Inquiring about and assessing the social determinants of health (SDH) that affect patients is widely recommended in primary care encounters.1 To meet the needs of primary care professionals, several sets of questions to screen patients’ social circumstances have been developed.2 These sets are mainly informed by literature reviews and physicians’ practice-based opinions2 and therefore may prioritize physicians over other professionals and stakeholders. In Japan, a tentative SDH question set has been published.3 However, this set was not developed in a scientific manner. In our project, we aimed to reach a consensus among diverse experts including patients, non-health care stakeholders, and nonphysician medical professionals, to develop a set of items to address patients’ SDH in the Japanese primary care setting.
RESEARCH BRIEF
Assessing Social Circumstances in Primary Care: Expert Consensus via Delphi Technique
Junki Mizumoto, MD | Toshichika Mitsuyama, MD, PhD | Satoshi Kondo, MD | Masashi Izumiya, MD, PhD | Shoko Horita, MD, PhD | Masato Eto , MD, PhD
PRiMER. 2023;7:3.
Published: 1/17/2023 | DOI: 10.22454/PRiMER.2023.765336
Background and Objective: In the Japanese primary care setting, a set of questions to screen patients’ social circumstances has never been developed in a scientific manner. This project aimed to reach a consensus among diverse experts to develop a set of such questions, to meet the need for assessing patients’ health-related social circumstances.
Methods: We used a Delphi technique to generate expert consensus. The expert panel was composed of various clinical professionals, medical trainees, researchers, support members for marginalized people, and patients. We conducted multiple rounds of communication online. In round 1, the participants provided their opinions about what health care professionals should ask to assess patients' social circumstances in primary care settings. These data were analyzed into several themes. In round 2, all themes were confirmed by consensus.
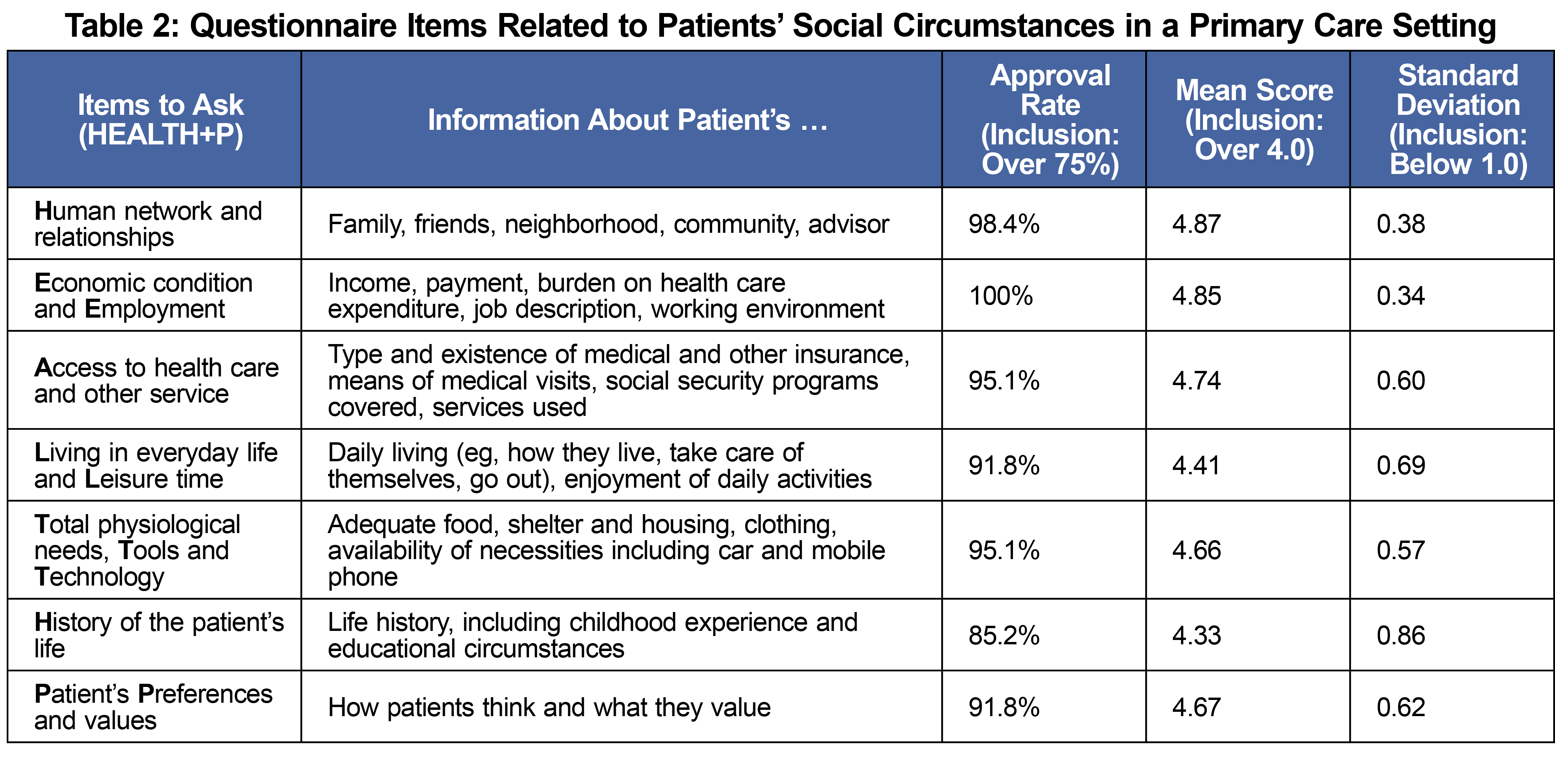
Results: Sixty-one people participated in the panel. All participants completed the rounds. Six themes were generated and confirmed: economic condition and employment, access to health care and other services, living in everyday life and leisure time, total physiological needs, tools and technology, and history of the patient's life. In addition, the panelists emphasized the importance of respecting the patient's preferences and values.
Conclusion: A questionnaire, abbreviated by the acronym of HEALTH+P, was developed. Further research about its clinical feasibility and impact on patient outcomes is warranted.
We used a Delphi technique4 to reach a consensus on inquiries about patients’ social circumstances. This study followed the Guidance on Conducting and Reporting Delphi Studies (CREDES.)5 We conducted this research simultaneously with a previously reported study, which aimed to develop observable practice activities related to SDH in primary care settings.6 The previous study described the entire process of patient care. In our study, we aimed to identify specific items to be used in medical interviews. The expert panel included various clinical professionals, medical trainees, researchers, support members for socially marginalized people, and patients. All participants provided written consent for voluntary participation.
In round 1, we asked participants what health care professionals should ask patients or other related persons to assess patients’ social circumstances in primary care settings. They recorded their opinions on an open-ended questionnaire. The first, second, and third authors analyzed the collected comments using content analysis.7 Coding data were collapsed and then modified through discussion with the other researchers to produce SDH items. In subsequent rounds, we asked participants to evaluate each item on a 5-point Likert scale (1: absolutely unimportant to 5: absolutely important) and to add free-text comments if necessary. We analyzed and selected responses using the following predefined standard: a mean score of ≥4, a standard deviation of <1, and scores of 4 or 5 from ≥75% of the panelists.
Participants were given 14 days to complete each questionnaire. Upon starting the subsequent round, participants received a summary of anonymous results from the previous round. In all rounds, questionnaires were provided via the web-based survey system SurveyMonkey (Survey Monkey, Inc, San Mateo, CA). The research ethics committee of the University of Tokyo Graduate School of Medicine and Faculty of Medicine (No. 2020250NI) provided ethical approval for this study.
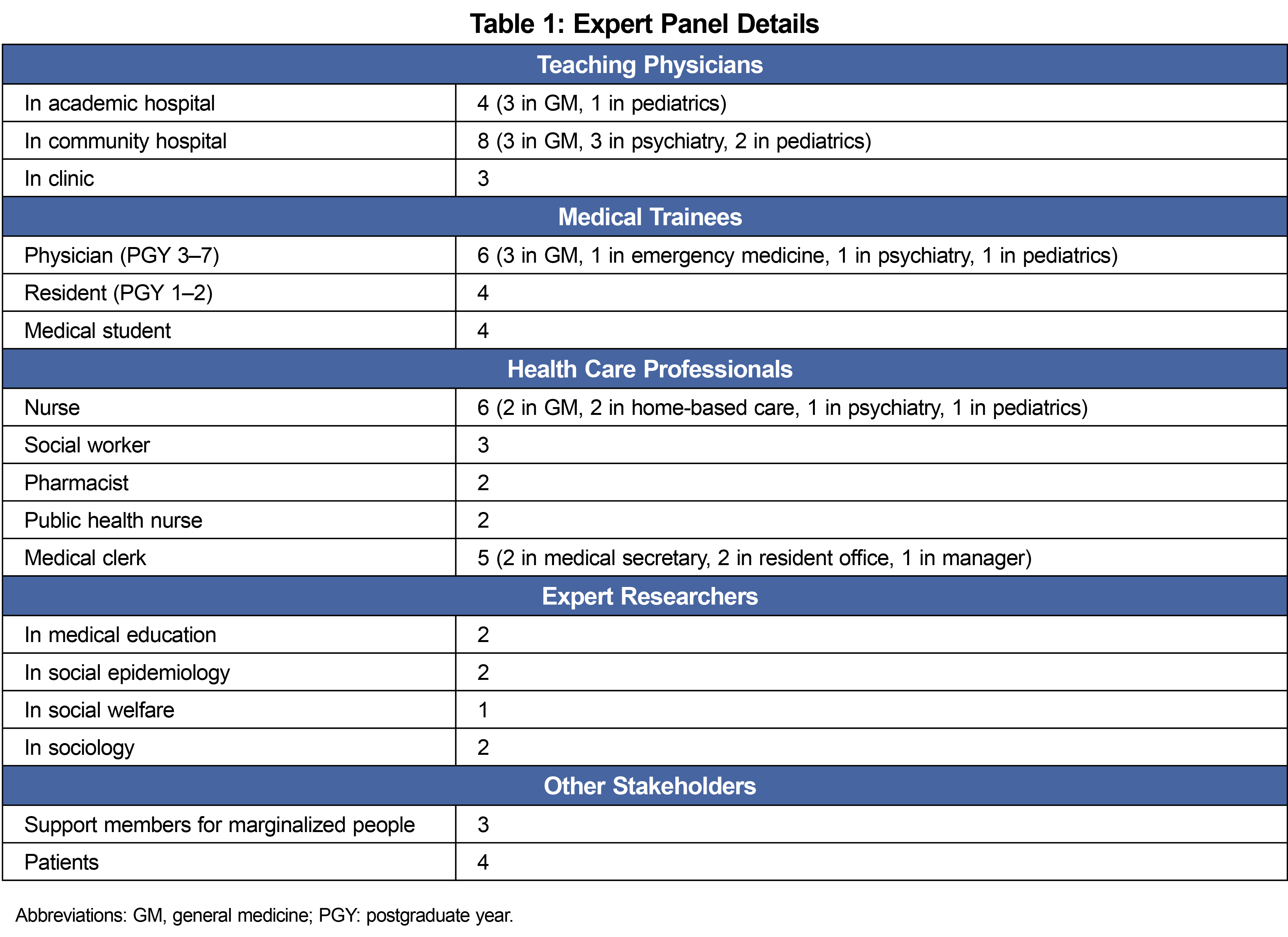
We recruited 63 people for the panel, and 61 people participated. The age range was 19–74 years (median: 42 years). Women accounted for 47.5% of the participants. Table 1 provides demographic details of the panel.
Round 1 identified 222 potentially important SDH-related factors to inquire about. Seven themes emerged from the content analysis: (1) human networks and relationships (ie, people one lives with or obtains help from); (2) economic conditions and employment (eg, income and expenditure, work); (3) access to health care and other services (eg, insurance, barriers to medical care, services used); (4) living in everyday life and leisure time (ie, basic and advanced activities, enjoyment); (5) total physiological needs, tools and technology (eg, basic life security, cars or other transportation, mobile phones); (6) history of the patient’s life (eg, childhood experiences, education); and (7) although not specifically about SDH—patient’s preferences and values. In round 2 we confirmed that all items met the positive consensus standard (Table 2), although some minor modifications were suggested. We revised the list according to these suggestions. Instead of performing round 3, we distributed the revised list to the panelists. All panelists approved the final version.
In this study, we developed an SDH assessment set via a scientific consensus-making process involving a wide range of stakeholders. To our knowledge, this is the first study to generate such a set in such a way, and we believe it will help in delivering patient-centered, quality health care. This SDH set can be abbreviated using the acronym HEALTH: Human networks and relationships; Economic conditions and Employment; Access to health care and other services; Living in everyday life and Leisure time; Total physiological needs, Tools and Technology; and History of the patient’s life.
In addition, assessing Patient’s Preferences and values (+P) should be emphasized. Although this item is not specifically about social circumstances, many participants mentioned its importance, particularly in delivering contextualized care. They believed that focusing only on patients’ social challenges sometimes meant that patients’ thoughts, beliefs, and desires were ignored. Patients’ preferences and values should thus be emphasized to avoid proposing solutions that are cheap and easy but inflexible.
Using an SDH question set may help physicians to incorporate the exploration of social factors into daily practice and facilitate dialogue with patients.8 Compared with previous relevant reports, the theme of tools and technology seems unique to this study. This theme emerged mainly from support members for socially marginalized people. Having a mobile phone is essential in modern life, and is particularly important for socially marginalized people, including people experiencing homelessness.9,10 Alcohol and tobacco use did not emerge as a separate theme in the present data, probably because this information is routinely collected in Japanese primary care settings.
This research has limitations. First, all authors and participants live in Japan. The nature of appropriate inquiries about SDH depends on the clinical situation to some extent. Cultural and structural differences should be considered in any attempts to apply these findings to other countries. For example, our list does not address racial or ethnic group differences. Second, every patient has unique social circumstances that cannot be fully encompassed by this question set. We took into account individualized approaches and care.
In conclusion, we used a consensus method to develop a set of items to inquire about and assess patients’ social circumstances in the Japanese primary care setting. The diversity of the expert panel may increase the potential clinical effectiveness of these findings. However, further research is needed on the clinical feasibility of the items and any related improvements in patient outcomes.
Acknowledgments
The authors thank Diane Williams, PhD, for editing a draft of this manuscript.
Author Contributions: J.M. developed an initial list, recruited and contacted the panelists, summarized quantitative data, coded qualitative data and wrote the manuscript. T.M. supervised the rounds, coded the data and revised the manuscript. S.K. revised the initial list, coded the data and revised the manuscript. M.I., S.H., and M.E. revised the initial list, data coding, and the manuscript. All authors have given final approval to the paper.
References
- Daniel H, Bornstein SS, Kane GC; Health and Public Policy Committee of the American College of Physicians. Addressing Social Determinants to Improve Patient Care and Promote Health Equity: An American College of Physicians Position Paper. Ann Intern Med. 2018;168(8):577-578. doi:10.7326/M17-2441
- LaForge K, Gold R, Cottrell E, et al. How 6 Organizations Developed Tools and Processes for Social Determinants of Health Screening in Primary Care: an Overview. J Ambul Care Manage. 2018;41(1):2-14. doi:10.1097/JAC.0000000000000221
- Mizumoto J, Terui T, Komatsu M, et al. Social vital signs for improving awareness about social determinants of health. J Gen Fam Med. 2019;20(4):164-165. doi:10.1002/jgf2.251
- Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32(4):1008-1015.
- Jünger S, Payne SA, Brine J, Radbruch L, Brearley SG. Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: recommendations based on a methodological systematic review. Palliat Med. 2017;31(8):684-706. doi:10.1177/0269216317690685
- Mizumoto J, Mitsuyama T, Kondo S, Izumiya M, Horita S, Eto M. Defining the observable processes of patient care related to social determinants of health. Med Educ. 2023;Jan57(1):57-65. doi:10.1111/medu.14915
- Burnard P. A method of analysing interview transcripts in qualitative research. Nurse Educ Today. 1991;11(6):461-466. doi:10.1016/0260-6917(91)90009-Y
- Mizumoto J, Son D, Izumiya M, Horita S, Eto M. Experience of residents learning about social determinants of health and an assessment tool: mixed-methods research. J Gen Fam Med. 2022;23(5):319-326; Epub Ahead of Print. doi:10.1002/jgf2.559
- Raven MC, Kaplan LM, Rosenberg M, Tieu L, Guzman D, Kushel M. Mobile phone, computer, and internet use among older homeless adults: results from the HOPE HOME cohort study. JMIR Mhealth Uhealth. 2018;6(12):e10049. doi:10.2196/10049
- Thurman W, Semwal M, Moczygemba LR, Hilbelink M. Smartphone technology to empower people experiencing homelessness: secondary analysis. J Med Internet Res. 2021;23(9):e27787. doi:10.2196/27787
Lead Author
Junki Mizumoto, MD
Affiliations: Department of Medical Education Studies, International Research Center for Medical Education, Graduate School of Medicine, the University of Tokyo, Tokyo, Japan
Co-Authors
Toshichika Mitsuyama, MD, PhD - Department of Medical Education Studies, International Research Center for Medical Education, Graduate School of Medicine, the University of Tokyo, Tokyo, Japan
Satoshi Kondo, MD - Department of Medical Education Studies, International Research Center for Medical Education, Graduate School of Medicine, the University of Tokyo, Tokyo, Japan
Masashi Izumiya, MD, PhD - Department of Medical Education Studies, International Research Center for Medical Education, Graduate School of Medicine, the University of Tokyo, Tokyo, Japan
Shoko Horita, MD, PhD - Department of Medical Education Studies, International Research Center for Medical Education, Graduate School of Medicine, the University of Tokyo, Tokyo, Japan
Masato Eto , MD, PhD - Department of Medical Education Studies, International Research Center for Medical Education, Graduate School of Medicine, the University of Tokyo, Tokyo, Japan
Corresponding Author
Junki Mizumoto, MD
Correspondence: Department of Medical Education Studies, International Research Center for Medical Education, Graduate School of Medicine, The University of Tokyo, 7-3-1 Hongou, Bunkyo-ku, Tokyo, 113-0033 Japan. +81(03)-3812-2111.
Email: jnk_mizu@yahoo.co.jp
Fetching other articles... 
Loading the comment form... 
Submitting your comment... 


There are no comments for this article.