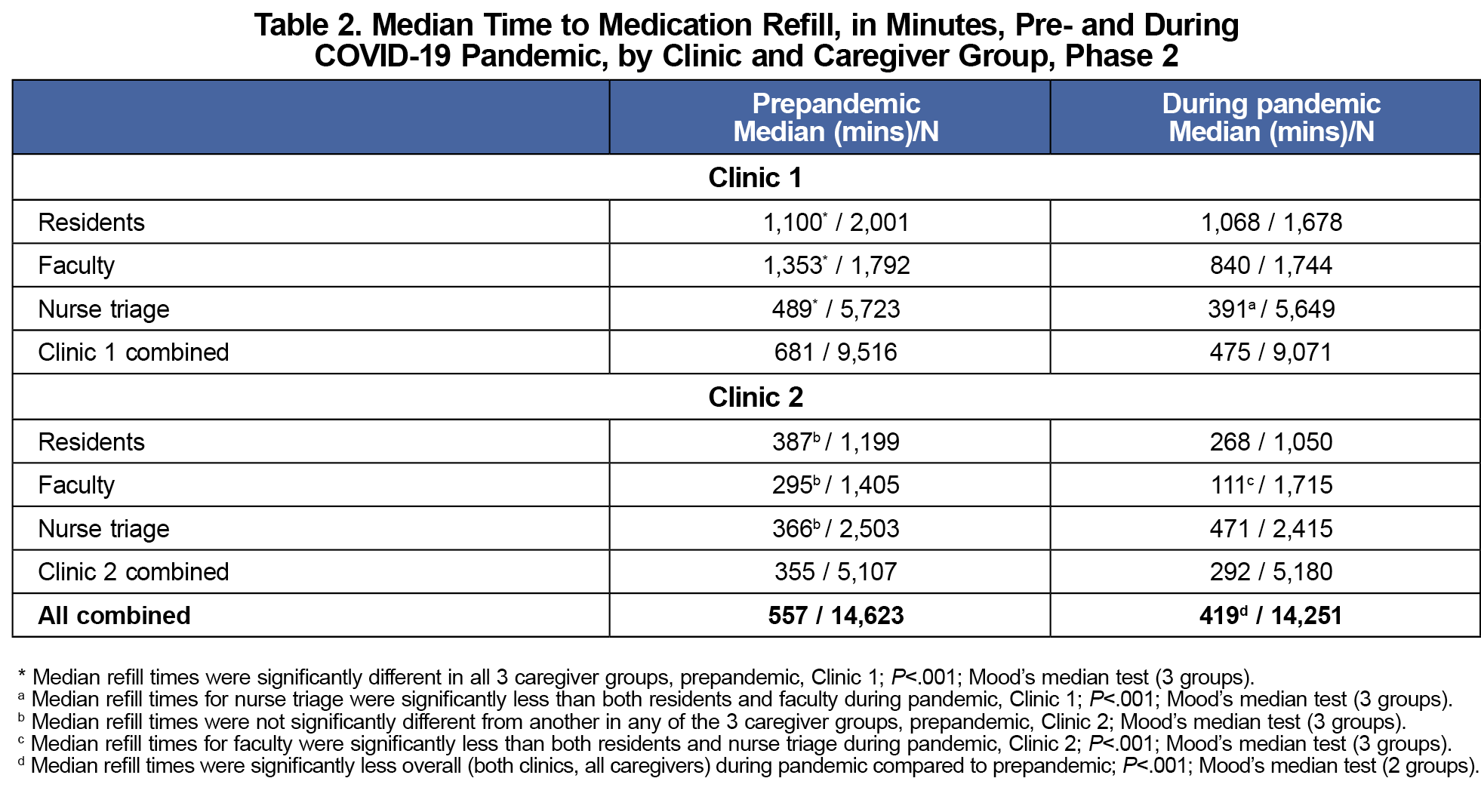
The total number of refills from the combined clinics were similar pre- and during the COVID-19 pandemic (N=14,623 vs 14,251), and 64.4% of refills were at Clinic 1 in each case. We found significant reductions in median time to refill (Figure 2) and variability in response time (Levene’s test=20.6; P<.001) between the two time periods. When comparing clinics overall, regardless of time period, we also found a significant reduction in median time to refill (561 minutes for Clinic 1 vs 325 minutes for Clinic 2; P<.001; Mood’s median test) and variability in response time (Levene’s test=26.9; P<.001).
Further comparing differences in time between caregiver groups within both clinics combined regardless of time period (residents [N=5,928], faculty [N=6,656], and nursing [N=16,290]), nursing refilled medications faster than residents and faculty, with residents’ median time 694 minutes, faculty 559 minutes, and nursing 426 minutes (P<.001; Mood’s median test). Table 2 presents results from each clinic by time period and caregiver group. The percentage of refills completed within 48 hours significantly increased between the pre-COVID-19 and COVID-19 pandemic among faculty and nursing in Clinic 1 and residents and faculty in Clinic 2 (Figure 3).
This project outlined the positive impact of a standardized multidisciplinary medication refill protocol with a dedicated refill nurse in family medicine residency clinics. While the number of refills did not decline between prepandemic and during the pandemic periods, we highlighted the fact that a nursing-driven medication refill process can reduce refill request response times, even during such an extraordinary event. Unfortunately, we were only able to analyze overall refill response time through our EMR, not the percentage of refills sent to primary care providers or triage nurses by protocol. Additionally, large standard deviations and variability of refill times were driven by significant outliers. Informal observation indicated that the latter may have been caused by missing information on the initial refill request, requirements that patients be seen for certain refill requests, resident/faculty vacations, resident/faculty assignment to intense inpatient services with decreased clinic time, unusually high clinic visit volumes, and other causes that we were not able to account for. Certainly, and intuitively, complexity of refill requests also may have increased refill time, as evidenced by nurse triage time and interquartile range increases in Phase 1. Despite lower refill volumes and overall clinic refill time decreases with protocol implementation, nurse triage refill assignments were largely requests already delayed or problematic. Moreover, the number of nurses and residents available in Clinic 1 versus Clinic 2 on a given day also may have influenced the outcome of this study.
Improvement in refill time, including percentage of requests completed within 48 hours, and decrease in variability allow for a more reasonable and defined interval for refills to be completed (and for patients to enjoy this improvement and predictability). In the context of an academic clinic, this refill protocol significantly reduced the turnaround time of refill requests that physicians were responsible for and reduced inbox work (and perhaps burnout),10 yet retained the experience of providing physician input, per protocol, for the residents.
In the next phase, expanding the use of such a medication protocol to clinical pharmacists who are comanaging chronic medical conditions may be beneficial.1,4 Pharmacist-led protocols have been suggested to increase safety as well.11 In addition, exploring the impact of medication refill by a nonclinician-driven protocol, perhaps with enhanced clinical decision support,12 on patient satisfaction and overall physician well-being would be helpful.
Acknowledgments
We acknowledge and thank all the nursing staff for their diligence and hard work in rolling out the medication refill protocol, as well as residents and attending physicians for their willingness to learn a new workflow. In addition, we acknowledge the following individuals for contributing to this project: Sara Ward, MD; Caleb Patee, DO, MPH; Raheel Mody, DO; Mark Robinson, DO; Christopher Klink, PharmD; Marianne Klumph, MA; Catherine De Grandville, MD; and Bonnie Bobot, MD.
Presentations: Some of this work was presented externally at the 2020 Society of Teachers of Family Medicine Annual Conference, a virtual meeting August 24-27, 2020, and the virtual 2021 North American Primary Care Conference November 19-21, 2021. Some of this work also was presented internally.
References
- Schlosser EG, Neff E, Francis SM, Vormohr H, Hincapie AL. Implementation of a protocol-driven pharmacy technician refill process at a large physician network. J Am Pharm Assoc. 2020;60(6):e341-e348. doi:10.1016/j.japh.2020.07.006
- Schoenhaus R, Lustig A, Rivas S, Monrreal V Jr, Westrich KD, Dubois RW. Using an electronic medication refill system to improve provider productivity in an accountable care setting. J Manag Care Spec Pharm. 2016;22(3):204-208. doi:10.18553/jmcp.2016.22.3.204
- Guirguis-Blake J, Keppel GA, Force RW, Cauffield J, Monger RM, Baldwin LM. Variation in refill protocols and procedures in a family medicine residency network. Fam Med. 2012;44(8):564-568. https://www.stfm.org/familymedicine/vol44issue8/Guirguis-Blake564
- Rim MH, Thomas KC, Hatch B, Kelly M, Tyler LS. Development and implementation of a centralized comprehensive refill authorization program in an academic health system. Am J Health Syst Pharm. 2018;75(3):132-138. doi:10.2146/ajhp170333
- Shipman SA, Sinsky CA. Expanding primary care capacity by reducing waste and improving the efficiency of care. Health Aff (Millwood). 2013;32(11):1,990-1,997. doi:10.1377/hlthaff.2013.0539
- Andersson K, Melander A, Svensson C, Lind O, Nilsson JL. Repeat prescriptions: refill adherence in relation to patient and prescriber characteristics, reimbursement level and type of medication. Eur J Public Health. 2005;15(6):621-626. doi:10.1093/eurpub/cki053
- Ghorob A, Bodenheimer T. Sharing the care to improve access to primary care. N Engl J Med. 2012;366(21):1,955-1,957. doi:10.1056/NEJMp1202775
- Galt KA, Rule AM, Clark BE, Bramble JD, Taylor W, Moores KG. Best practices in medication safety: areas for improvement in the primary care physician office. In: Henriksen K, Battles JB, Marks ES, Lewin DI, eds. Advances in Patient Safety: From Research to Implementation. Vol. 1. Agency for Healthcare Research and Quality; 2005:101-129.
- Yacoob Z, Cook C, Kotovicz F, et al. Enhancing immunization rates in two urban academic primary care clinics: a before and after assessment. J Patient Cent Res Rev. 2020;7(1):47-56. doi:10.17294/2330-0698.1709
- Hurley-Kim K, Keyvani A, Ahmed R, Wong HW, McBane S. Pharmacist-managed refill service impacts on clinician workload and medication interventions in a federally qualified health center. J Prim Care Community Health. 2023;14. doi:10.1177/21501319231168716
- White N. Reducing primary care provider burnout with pharmacist-delivered comprehensive medication management. Am J Lifestyle Med. 2020;15(2):133-135. doi:10.1177/1559827620976539
- Tokazewski JT, Peifer M, Howell JT III. Leveraging and improving refill protocols at your health system. Appl Clin Inform. 2022;13(5):1,063-1,069. doi:10.1055/a-1947-2556
Lead Author
Samia Khan, DO
Affiliations: Department of Family Medicine, Aurora UW Medical Group, Aurora St. Luke’s Medical Center, Advocate Aurora Health, Milwaukee, WI
Co-Authors
Jessica J. F. Kram, MPH - Academic Affairs, Aurora UW Medical Group, Advocate Aurora Health Care, Aurora Sinai Medical Center, Milwaukee, WI | Center for Urban Population Health, Milwaukee, WI
Dennis J. Baumgardner, MD - Department of Family Medicine, Aurora UW Medical Group, Aurora St. Luke’s Medical Center, Advocate Aurora Health, Milwaukee, WI | Center for Urban Population Health, Milwaukee, WI
Amanda G. Sessions, DO - Department of Family Medicine, Aurora UW Medical Group, Aurora St. Luke’s Medical Center, Advocate Aurora Health, Milwaukee, WI
Patrick Foss, MD - Department of Family Medicine, Aurora UW Medical Group, Aurora St. Luke’s Medical Center, Advocate Aurora Health, Milwaukee, WI
Carl Bellinger, DO - Department of Family Medicine, Aurora UW Medical Group, Aurora St. Luke’s Medical Center, Advocate Aurora Health, Milwaukee, WI
Fabiana Kotovicz, MD - Department of Family Medicine, Aurora UW Medical Group, Aurora St. Luke’s Medical Center, Advocate Aurora Health, Milwaukee, WI
Corresponding Author
Samia Khan, DO
Correspondence: Department of Family Medicine, Aurora UW Medical Group, Aurora St. Luke’s Medical Center, Advocate Aurora Health, Milwaukee, WI
Email: samia.khan@aah.org
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.