Introduction: Nationally, low-income women of Hispanic ethnicity have a significantly higher rate of unintended pregnancy than their White counterparts. This disparity leads to an increased risk for poor maternal and child outcomes that have long and short-term sequelae for health and well-being. A quantitative report in Washtenaw County, Michigan in 2017 found that both men and women were at high risk for unintended pregnancy with many women reporting no contraception use, despite not desiring a pregnancy.
Methods: We used semistructured interviews to assess the opinions and experiences regarding the use of contraception among 21 Hispanic women and men of reproductive age in a Midwestern county.
Results: Our study found that the use of contraception to prevent unwanted pregnancy was important to our sample of Hispanic women and men. However, concerns about side effects, limited knowledge on reproductive health, the influence of partners, and financial barriers played a role in the use of contraception.
Conclusion: Our findings provide insight into the influences and barriers to contraception use among Hispanic women and men and can inform future research.
Nearly half of pregnancies in the United States are unintended, defined as a pregnancy that a woman reports was not desired at the time it occurred.1 Unintended pregnancies are a risk factor for birth defects, preterm birth, and low birth weight.2-5
Specifically, low-income women of Hispanic ethnicity experience a significantly higher rate of unintended pregnancy (58%) compared to their White counterparts (33%).4 Factors associated with higher rates of unintended pregnancy among Hispanic women include lower age, non-US-born status, lower education, unmarried, lower English language proficiency, perceptions of contraceptive methods, and religious/cultural beliefs.6-8 However, these studies have mainly focused on women’s experiences,3,8,9 and typically are from samples from large cities, such as Chicago, Miami, New York, and Los Angeles, rather than smaller communities where a large proportion of Hispanic individuals live.10
A quantitative report examining pregnancy intentions among Hispanic persons found that many women reported no contraception use, despite not desiring a pregnancy. 11 The aim of this qualitative study was to characterize specific barriers to contraception use among Hispanic women and men of childbearing age in Washtenaw County, Michigan, a county that includes urban, suburban and rural regions located in the Midwest region of the United States. Understanding these factors is critical to creating effective policies and practices that support the health and well-being of Hispanic women, men, and their families.
Design and Setting
We used a qualitative design employing semistructured qualitative interviews. This study was approved by the University of Michigan’s Institutional Review Board and written informed consent was obtained from all participants. Participants were recruited from Washtenaw County, Michigan between March and May 2017.
Participants and Recruitment
Inclusion criteria were as follows: women and men between ages 18-49 years (reproductive age), living in Washtenaw County, and identifying as Hispanic or Latino. A convenience sample of participants was recruited from a primary care clinic using flyers distributed upon check-in for a clinic visit. Eligible and interested participants were asked to complete an in-person interview in a private room after their clinic visit or were contacted by telephone for an interview at a later time, if preferred. Participants received a $10 incentive for participating.
Data Collection
Bilingual medical students conducted semistructured interviews in person or by phone in English or Spanish based on the participant’s preference. Interviewers followed a standard interview guide developed by the investigators. Responses to open-ended questions elicited participant demographic information and perspectives on sexual health, pregnancy and contraception use.12 All interviews were audio-recorded.
Data Analysis
We transcribed interviews verbatim and reviewed them for accuracy. We first open coded the text inductively, using techniques described by Corbin and Strauss.13 Each transcript was reviewed by two investigators, line-by-line, to identify prominent concepts and ideas to draft preliminary coding categories. Preliminary codes were then reviewed and discussed in person by the entire author team and a detailed codebook defining each code was created. Each transcript was then coded by at least two authors using the codebook and discrepancies in coding were discussed in person to reach consensus. We identified major themes through discussion and identified representative quotes.
All transcripts were analyzed in the language the interview was conducted as all investigators are fluent in both languages. Illustrative quotes included in the manuscript that were in Spanish were translated into English.
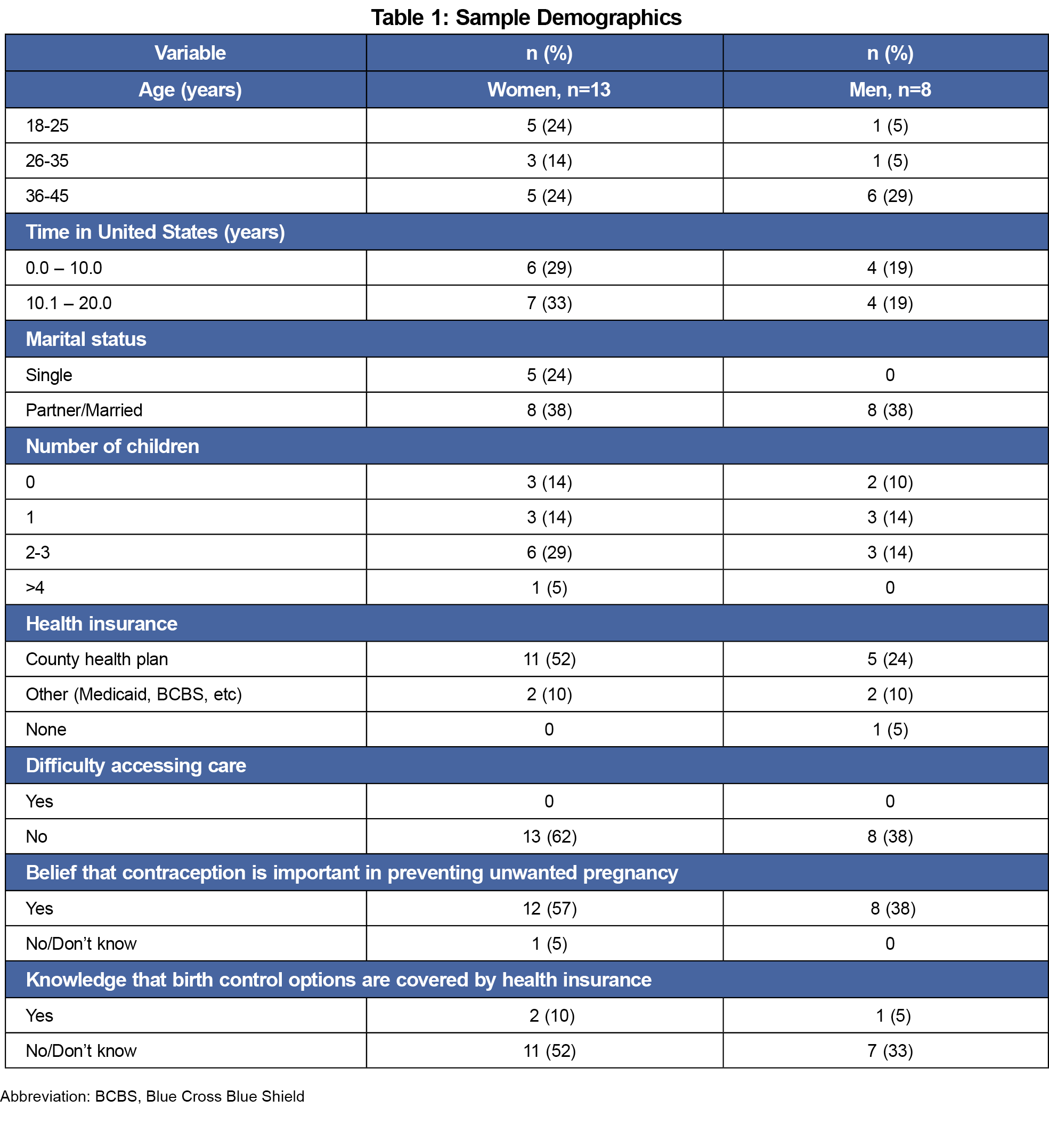
Our sample included 21 participants from Washtenaw County, Michigan. Thirteen identified as women and eight identified as men with a mean age of 33.3 years (SD 8.7). All participants identified as Hispanic/Latino(a) and have lived in the United States for an average of 9.5 years (range: 0.3–20 years). No participant expressed difficulty accessing health care, but only three participants (14%) knew that their health insurance covered the cost of contraception (Table 1). The duration of interview sessions ranged from 13:27 to 38:20 minutes with a median time of 23:38 minutes.
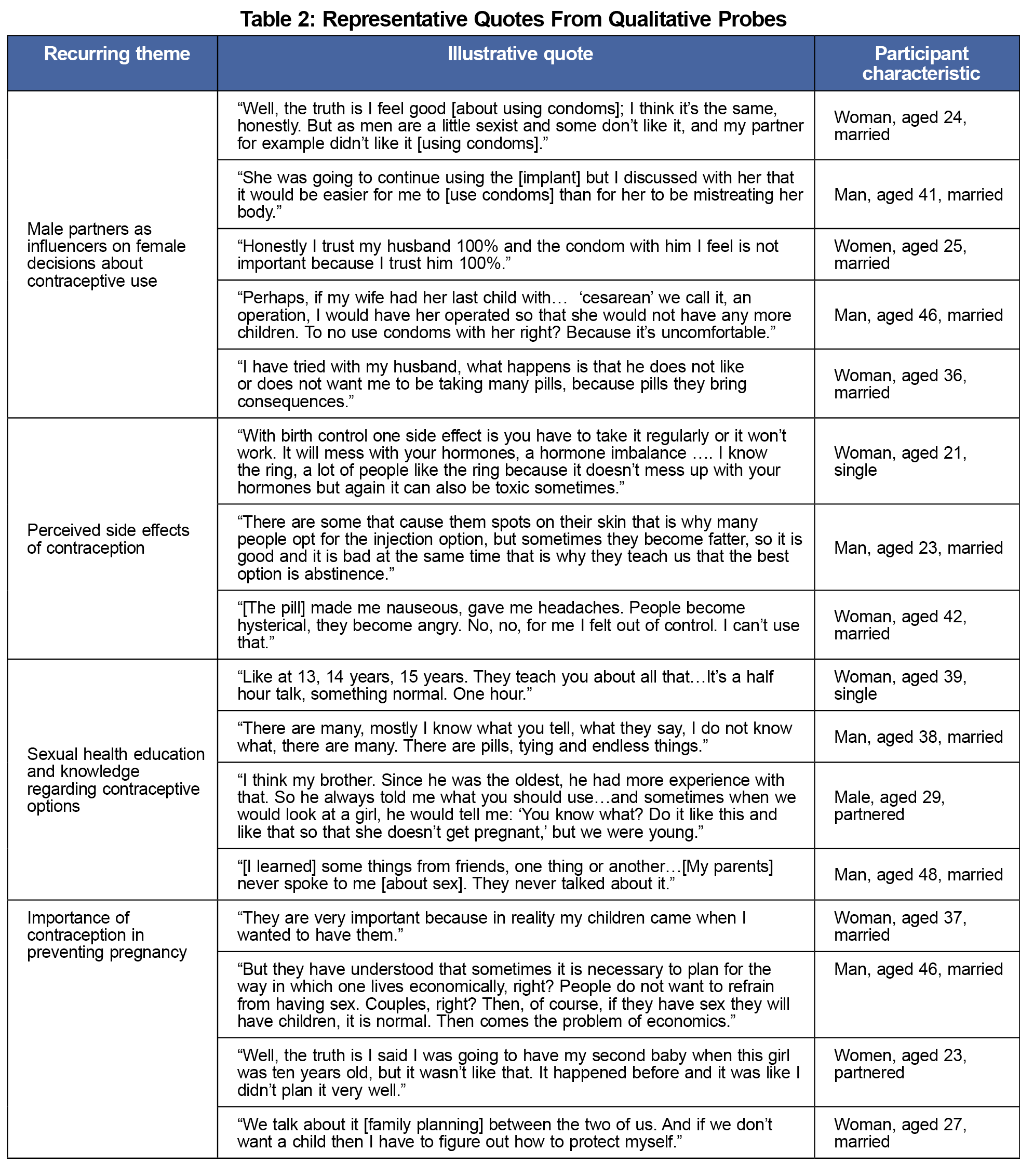
Our results showed that all participants affirmed the importance of planning pregnancy. Most men and women (20/21) believed contraception to be very important in preventing unwanted pregnancies. Participants reported using condoms (11), oral contraceptive pills (6), intrauterine device (6), contraceptive injection (5), implant (2) and patch (1). Oral contraceptive pills (4) and condoms (3) were the most preferred forms of contraception though less than half of the respondents (10/21) reported having a preference. Both men and women cited concern for side effects, perceived and experienced. While many respondents received some form of education on sexual health from their country of origin, participants felt this education to be inadequate. Male partners’ opinions appeared to impact female decisions about contraceptive use (Table 2). Interpersonal relationships (partners, family), cultural (including family background and religion), and financial factors were reported by both men and women to influence family planning and decisions regarding contraceptive choice (Table 2).
Among our sample of 21 Hispanic men and women, we found that the opinions of men influenced contraceptive decisions among women. This finding is similar to other studies, particularly studies of populations outside of the United States.14,15 Because male partners are so influential in this population, it may be beneficial to encourage female patients to invite male partners to participate in the health care visits of women when discussing contraception. Current contraceptive counseling practice includes discussion of different methods as well as the patient’s values and preferences,16 but does not specifically recommend engaging male partners.
Similar to other studies, concerns about side effects were a major barrier to contraceptive use.7,17 Although discussion of side effects is recommended during contraception counseling,16 contraceptive providers do not always discuss side effects with patients.18 Among Hispanic patients, these discussions are particularly important as they may dispel myths and provide critical information needed to inform contraceptive decisions, as many participants also noted that contraception education in their home countries was limited. 7
We also noted financial barriers. Nearly all participants (n=20/21) had health insurance, though few (3/21) knew that their health insurance plan covered contraception. Language concordant information on insurance coverage may alleviate concerns about the affordability of contraception in this population.
One of the limitations in our study is internal validity due to not achieving theme saturation. As mentioned previously, we are all fluent in both English and Spanish and are qualified to provide medical care to Spanish speakers without a translator. While this allowed for a deeper connection and understanding of participants, it can create a potential bias when interpreting the data due to preconceived notions of researchers. Of note, Spanish quotations included in this manuscript were reviewed and translated by the investigators of the study and not by a professional translator. An additional limitation is a delay in the publication of results due to the COVID-19 pandemic, consequently the data presented is prepandemic and pre-Roe overturn.19 Finally, all participants in our sample identified as cis-gender and most report being married or coupled, which limits generalizability among those who do not match these characteristics.
In conclusion, our study found that the use of contraception to prevent unwanted pregnancy was important to our sample of Hispanic patients. However, concerns about side effects, limited knowledge on reproductive health, the influence of partners and financial barriers played a role in the use of contraception.
References
- Guttmacher Institute. Unintended pregnancy in the United States. 2019. Accessed May 12, 2022. https://www.guttmacher.org/fact-sheet/unintended-pregnancy-united-states
- Jackson AV, Wang LF, Morse J. Racial and ethnic differences in contraception use and obstetric outcomes: a review. Semin Perinatol. 2017;41(5):273-277. doi:10.1053/j.semperi.2017.04.003
- Hall JA, Benton L, Copas A, Stephenson J. Pregnancy intention and pregnancy outcome: systematic review and meta-analysis. Matern Child Health J. 2017;21(3):670-704. doi:10.1007/s10995-016-2237-0
- Finer LB, Zolna MR. Declines in unintended pregnancy in the United States, 2008-2011. N Engl J Med. 2016;374(9):843-852. doi:10.1056/NEJMsa1506575
- American College of Obstetricians and Gynecologists’ Committee on Health Care for Underserved Women. 654: reproductive life planning to reduce unintended pregnancy. Obstet Gynecol. 2016;127(2):e66-e69. doi:10.1097/AOG.0000000000001314
- Unger JB, Molina GB. Acculturation and attitudes about contraceptive use among Latina women. Health Care Women Int. 2000;21(3):235-249. doi:10.1080/073993300245285
- Sangi-Haghpeykar H, Ali N, Posner S, Poindexter AN. Disparities in contraceptive knowledge, attitude and use between Hispanic and non-Hispanic whites. Contraception. 2006;74(2):125-132. doi:10.1016/j.contraception.2006.02.010
- Kim TY, Dagher RK, Chen J. Racial/Ethnic differences in unintended pregnancy: evidence from a national sample of U.S. women. Am J Prev Med. 2016;50(4):427-435. doi:10.1016/j.amepre.2015.09.027
- Masinter LM, Feinglass J, Simon MA. Pregnancy intention and use of contraception among Hispanic women in the United States: data from the National Survey of Family Growth, 2006-2010. J Womens Health (Larchmt). 2013;22(10):862-870. doi:10.1089/jwh.2013.4366
- The Brookings Institute; Center on Urban & Metropolitan Policy and the Pew Hispanic Center. Latino growth in metropolitan America: changing patterns, new locations. Accessed May 11, 2022, https://www.brookings.edu/wp-content/uploads/2016/06/surosinger.pdf
- Hughey KL, Llanes M, Plegue M, et al. Risk for unintended pregnancy among Latino men and women in a nonmetropolitan county in Michigan. PRiMER Peer-Rev Rep Med Educ Res. 2017;1:21. doi:10.22454/PRiMER.2017.651218
- Scruggs E, Hughey K, Crespo Albiac L, Martin E, Llanes M. Interview Guide (English/(Spanish). STFM Resource Library. Accessed May 11, 2022. https://resourcelibrary.stfm.org/viewdocument/interview-guide-englishspanish?CommunityKey=2751b51d-483f-45e2-81de-4faced0a290a
- Corbin J, Strauss A. Grounded Theory Research: Procedures, canons, and evaluative criteria. Qual Sociol. 1990;13(1):3-21. doi:10.1007/BF00988593
- Kriel Y, Milford C, Cordero J, et al. Male partner influence on family planning and contraceptive use: perspectives from community members and healthcare providers in KwaZulu-Natal, South Africa. Reprod Health. 2019;16(1):89. doi:10.1186/s12978-019-0749-y
- Comfort AB, Harper CC, Tsai AC, et al. The association between men’s family planning networks and contraceptive use among their female partners: an egocentric network study in Madagascar. BMC Public Health. 2021;21(1):209. doi:10.1186/s12889-021-10180-6
- American College of Obstetricians and Gynecologists (ACOG). Patient-centered contraceptive counseling. Accessed May 13, 2022, https://www.acog.org/-/media/project/acog/acogorg/clinical/files/committee-statement/articles/2022/02/patient-centered-contraceptive-counseling.pdf
- Gilliam ML, Warden M, Goldstein C, Tapia B. Concerns about contraceptive side effects among young Latinas: a focus-group approach. Contraception. 2004;70(4):299-305. doi:10.1016/j.contraception.2004.04.013
- Dehlendorf C, Levy K, Ruskin R, Steinauer J. Health care providers’ knowledge about contraceptive evidence: a barrier to quality family planning care? Contraception. 2010;81(4):292-298. doi:10.1016/j.contraception.2009.11.006



There are no comments for this article.