Point-of-care ultrasound (POCUS) has the potential to revolutionize medical practice, yet many barriers limit widespread use. POCUS supports diagnosis and procedures, and according to the American Academy of Family Physicians (AAFP), “may be the biggest advance in bedside diagnosis since the advent of the stethoscope.”1,2 POCUS training is becoming increasingly prevalent in family medicine residencies and will be required by the Accreditation Council for Graduate Medical Education (ACGME) in 2023.3,4 POCUS training modalities and competency assessment vary widely, and residencies must determine their own scope of training and curricula.1-3 Barriers to clinical use include limited funding, limited time to train faculty, limited equipment access, difficulty establishing billing, and discomfort with image interpretation.5 To better understand usefulness of current POCUS curricula, educational needs, practice trends, and relevance to future practice, we surveyed family medicine residents, faculty, and recent graduates of the University of Missouri Family & Community Medicine (MUFCM) regarding their interest, level of training, perceived barriers, and current POCUS application.
RESEARCH BRIEF
Point-of-Care Ultrasound Attitudes, Barriers, and Current Use Among Family Medicine Residents and Practicing Physicians
Alicia Ludden-Schlatter, MD, MSAM | Robin L. Kruse, PhD, MSPH | Reiana Mahan, MD | Luke Stephens, MD, MSPH
PRiMER. 2023;7:13.
Published: 4/26/2023 | DOI: 10.22454/PRiMER.2023.967474
Introduction: Point-of-care ultrasound (POCUS) has high interest among learners and educators, but many barriers inhibit training and clinical use. Interest and barriers may differ between educators, trainees, and practicing physicians. This study investigates interest in POCUS, confidence in POCUS skills, and barriers to POCUS use for residents, academic family physicians, and community providers.
Methods: Online surveys sent to current residents, faculty, and graduates of an academic family medicine residency compared current use, comfort, training, perceived importance, barriers, and interest in future use of POCUS.
Results: Most participants (95.6%) agreed that POCUS was somewhat or extremely important to family medicine. Most participants also reported interest in all POCUS indications, other than obstetrics. Very few (5.4%) reported being extremely comfortable using POCUS. Most residents were somewhat comfortable, whereas most faculty and graduates were not at all comfortable. A majority in each group reported inexperience with equipment and interpreting images as a barrier. One-third of faculty and graduates reported “not billable” as a barrier. Statistically significant differences were found between groups’ reports of prior training, current use, and interest in POCUS for obstetrics.
Conclusions: Family medicine residents, faculty, and community physicians reported high perceived importance of and interest in nonobstetric POCUS, but low comfort level in performing POCUS. Resident and faculty barriers may vary according to practice environment and differing time constraints. Senior faculty may have less POCUS training and comfort using POCUS than residents, highlighting the importance of continuing faculty education.
MUFCM residents and faculty practice at rural clinics, urban clinics, or a federally qualified health center. Residents rotate on outpatient, inpatient, and obstetric services managed by family medicine and other specialties. Since 2018, resident didactic seminars included monthly hour-long POCUS workshops with lectures and hands-on sessions, led by two faculty. Attendance is excused for vacation and clinical care responsibilities. Since 2019, faculty have received one to two POCUS training sessions per year.
We created a Qualtrics survey to assess use, comfort, training, perceived importance, barriers, and interest in future use of POCUS. Items rating importance and comfort were scored as 1: extremely, 2: somewhat, and 3: not at all.5 The survey was reviewed by two senior faculty for clarity and accuracy of language. We emailed the survey to all MUFCM faculty, 2014-2019 graduates employed elsewhere, and residents in spring 2020 and to new PGY1s in fall 2020. We sent one reminder email to all participants. We offered no incentives, and response was anonymous and voluntary.
Survey data were imported into SAS for Windows 9.4 (SAS Institute, Cary, NC). We calculated simple frequencies for each item. For ranked data, we used the Kruskal-Wallis test to determine whether responses were from the same distribution. Post hoc tests were performed between groups when the initial test was statistically significant. We analyzed yes/no responses with the χ2 test. When expected cell counts were <5, we used the Fisher’s exact test. This study was exempted by the University of Missouri Health Sciences Institutional Review Board.
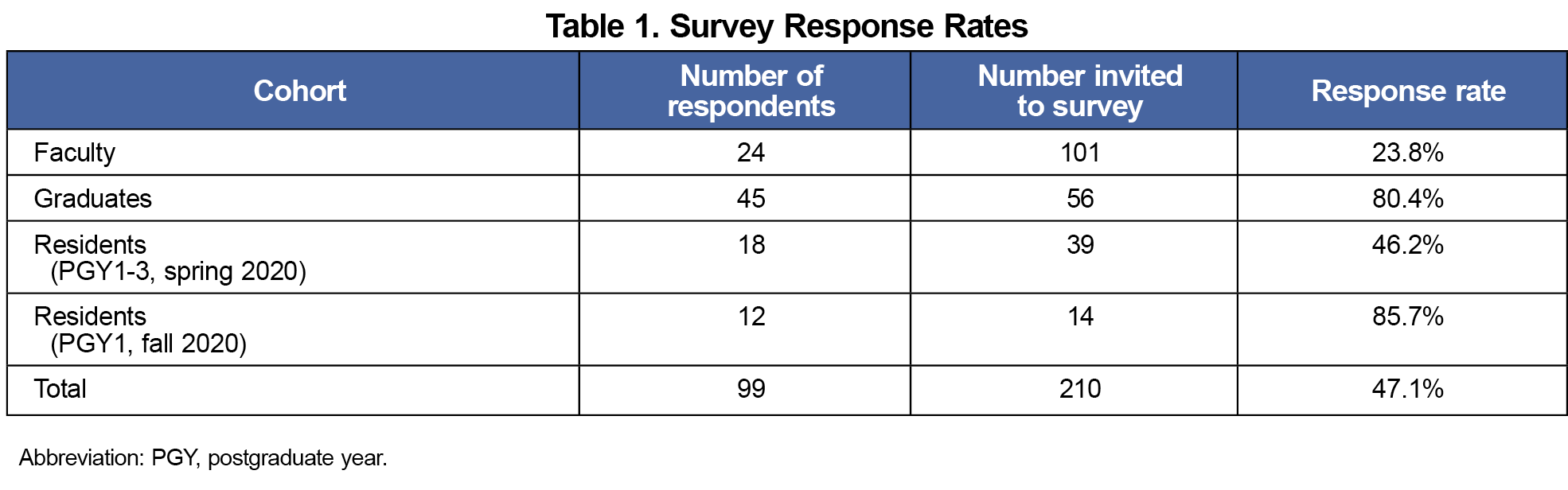
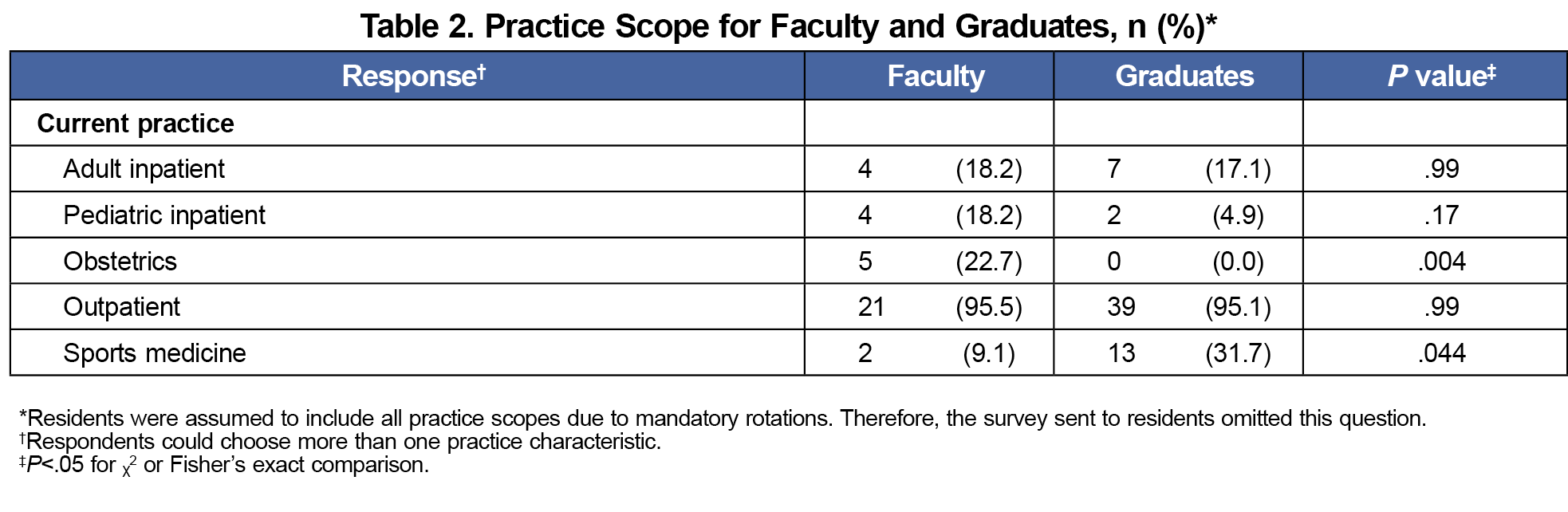
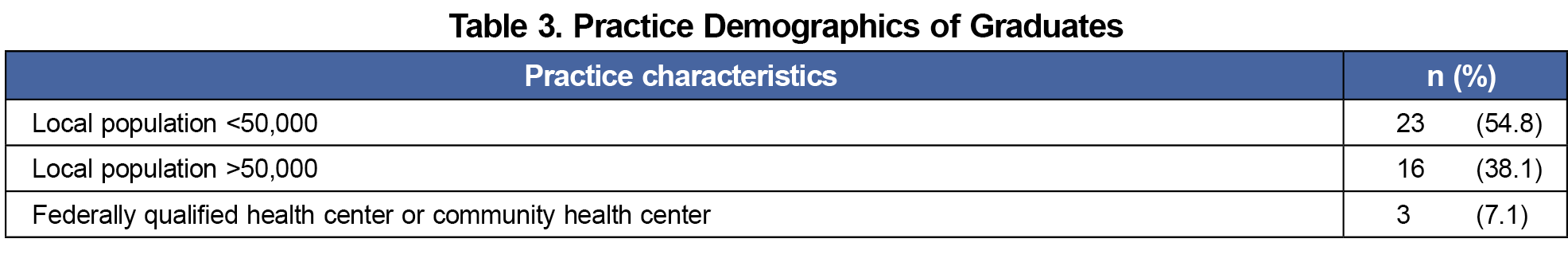
The overall survey response rate was 47.1% (Table 1). Responder characteristics are reported in Tables 2 and 3. Most respondents practiced outpatient medicine. Only 22.7% of faculty and no graduates practiced obstetrics.
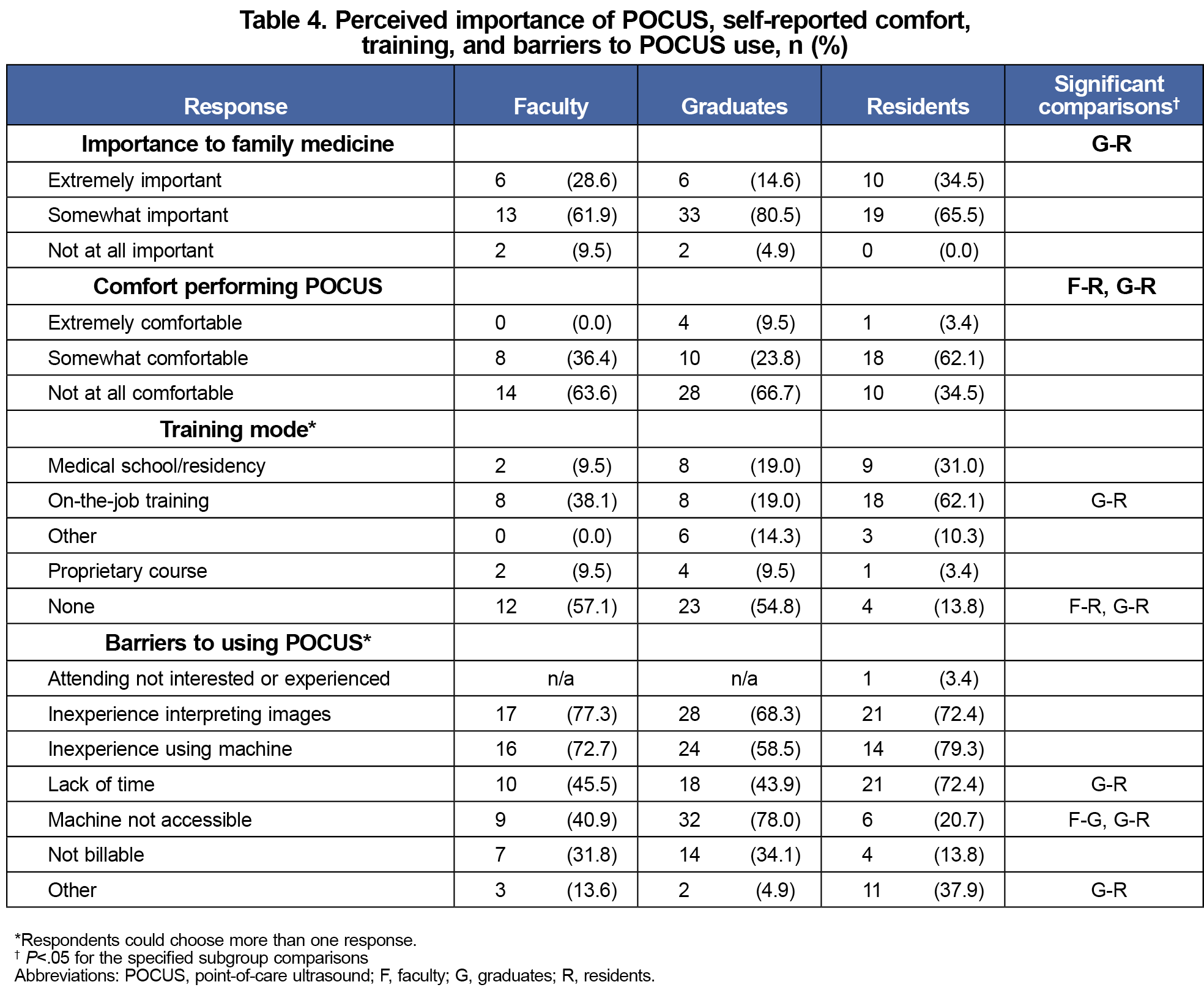
Most participants (95.6%) agreed that POCUS was somewhat or extremely important to family medicine (Table 4). Very few respondents (5.4%) reported being extremely comfortable using POCUS. Most residents reported being somewhat comfortable, while most faculty and graduates were not at all comfortable. More than half of faculty and graduates reported no POCUS training, compared with only 13.8% of residents. More residents (62.1%) than faculty (38.1%) or graduates (19.0%) reported on-the-job training.
Respondents reported several barriers to POCUS use. A majority in all groups reported inexperience interpreting images or using the machine. More residents cited lack of time (72.4%) than graduates (43.9%). Most graduates (78.0%) cited lack of machine access, compared with 40.9% of faculty and 20.7% of residents.
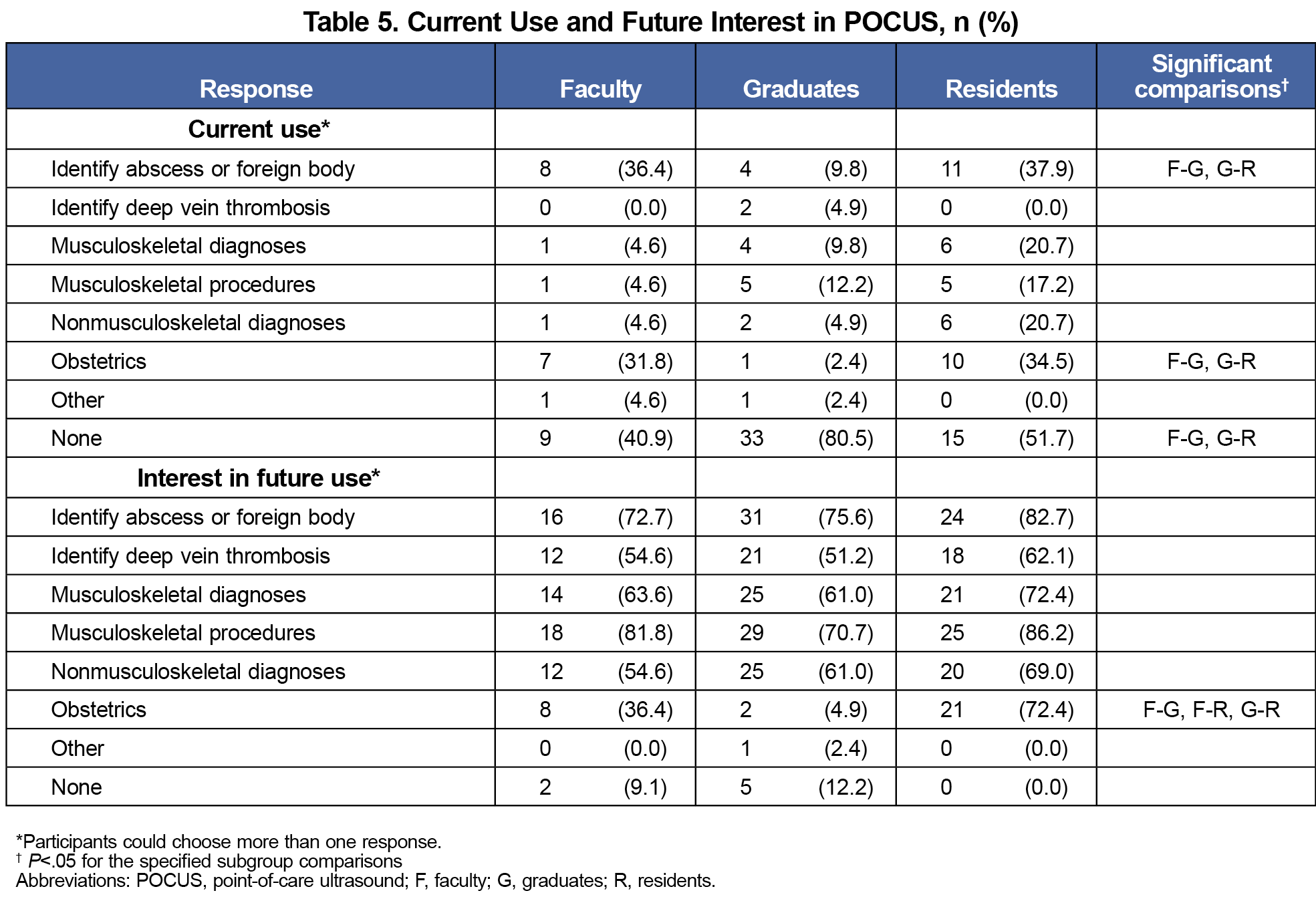
More than 80% of graduates reported no current POCUS use, compared with 40.9% of faculty and 51.7% of residents (Table 5). Approximately one-third of faculty and residents used POCUS for obstetrics, compared with 2.4% of graduates. More than one-third of residents and faculty used POCUS to identify an abscess or foreign body compared to 9.8% of graduates.
Interest in future POCUS use was high, with most choices endorsed by more than half of participants. Interest was similar across groups except for obstetrics, where all three groups differed from each other.
POCUS training is rapidly expanding in family medicine. In 2019, 6% of family medicine programs had established POCUS curricula. This proportion jumped to 32% in 2021.6 As of July 2023, all family medicine residents will be expected to have experience using POCUS in clinical care.3 Educational efforts to develop or refine skills must begin with assessments of current attitudes and competency. To our knowledge, this survey is the first to directly compare perceptions regarding POCUS among faculty, trainees, and graduates. Our survey, like others in this area, indicates high interest in and perceived importance of POCUS for diagnosis and treatment of many conditions.6,7 Barriers to POCUS use differed by group; graduates disproportionately cited lack of machine accessibility and residents cited lack of time.
Obstetric POCUS had the largest discrepancy in interest between subgroups, which may reflect low rates of obstetric practice among faculty and graduates versus required rotations in residency. Nationally, rates of family medicine obstetric practice have been declining for many years.8 Therefore, obstetric POCUS may become less applicable among family physicians.
Approximately one-third of our faculty and graduates cited “not billable” as a barrier. According to 2012-2017 Medicare claims, only 9.3% of primary care physicians billed for ambulatory POCUS services.9 In a survey of family medicine chairs, 32% of departments had a POCUS curriculum, only 6% had established billing, and 73% reported difficulty with establishing billing.6 Billing practice correlated with increasing number of POCUS-trained faculty. Whether more widespread POCUS training may lead to increased billing, or whether billing is necessary to promote POCUS use, remains to be seen. Regardless, our survey indicates lack of POCUS billing as a notable, if not primary, barrier for community and faculty physicians.
Inexperience with POCUS was endorsed by a majority in all subgroups. POCUS training increases both trainee confidence and competency.7,10 Many POCUS training courses exist, with widely varying scope, didactic modalities, and training hours.1 The AAFP’s curriculum guidelines for POCUS training leave specifics regarding scope and curriculum design to the discretion of individual residencies.2 Our residents reported a much higher rate of POCUS training than faculty, likely reflecting our residency’s monthly, mandatory POCUS workshops. These workshops occur during protected educational time. Graduates of the 2018-2019 classes had POCUS workshops in residency, whereas 2014-2017 graduates did not. Faculty POCUS workshops occur much less frequently. This discrepancy reflects a national dilemma, in which residencies will be required to provide POCUS training, although senior faculty will likely be novices. Nationally, family medicine chairs have reported limited training time as the largest barrier to increasing numbers of trained POCUS faculty, and time and/or funding to train faculty as the most useful means to increase POCUS use.5 This survey highlights the importance of protected time and resources for continuing faculty education.
This study has several limitations. Surveys were sent to affiliates of a single institution. Response rates for the faculty cohort were low, which may be due to inclusion of nonclinical faculty on the survey invitations. Responders may have higher interest in POCUS than nonresponders. Despite a small sample size, significant differences were found in practice patterns, prior training, and barriers to use, similar to national trends.7,11 More than half of faculty reported no prior training, which reflects the need to train faculty in new skill sets—a common dilemma.12 Finally, this cross-sectional survey assesses self-rated confidence, which does not necessarily correlate with competence. This survey should not be interpreted with respect to competence or diagnostic accuracy.
Residencies planning and revising POCUS curricula must consider available resources, faculty skills, and the future practice needs of their learners. This survey provides insight into interest in POCUS according to trainees, faculty, and community physicians, and elucidates the unique barriers that limit POCUS in these groups. This survey is consistent with others that indicate universally high interest in nonobstetric POCUS, but barriers to POCUS implementation including lack of time, difficulty with billing, and faculty inexperience.6,12 This and future surveys may guide the recommended scope of POCUS in primary care and support advocacy for increased POCUS funding and training for current and future providers.
Acknowledgments
The authors thank Gwen Wilson, MLS, AHIP, for management of citations.
References
- Andersen CA, Holden S, Vela J, Rathleff MS, Jensen MB. Point-of-care ultrasound in general practice: a systematic review. Ann Fam Med. 2019;17(1):61-69. doi:10.1370/afm.2330
- American Academy of Family Physicians. Recommended curriculum guidelines for family medicine residents: point of care ultrasound. AAFP Reprint No. 290D. Published 2016. Accessed November 15, 2022. https://www.aafp.org/dam/AAFP/documents/medical_education_residency/program_directors/Reprint290D_POCUS.pdf
- Accreditation Council for Graduate Medical Education. ACGME program requirements for graduate medical education in family medicine. Published 2022. Accessed November 24, 2022. https://www.acgme.org/globalassets/pfassets/programrequirements/120_familymedicine_2023.pdf
- Hall JWW, Holman H, Barreto TW, et al. Point-of-care ultrasound in family medicine residencies 5-year update: A CERA study. Fam Med. 2020;52(7):505-511. doi:10.22454/FamMed.2020.223648
- Ludden-Schlatter A, Robin K, Mahan R, et al. Survey regarding point of care ultrasound attitudes, barriers, and current use among family medicine residents and practicing physicians. Published 2022. Accessed January 28, 2023. https://resourcelibrary.stfm.org/viewdocument/survey-regarding-point-of-care-ultr?CommunityKey=2751b51d-483f-45e2-81de-4faced0a290a&tab=librarydocuments
- Capizzano JN, O’Dwyer MC, Furst W, et al. Current state of point-of-care ultrasound use within family medicine. J Am Board Fam Med. 2022;35(4):809-813. doi:10.3122/jabfm.2022.04.220019
- Johnson J, Stromberg D, Willims B, Greenberg N, Myers O. Point-of-care ultrasound for family medicine residents: attitudes and confidence. Fam Med. 2021;53(6):457-460. doi:10.22454/FamMed.2021.930080
- Barreto T, Peterson LE, Petterson S, Bazemore AW. Family physicians practicing high-volume obstetric care have recently dropped by one-half. Am Fam Physician. 2017;95(12):762.
- Niblock F, Byun H, Jabbarpour Y. Point-of-care ultrasound use by primary care physicians. J Am Board Fam Med. 2021;34(4):859-860. doi:10.3122/jabfm.2021.04.200619
- Bornemann P. Assessment of a novel point-of-care ultrasound curriculum’s effect on competency measures in family medicine graduate medical education. J Ultrasound Med. 2017;36(6):1205-1211. doi:10.7863/ultra.16.05002
- Bahner DP, Goldman E, Way D, Royall NA, Liu YT. The state of ultrasound education in U.S. medical schools: results of a national survey. Acad Med. 2014;89(12):1681-1686. doi:10.1097/ACM.0000000000000414
- Micks T, Braganza D, Peng S, et al. Canadian national survey of point-of-care ultrasound training in family medicine residency programs. Can Fam Physician. 2018;64(10):e462-e467.
Lead Author
Alicia Ludden-Schlatter, MD, MSAM
Affiliations: University of Missouri Department of Family and Community Medicine, Columbia, MO
Co-Authors
Robin L. Kruse, PhD, MSPH - University of Missouri Department of Family and Community Medicine, Columbia, MO
Reiana Mahan, MD - University of Missouri Department of Family and Community Medicine, Columbia, MO
Luke Stephens, MD, MSPH - University of Missouri Department of Family and Community Medicine, Ashland, MO
Corresponding Author
Alicia Ludden-Schlatter, MD, MSAM
Correspondence: Family Medicine-South Providence, 551 Veterans United Drive, Columbia, MO 65201. 573-884-7733.
Email: luddena@health.missouri.edu
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.