Introduction: Considering increasing rates of tick-borne diseases (TBDs) in the United States, we investigated the scope of continuing medical education (CME) available to physicians on these infections.
Methods: We surveyed online medical board and society databases serving front-line primary and emergency/urgent care providers for the availability of TBD-specific CME between March 2022 and June 2022. We recorded and analyzed opportunity title, author, web address, publication year, learning objectives, CME credit values, and CME credit type.
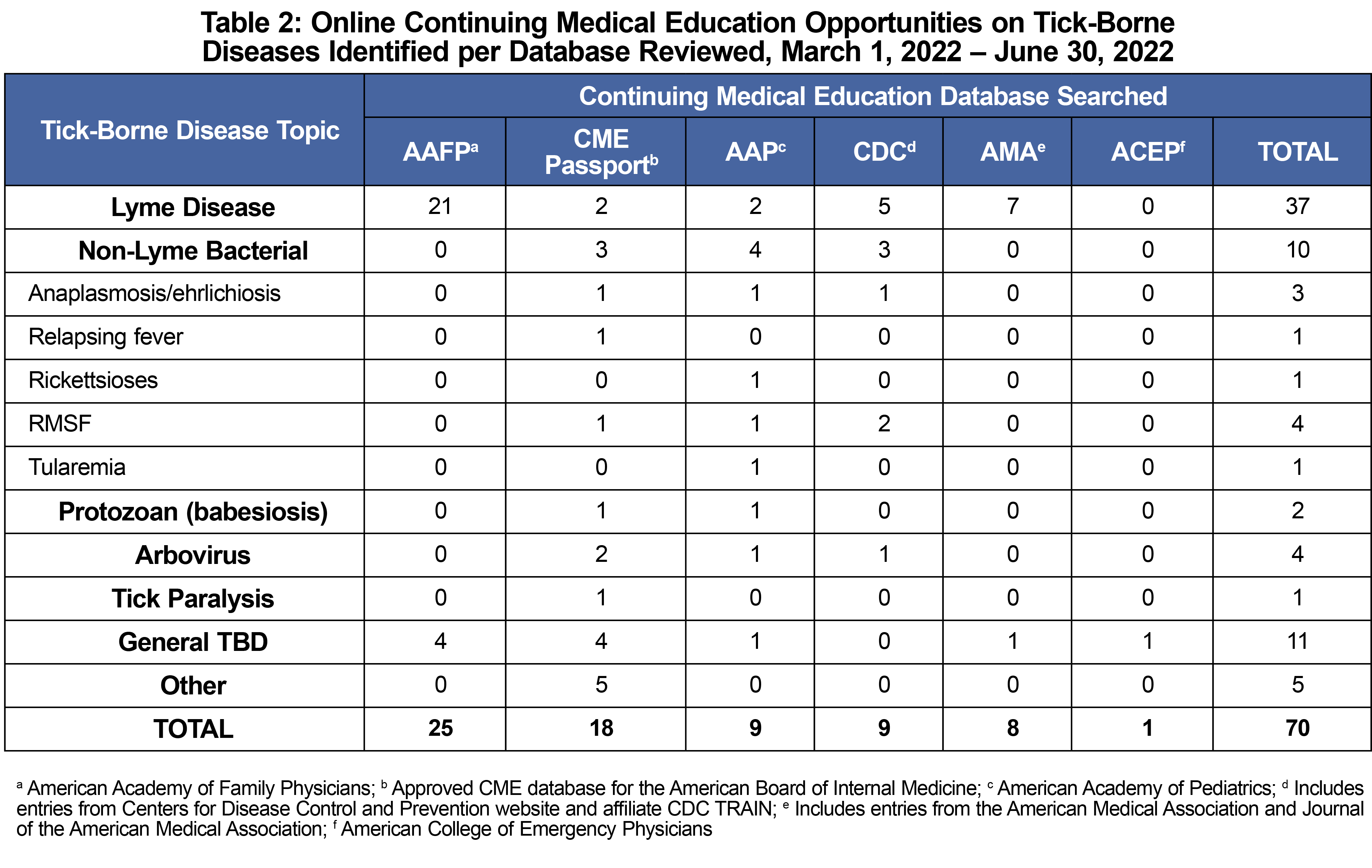
Results: We identified 70 opportunities across seven databases. Thirty-seven opportunities focused on Lyme disease; 17 covered nine non-Lyme TBDs, and 16 covered general topics on TBDs. Most activities were hosted through family medicine and internal medicine specialty databases.
Conclusion: These findings suggest limited availability of continuing education for multiple life-threatening TBDs of increasing importance in the United States. Increasing the availability of CME materials covering the broad scope of TBDs in targeted specialty areas is essential for increased content exposure and a necessary step to ensure our clinical workforce is adequately prepared to address this growing public health threat.
Tick-borne diseases (TBDs) are caused by bacterial, viral, and parasitic disease agents transmitted to humans via the bite of an infected tick. At least 12 different TBDs can be transmitted to humans in the United States and incidence of TBDs more than doubled between 2004 and 2016.1 There remains limited recognition and diagnosis of TBDs in clinical spaces, which can contribute to increased morbidity and mortality.2–7
Medical professionals update, maintain, and increase their clinical knowledge through continuing medical education (CME) opportunities.8 Establishing a baseline for the availability of TBD-focused CME can augment the development and promotion of responsive training. We conducted a scoping review of available online CME opportunities regarding TBD diagnosis and treatment as a first step to characterizing the TBD continuing education landscape in the United States.
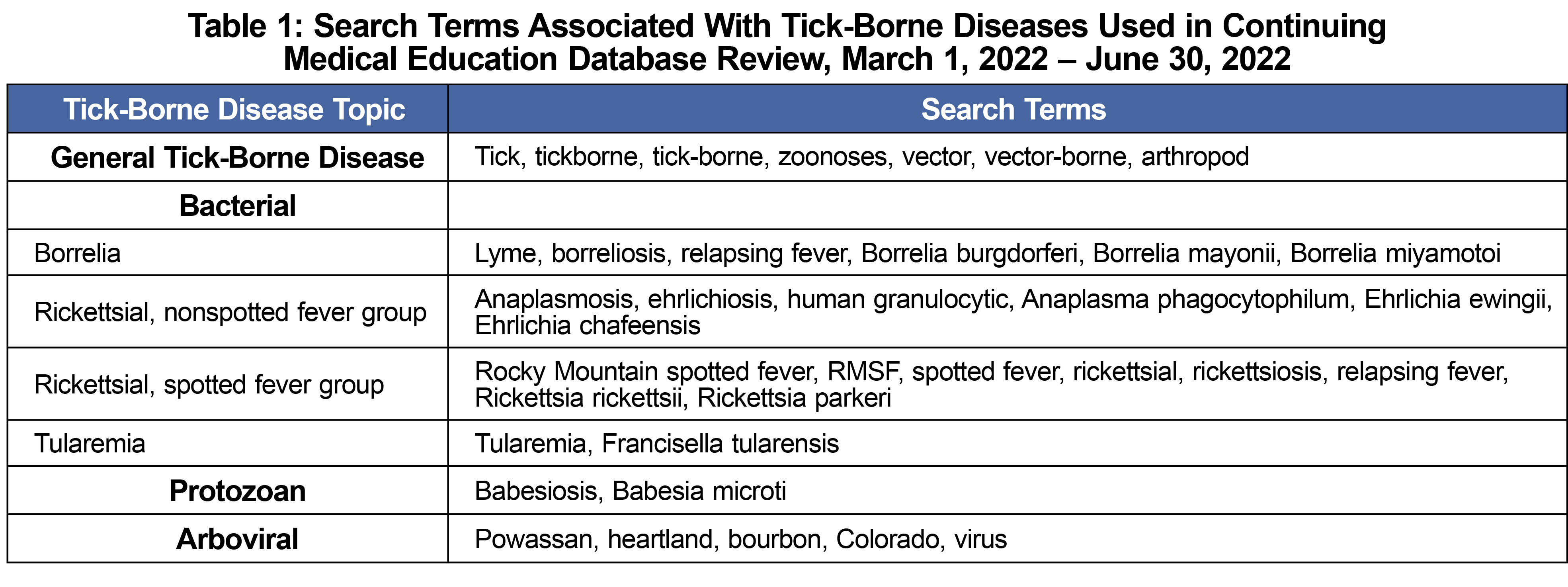
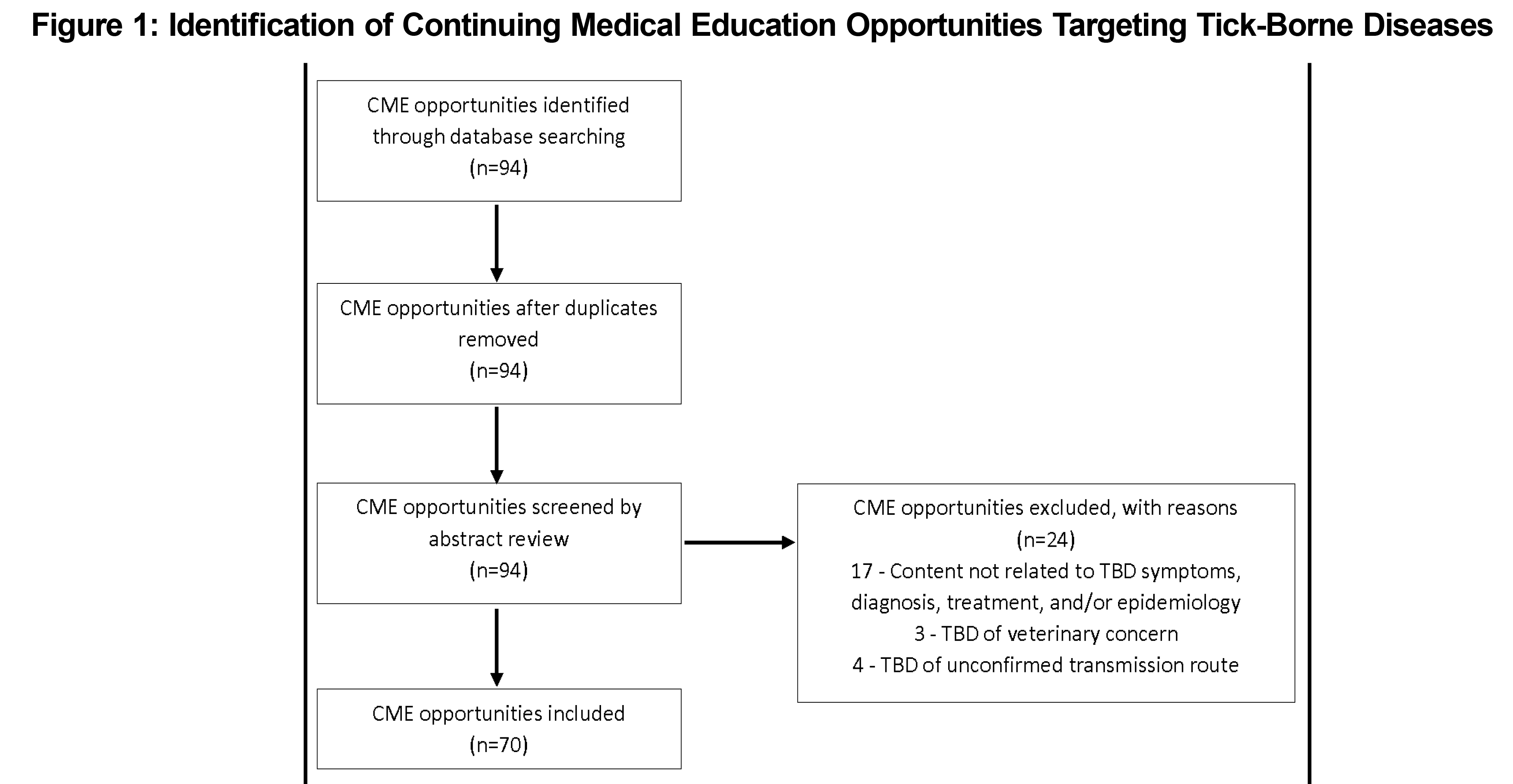
We conducted a scoping search for TBD-specific CME across online databases maintained by medical specialty board and association websites serving front-line providers. We defined front-line providers to include specialties of family medicine, pediatrics, internal medicine, emergency, and urgent care. Our list of databases targeted for CME searches was reviewed by two infectious disease physicians for comprehensiveness and applicability (see Table 2). We then searched the identified CME databases between March 1, 2022 and June 30, 2022 for the availability of TBD-specific CME using a series of predefined search terms (Table 1) informed by a list of concerning TBDs in the United States developed by the American Academy of Family Physicians (AAFP).9,10 Search terms incorporated the following TBDs: Lyme disease, Rocky Mountain spotted fever (RMSF), anaplasmosis, ehrlichiosis, babesiosis, Powassan virus, Colorado tick fever virus, tularemia, and tick-borne relapsing fever. Opportunities were included in the review if their learning objectives incorporated one or more of the following topics: TBD symptoms, diagnosis, treatment, or epidemiology. Opportunities were excluded if they covered TBDs of exclusively veterinary concern or diseases that do not have confirmed tick-borne transmission routes. Due to paywall restrictions, inclusion/exclusion criteria and full data extraction were applied only to the prepayment course abstracts. Online CME databases not affiliated with a medical specialty board were not searched due to the inability to fully review course learning objectives prepayment, with the exception of the database maintained by the Centers for Disease Control and Prevention. We recorded the opportunity title, author, web address, publication year, learning objectives, CME credit values, and CME credit type.
Online searches identified 94 CME opportunities across seven CME databases. We excluded 24 courses after abstract review (Figure 1), resulting in 70 opportunities targeting TBDs (Table 2).
The activities ranged in credit value from 0.25 credits to 19.00 credits, with a median credit value of 1.00 credits. All identified opportunities were enduring material activities. Forty-three percent of opportunities identified were online modules, and 21% were nonmodule self-study activities. Most opportunities (61%) carried no cost, while those with access fees ranged between $25 and $2,199 (Table 3).
Most opportunities carried accreditation through either the AAFP (31%, n=22) or American Medical Association PRA Category 1 Credit (47%, n=33). The AAFP hosted the highest number of opportunities (36%), followed by CME Passport of the American Board of Internal Medicine (26%).
Roughly half of the identified CME opportunities (n=37) specifically focused on Lyme disease. Review of course abstracts indicated that of these, 50% mentioned symptoms and diagnosis, with 27.8% of those explicitly discussing the erythema migrans lesion. In addition, 25% of Lyme-specific CME discussed ticks or tick biology, and 25% reviewed the role of antimicrobials in treatment. Three opportunities discussed posttreatment manifestations of Lyme disease, six mentioned the epidemiology of Lyme disease, and four discussed recognition of the transmission route or vector. Six opportunities reviewed interpersonal roles in diagnosis and management; 89% of the Lyme-specific opportunities were available free of charge.
Of the remainder of the opportunities identified (n=33), two focused on babesiosis; 10 discussed bacterial infections other than Lyme disease (Table 1); four covered arboviral diseases; and one discussed tick paralysis. Sixteen opportunities covered general topics on TBDs or larger health topics with TBDs incorporated into the agenda (ie, board review packages). Review of course abstracts indicated that 19 opportunities discussed topics related to clinical manifestations or diagnostics; 13 discussed antibiotics; eight discussed interprofessional roles in diagnosis and management; and six discussed the epidemiology of their covered diseases. Thirty percent of the non-Lyme CME opportunities were available at no cost.
We performed a scoping search for CME opportunities focused on TBDs across seven CME online databases. As expected, a large proportion of the opportunities cataloged covered topics about or related to Lyme disease. However, we found that there were surprisingly fewer CME opportunities for other TBDs of growing concern in the United States, as well as variability in the availability of these opportunities across specialty board and association websites.
Limited CME opportunities were provided for non-Lyme TBDs of growing concern. Our results only identified three opportunities explicitly targeting anaplasmosis/ehrlichiosis, two opportunities targeting babesiosis, and only one opportunity on non-RMSF rickettsioses. Additionally, three of the four identified opportunities addressing arboviruses either focused broadly on arboviral encephalitis or on tick-borne encephalitis virus specific to Europe and Asia.11 These findings suggest limited availability of continuing education for multiple life-threatening TBDs, many of which have seen an increase in prevalence within tick populations and human cases in the United States.1,12–15
We also noted surprising gaps in coverage of TBD material availability within specific medical specialty databases. The American College of Emergency Physicians database included only one opportunity related to ticks and TBDs as part of a larger general topics opportunity. Emergency and urgent-care physicians frequently encounter patients presenting with sudden symptoms or tick bites and therefore play a critical role in the diagnosis and treatment of TBDs within their scope of practice.16–18 The American Academy of Pediatrics (AAP) database also lacked any specific CME opportunities on TBDs. Instead, all potential CME opportunities were derived from content within the 2021 AAP Red Book. However, content included in the Red Book is reputed as the authority for pediatric infectious disease.19 Increasing the availability of TBD-specific CME opportunities in targeted specialty areas is essential for increased content exposure and is a necessary step to address gaps in clinical knowledge for front-line medical providers.
Several of the CME opportunities had costs for access. This inhibited an in-depth evaluation of the content covered in each opportunity beyond what was contained in the course abstract. This limitation prevented us from accounting for courses that may have mentioned common coinfections or grouped closely-related TBDs; thus, we may underreport the extent to which the identified CME opportunities address the broad scope of TBDs in the United States. We only evaluated online materials from selected medical boards and association databases; CME credits can also be obtained through attendance at in-person conferences or seminars or through other online databases that were not included in this review. Lastly, we did not investigate CME opportunities specifically targeting nonphysician care providers, including nurse practitioners and physician assistants. Evaluation of live CME opportunities provided through conferences, offered through journals, and those available in nonphysician provider databases can provide a complement to the current assessment.
Considering increasing rates of TBDs in the United States, we investigated the scope of information available to front-line care physicians on these infections. While opportunities were offered through several mediums, the overall coverage for TBDs focused primarily on Lyme disease. Increased access to timely, relevant, and enduring CME materials covering the broad scope of TBDs in the United States is needed to ensure our clinical workforce is adequately prepared to address this growing public health threat.
Acknowledgments
The authors thank Dr Laura Harrington for support provided to personnel involved in this project.
Funding: This publication was supported by cooperative agreement 1U01CK000509 between Cornell University and the Centers for Disease Control and Prevention (CDC). Contents are solely the responsibility of the authors and do not necessarily represent the official views of the CDC or the Department of Health and Human Services.
References
- Rosenberg R, Lindsey NP, Fischer M, et al. Vital Signs: trends in reported vectorborne disease cases - United States and territories, 2004-2016. MMWR Morb Mortal Wkly Rep. 2018;67(17):496-501. doi:10.15585/mmwr.mm6717e1
- Nesgos AT, Harrington LC, Mader EM. Experience and knowledge of Lyme disease: A scoping review of patient-provider communication. Ticks Tick Borne Dis. 2021;12(4):101714. doi:10.1016/j.ttbdis.2021.101714
- Fix AD, Peña CA, Strickland GT. Racial differences in reported Lyme disease incidence. Am J Epidemiol. 2000;152(8):756-759. doi:10.1093/aje/152.8.756
- Carson DA, Kopsco H, Gronemeyer P, et al. Knowledge, attitudes, and practices of Illinois medical professionals related to ticks and tick-borne disease. One Health. 2022;15:100424. doi:10.1016/j.onehlt.2022.100424
- Dixon DM, Branda JA, Clark SH, et al. Ehrlichiosis and anaplasmosis subcommittee report to the Tick-borne Disease Working Group. Ticks Tick Borne Dis. 2021;12(6):101823. doi:10.1016/j.ttbdis.2021.101823
- Mattoon S, Baumhart C, Barsallo Cochez AC, et al. Primary care clinical provider knowledge and experiences in the diagnosis and treatment of tick-borne illness: a qualitative assessment from a Lyme disease endemic community. BMC Infect Dis. 2021;21(1):894. doi:10.1186/s12879-021-06622-6
- Mosites E, Carpenter LR, McElroy K, et al. Knowledge, attitudes, and practices regarding Rocky Mountain spotted fever among healthcare providers, Tennessee, 2009. Am J Trop Med Hyg. 2013;88(1):162-166. doi:10.4269/ajtmh.2012.12-0126
- Accreditation Council for Continuing Medical Education. CME content: definitions and examples. ACCME Policies. Published 2022. Accessed May 4, 2022. https://www.accme.org/accreditation-rules/policies/cme-content-definition-and-examples
- Pace EJ, O’Reilly M. Tickborne diseases: diagnosis and management. Am Fam Physician. 2020;101(9):530-540.
- Kapoor AK, Zash R. Powassan Virus.StatPearls Publishing; 2022. Accessed February 1, 2023. https://www.ncbi.nlm.nih.gov/books/NBK570599/
- Centers for Disease Control and Prevention. Tick-borne encephalitis (TBE). Published 2022. Accessed July 7, 2022. https://www.cdc.gov/tick-borne-encephalitis/index.html
- Rodino KG, Theel ES, Pritt BS. Tick-Borne Diseases in the United States. Clin Chem. 2020;66(4):537-548. doi:10.1093/clinchem/hvaa040
- Centers for Disease Control and Prevention. Powassan virus: statistics and maps. Published 2021. Accessed May 4, 2022. https://www.cdc.gov/powassan/statistics.html
- Dupuis AP II, Prusinski MA, O’Connor C, et al. Heartland virus transmission, Suffolk County, New York, USA. Emerg Infect Dis. 2021;27(12):3128-3132. doi:10.3201/eid2712.211426
- Bamunuarachchi G, Harastani H, Rothlauf PW, et al. Detection of Bourbon virus-specific serum neutralizing antibodies in human serum in Missouri, USA. MSphere. 2022;7(3):e0016422. doi:10.1128/msphere.00164-22
- Varshavsky T, Cuthbert D, Riggs R. Babesiosis in the emergency department: a case report. J Emerg Med. 2021;61(1):e7-e10. doi:10.1016/j.jemermed.2021.01.040
- Marx GE, Spillane M, Beck A, Stein Z, Powell AK, Hinckley AF. Emergency department visits for tick bites - United States, January 2017 - December 2019. MMWR Morb Mortal Wkly Rep. 2021;70(17):612-616. doi:10.15585/mmwr.mm7017a2
- Applegren ND, Kraus CK. Lyme Disease: emergency department considerations. J Emerg Med. 2017;52(6):815-824. doi:10.1016/j.jemermed.2017.01.022
- Committee on Infectious Diseases, American Academy of Pediatrics. Red Book: 2021 - 2024 Report of the Committee on Infectious Diseases.32nd ed. American Academy of Pediatrics; 2021.




There are no comments for this article.