Introduction: In August 2022, mpox (formerly “monkeypox”) was declared a public health emergency in the United States, yet there has been little published on medical providers’ knowledge or perceptions of the disease. With one of the highest incidence rates in the United States being in South Florida, our Miami-based medical school aimed to assess students' perceived levels of knowledge and attitudes regarding mpox.
Methods: An optional, anonymous survey consisting of multiple choice and Likert-type questions was emailed to all medical students. The first survey was sent out September 1, 2022, after which students received reminders on October 3, 8, and 31, 2022. We analyzed respondents’ perceived knowledge and risk of contracting mpox by comparing responses between heterosexual and LGBTQ+ groups and preclinical and clinical groups. We used Mann-Whitney U or Kruskal Wallis tests for inferential statistical analysis.
Results: Of 480 medical students, 168 (35.0%) responded to the survey. Most respondents (88.1%) were not concerned about mpox; 95.2% perceived their personal risk to be moderate or low. LGBTQ+ students were significantly more likely than others to report feeling at risk from mpox. The majority (72.0%) of respondents reported poor perceived knowledge of mpox. There was no significant difference between preclinical and clinical students' reported level of perceived knowledge (P=.0621); 76.2% of respondents were not confident in their ability to recognize mpox symptoms. LGBTQ+ students were significantly more confident in identifying symptoms than others (P=.0201).
Conclusion: Medical students feel they lack critical knowledge of mpox and report being unprepared to recognize disease symptoms. The higher level of perceived risk and knowledge among LGBTQ+ students may stem from biases perpetuated by public messaging regarding mpox. These findings highlight the need for integrating education on emerging epidemics into undergraduate medical education to enable students to safely provide high-quality patient care.
Mpox, previously known as “monkeypox,” causes several weeks of a self-limiting viral disease with flu-like symptoms, swollen lymph nodes and rashes, but severe and fatal cases have also been reported. The mpox virus is transmitted from person to person via close contact with lesions, body fluids, respiratory droplets and contaminated materials.1 Transmission of the virus through respiratory droplets requires prolonged face-to-face contact, which puts health workers, household members, and other close contacts at greater risk.2 Biases and stigma within the general population and medical community regarding mpox have inaccurately presented men who have sex with men (MSM) as the primary population to contract and spread the virus.3
Since 1970, human cases of mpox have been reported in more than 10 African countries. In 2003, mpox was identified as a global public health concern, when its first outbreak outside of Africa occurred in the United States.2
In May 2022, cases of mpox were identified in several nonendemic countries, including the United States, where the highest incidence occurred in California, New York, Texas, and Florida.4 Research from August 2022 found that, although most of the population was aware that the mpox virus existed, only one-third of Americans considered themselves at least somewhat knowledgeable about the virus.5
Similarly, in 2022, after the first case of mpox was documented in Saudi Arabia, a cross-sectional study assessing medical students’ knowledge of and attitudes toward mpox was conducted at a medical school in the country. In line with the findings of the study in Saudi Arabia, two other studies in Syria10 and Jordan11 also found poor knowledge of mpox among undergraduate medical students. There are, however, no studies on this subject matter reported in the United States. Therefore, given this dearth of research in the United States, our study aimed to assess both clinical and preclinical medical students’ perceived knowledge of, and attitudes related to mpox at our medical school in South Florida.
All undergraduate medical students at a medical school in South Florida were invited to complete an anonymous, optional, online survey consisting of Likert-type and multiple-choice questions. The first survey was sent out September 15, 2022, via class email list servs, after which students received three reminders on October 3, 8, and 31, 2022. We examined univariate and bivariate frequency distribution for all research questions after exploratory data analysis. The comparison groups were heterosexual vs LGBTQ+ and preclinical students vs clinical students, respectively.
We used the Mann-Whitney U test and Kruskal Wallis tests to analyze the data, as appropriate. We used nonparametric tests for ordinal dependent variables which did not meet the assumptions of normality. We set the level of significance at 0.05 for all analyses. We conducted all statistical analyses using R version 4.2.1. Institutional Review Board exemption was obtained.
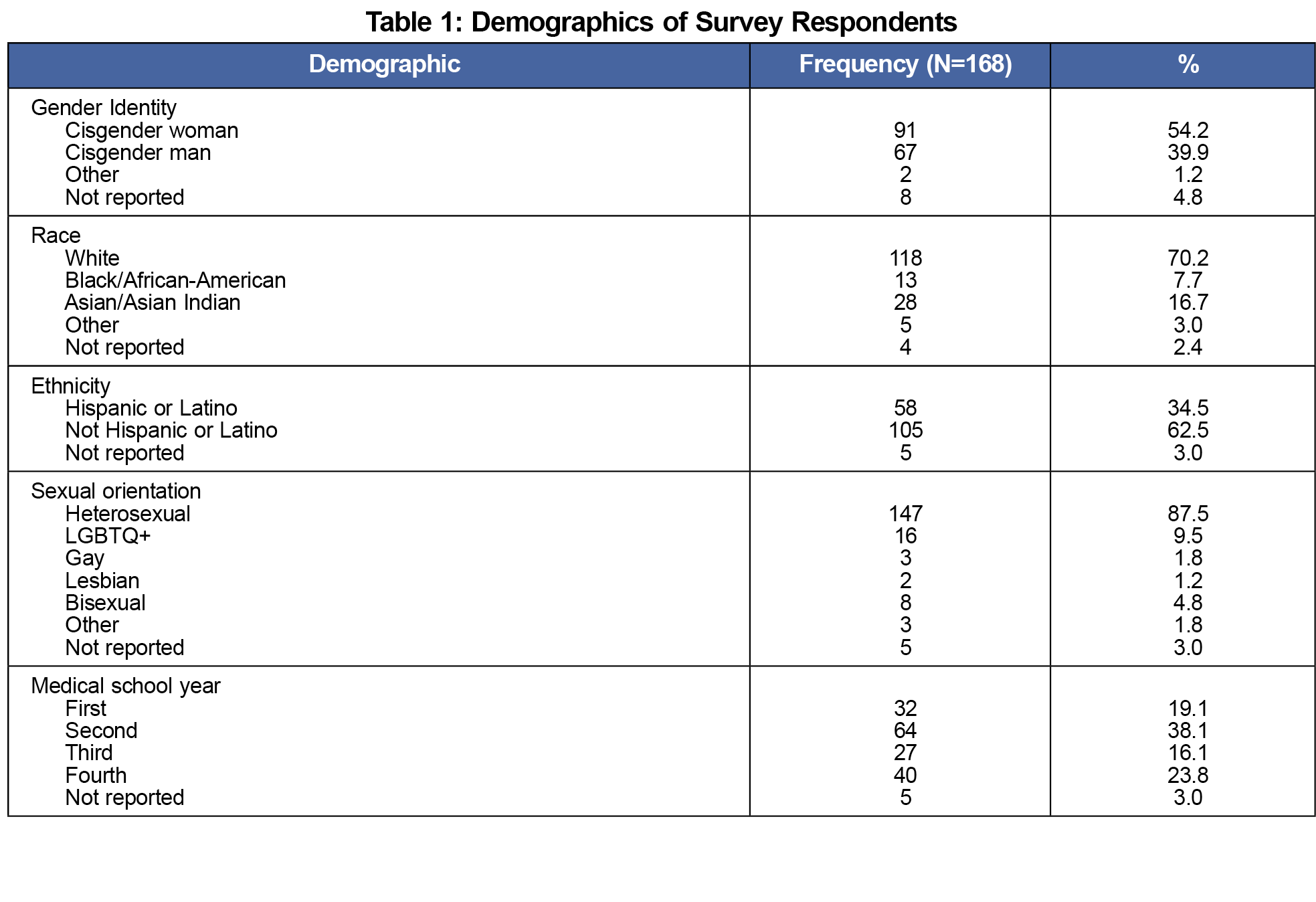
A total of 168 out of a possible 480 (35.0%) students completed the survey, of which 70.2% identified as White, 7.7% as Black, 16.7% as Asian, and 3.0% as other. Additionally, 34.5% of respondents identified as Hispanic. Regarding gender identity, 54.2% of respondents identified as cisgender women while 39.9% as cisgender men. Moreover, 9.5% of respondents identified as LGBTQ+ while 87.5% identified as heterosexual. The majority of respondents (57.2%) were in their preclinical years while 39.9% were in their clinical years (Table 1).
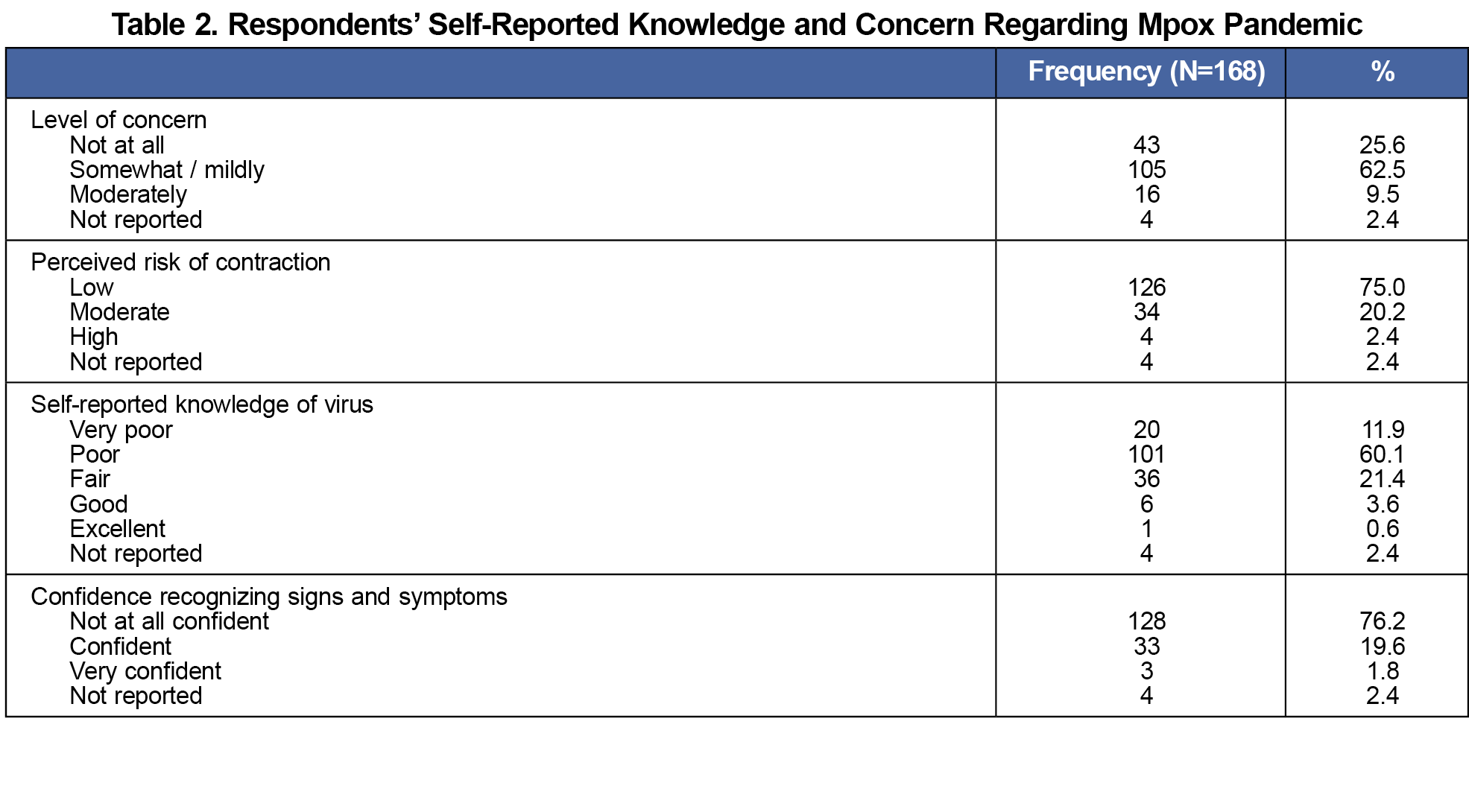
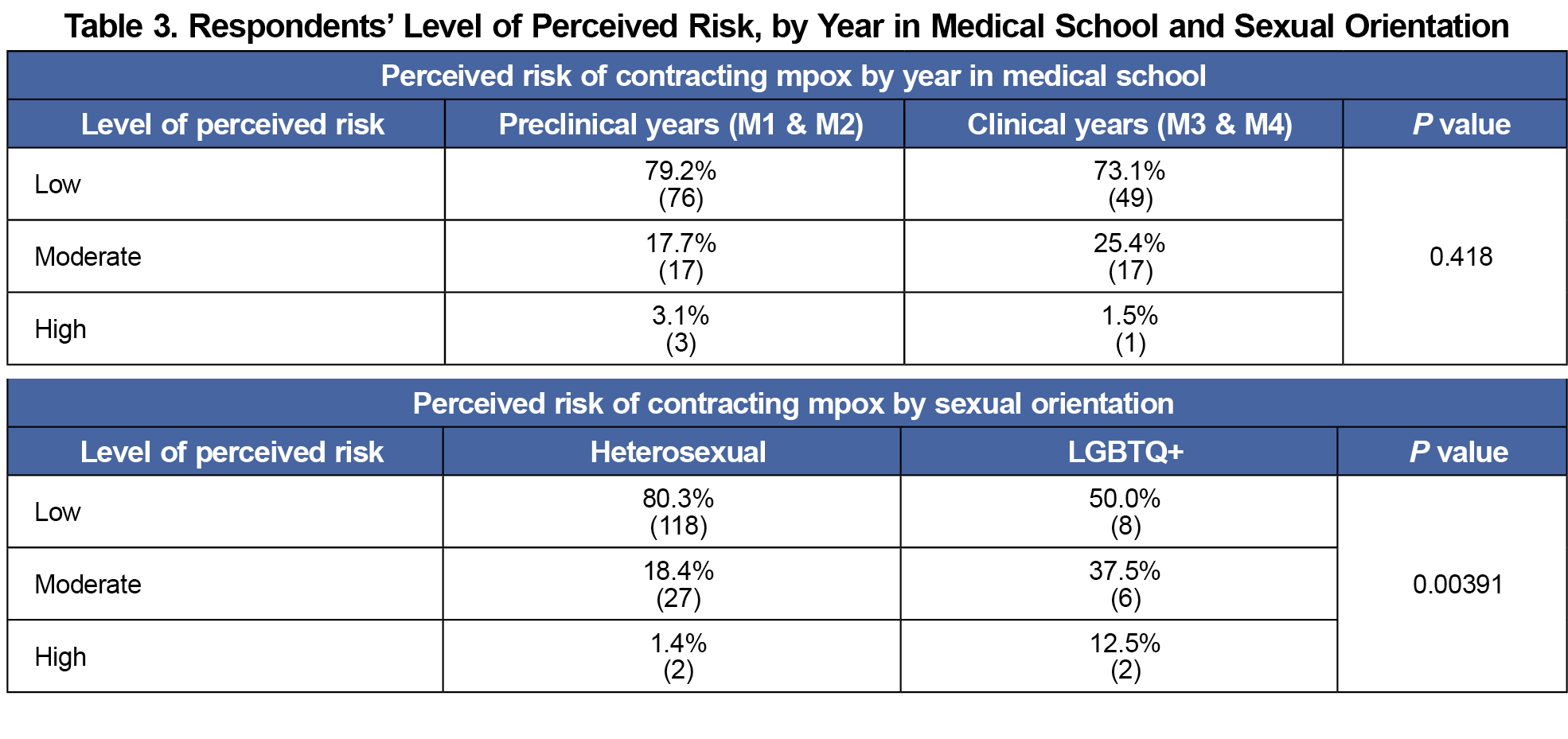
Only 9.5% of the respondents were moderately concerned about the mpox outbreak, while 88.1% were either mildly or not at all concerned. Similarly, only 2.4% of respondents felt they were at high risk of contracting the virus, 20.2% reported feeling at moderate risk, and 75.0% felt they were low risk (Table 2). There was no significant difference in the level of perceived risk between preclinical and clinical students (P=.418; Table 3). However, students identifying as LGBTQ+ were significantly more likely to report feeling at risk of mpox infection when compared to students identifying as heterosexual (P=.00391; Table 4).
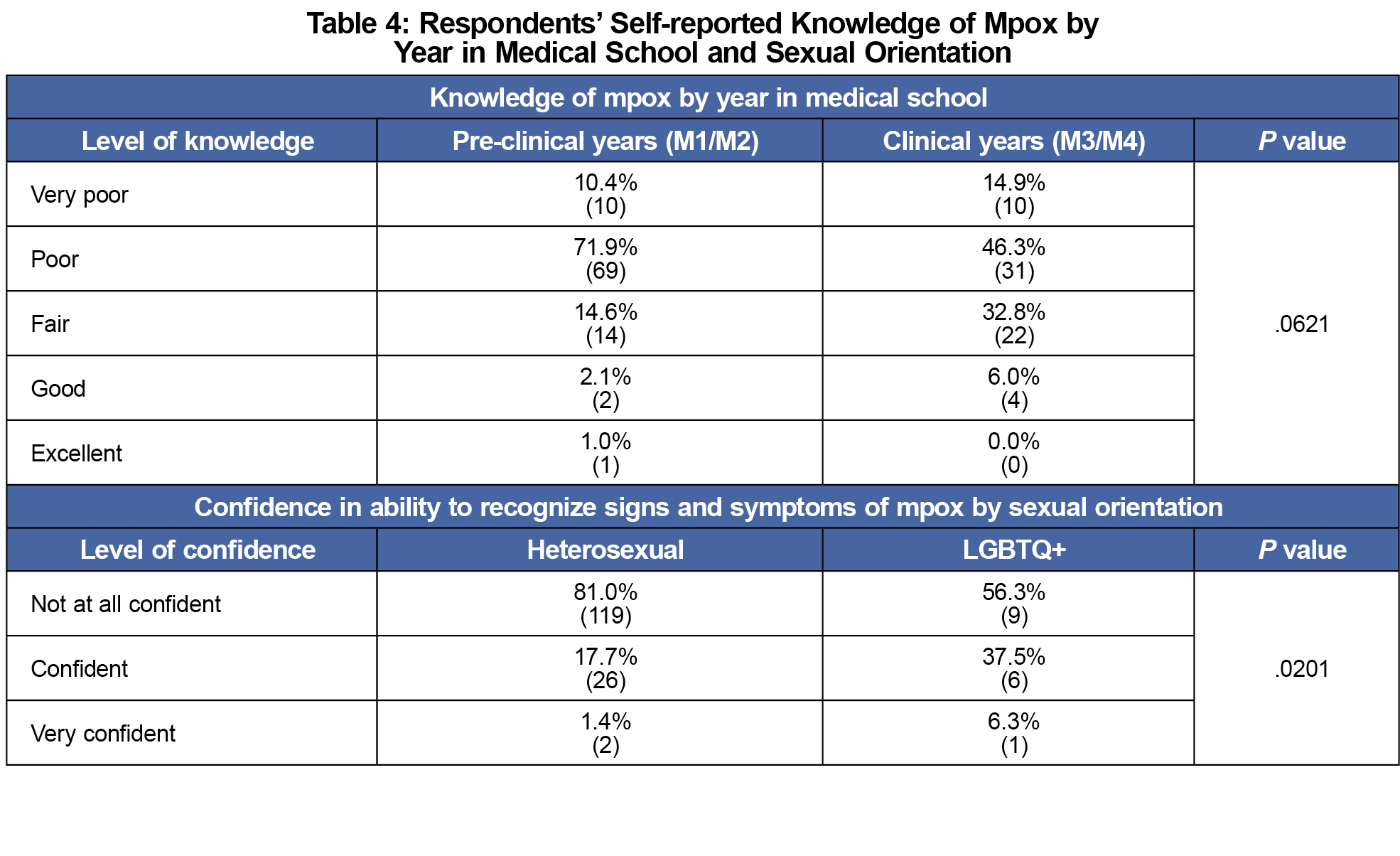
The survey showed that 72.0% of respondents rated their perceived knowledge of the mpox virus as either poor or very poor, 21.4% rated their perceived knowledge as fair, while only 4.2% rated their perceived knowledge as good or excellent. There was no significant difference in the level of perceived knowledge reported by students based on their year of training (P=.0621; Table 4). Similarly, 76.2% of respondents stated that they were not at all confident in their ability to recognize mpox symptoms (Table 2). Lastly, students identifying as LGBTQ+ were significantly more confident in their ability to recognize mpox symptoms compared to students who identify as heterosexual (P=.0201; Table 4).
Our results show that LGBTQ+ students were significantly more likely to perceive themselves to be at risk of contracting mpox when compared to their heterosexual peers. Furthermore, LGBTQ+ respondents were found to have significantly greater confidence in identifying the signs and symptoms of infection. We surmise that this difference may be attributed to the fact that public messaging regarding mpox has heavily targeted MSM, making the virus seem more relevant to this population.7
Despite a marginal P value (.06) and small sample size that may diminish the strength of our conclusions, we found no significant difference in the level of concern for, or self-reported knowledge related to mpox between clinical and preclinical students. Regardless, given that clinical students are on the frontlines, interacting with patients with undifferentiated symptoms, it is essential that they understand their vulnerability to infectious diseases and how to best prevent transmission. Moreover, there was no formal mpox education within our medical school curriculum, so it is likely that student knowledge was largely obtained through media and public messaging.
When specifically analyzing the composition of such mpox media messaging, a 2023 study found that approximately two-thirds of participants agreed that media-related content about mpox targeted and stigmatized gay, bisexual, and other MSM.8 With this finding, we theorize that consumption of targeted media content by LGBTQ+ students likely impacted their reported higher levels of both self-risk and knowledge, as they likely sought to learn more about the virus in an attempt to avoid transmission. However, messaging concerning mpox transmission that has overwhelmingly targeted the MSM population may have left medical students with little awareness of the risks and preventive measures of mpox. To ensure the safety of their clinical students, medical schools must quickly adapt curriculum to include new and emerging diseases.8
While our study assessed perceived knowledge, its results support other studies, including the one from Saudi Arabia6 that found low levels of mpox knowledge amongst medical providers.10,11 Studies in Syria, Saudi Arabia, and Jordan, along with our findings, reinforce the importance of incorporating education on emerging epidemics into undergraduate medical curricula. This is a crucial step to equip students with the necessary knowledge to ensure both patient and student safety.
One limitation of this study is its small sample size, which may have limited our ability to detect significant effects or associations. Moreover, the data were collected from medical students at a single institution, which may limit the generalizability of the findings. Further limitations include reliance on self-reported data, which is subject to response bias. While we proposed potential reasons for the higher self-risk or self-knowledge among LGBTQ students, it is important to note that our study did not establish causality on this topic, as direct measurements were not surveyed. Despite these limitations, our study begins to address the need for research on the topic.
Next steps in this project include conducting a multi-institutional study with a more diverse sample of participants. Additionally, it may be valuable to develop curricula that close gaps in knowledge regarding mpox and other emerging infectious diseases. With such curricular interventions, there is potential to enhance student understanding of mpox and ultimately improve patient management and outcomes.
Acknowledgments
* Jake Nusynowitz and Lily Jamneshan contributed equally to this manuscript and are designated as co-first authors.
References
- About Mpox. Centers for Disease Control and Prevention. Updated August 30, 2023. Accessed February 22, 2023. https://www.cdc.gov/poxvirus/monkeypox/about/index.html
- Mpox (monkeypox). World Health Organization. Updated April 18, 2023. Accessed February 22, 2023. https://www.who.int/news-room/fact-sheets/detail/monkeypox.
- Yang Z, Liu X, Zhu Z, et al. Combating stigma and health inequality of Monkeypox: experience from HIV. Infect Drug Resist. 2022;15:5941-5943. doi:10.2147/IDR.S383471
- 2022 U.S. Map & Case count. Centers for Disease Control and Prevention. Accessed February 22, 2023. https://www.cdc.gov/poxvirus/monkeypox/response/2022/us-map.html.
- Public knowledge of monkeypox increases but over 1 in 4 unlikely to get vaccinated if exposed. Annenberg Public Policy Center. https://www.asc.upenn.edu/news-events/news/public-knowledge-monkeypox-increases-over-1-4-unlikely-get-vaccinated-if-exposed. Accessed February 22, 2023.
- Alshahrani NZ, Mitra S, Alkuwaiti AA, et al. Medical students’ perception regarding the re-emerging monkeypox virus: an institution-based cross-sectional study from Saudi Arabia. Cureus. 2022;14(8):e28060. doi:10.7759/cureus.28060
- Dsouza VS, Rajkhowa P, Mallya BR, et al. A sentiment and content analysis of tweets on monkeypox stigma among the LGBTQ+ community: A cue to risk communication plan. Dialogues Health. 2023;2:100095. doi:10.1016/j.dialog.2022.100095
- Owens C, Hubach RD. An exploratory study of the Mpox media consumption, attitudes, and preferences of sexual and gender minority people assigned male at birth in the United States. LGBT Health. 2023;10(5):401-407. doi:10.1089/lgbt.2022.0251
- Stumbar SE, Nusynowitz J, Jamneshan L, Samuels M, Garba NA. The Need for Emerging Diseases Curricula: A Case Study of Mpox. PRiMER Peer-Rev Rep Med Educ Res. 2022;6:922238. doi:10.22454/PRiMER.2022.922238
- Swed S, Alibrahim H, Bohsas H, et al. Monkeypox in Syria: highlighting an awareness issue. IJID Reg. 2023;7:271-276. doi:10.1016/j.ijregi.2023.04.008
- Sallam M, Al-Mahzoum K, Al-Tammemi AB, et al. Assessing Healthcare Workers’ knowledge and their confidence in the diagnosis and management of human Monkeypox: A cross-sectional study in a Middle Eastern country. Healthcare (Basel). 2022;10(9):1722. doi:10.3390/healthcare10091722



There are no comments for this article.