Introduction: Mitigating the stress of graduate medical education has been the focus of residency leadership in the United States. This study examined family medicine (FM) resident and program director (PD) satisfaction with current wellness curricula, including perceptions of availability of resources and emphasis on well-being.
Methods: The Council of Academic Family Medicine Educational Research Alliance administered online surveys to PDs accredited by the Accreditation Council for Graduate Medical Education, US-based FM residencies, and resident American Academy of Family Physicians members from April to May 2021. The present study included an assessment of wellness curriculum implementation using the Wellness Element Count (WEC), a satisfaction rating with wellness programming, and a single question assessing perceived changes in emphasis on wellness during COVID-19.
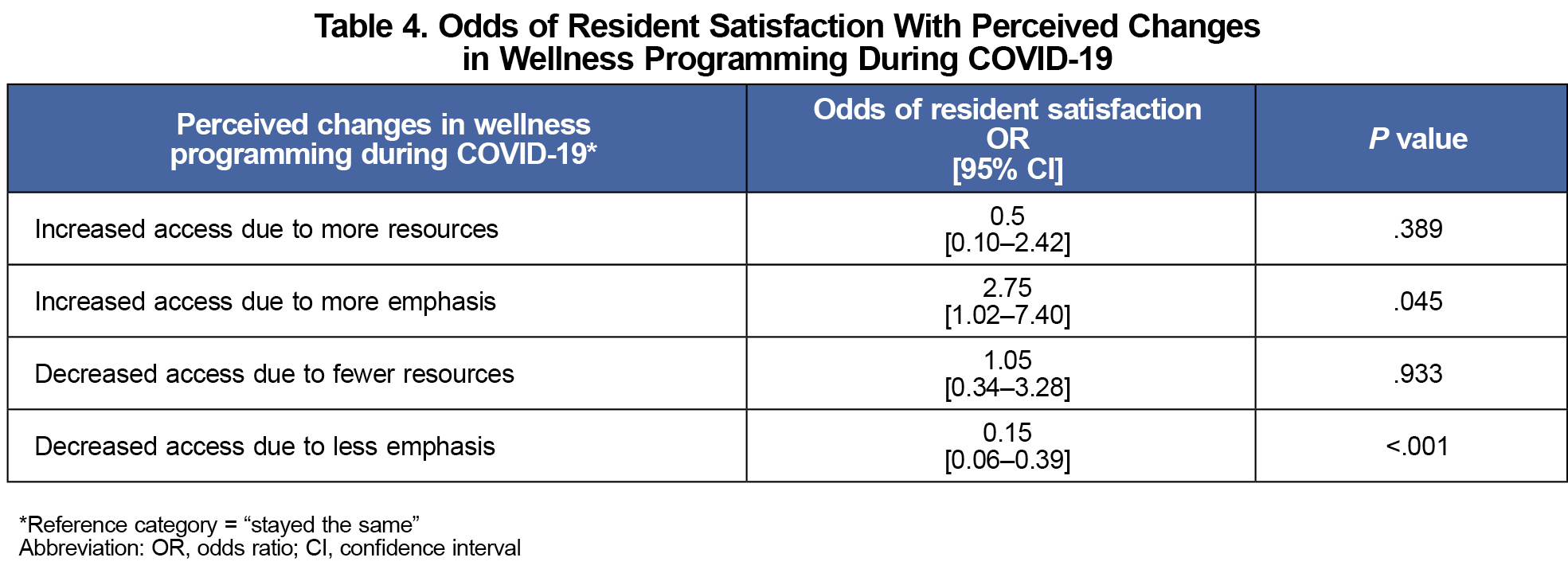
Results: A total of 242 residents (5% response rate) and 263 PDs (42% response rate) completed the survey. Residents reported lower WEC indicators compared to PDs (P<.001). Overall, 67.8% of resident respondents were satisfied with their program’s wellness efforts, compared to 89.3% of PDs (P<.001). Perceived emphasis on wellness curricula in the program was associated with greater resident satisfaction (OR=2.75, P<.05); less emphasis on wellness was associated with less resident satisfaction (OR=0.15, P<.001).
Conclusions: Residents reported overall lower perceived availability and satisfaction with program wellness efforts compared to PDs, suggesting a disparity between perspectives. Ongoing efforts should be directed at encouraging use of available wellness resources and supporting a culture of well-being.
Residency is a high-stress period requiring long hours, heavy workloads, and volumes of new information and skills to master. These stressors present an elevated risk of burnout and decreased well-being.1,2 Consistent with current Accreditation Council for Graduate Medical Education (ACGME) program requirements, family medicine (FM) leadership has encouraged wellness programming based on available evidence.3-5 However, residents face barriers accessing wellness resources, including lack of awareness, stigma around help-seeking, and competing demands for their time.6,7 Additionally, residents may have differing opinions on how best to structure wellness-related activities or what should be emphasized.4,8-10
Residents from various specialties have identified time away, positive learning environments, confidential access to mental health treatment, and protected time for wellness education as necessary to support resident well-being.11-14 Some elements (eg, time off, protected time for wellness education) must be balanced with program requirements for educational and clincial responsibilities, potentially creating misalignment between program director (PD) and resident views about how to prioritize curricula to support resident well-being.8,15
Resident input can help prioritize resources and guide implementation of wellness curricula that are designed for them. Several studies have assessed what residents think wellness programs should include and have sought their feedback on specific interventions. However, information on what residents perceive is actually available to them has been missing from much of the residency well-being research. A mismatch between what PDs and residents deem to be available to support well-being could create conflict. Our study sought to fill a critical gap by comparing FM resident and PD perspectives on accessibility of current wellness curricula and resident satisfaction with wellness programming.
Procedures
Our survey questions were distributed as part of separate online Council of Academic Family Medicine Educational Research Alliance (CERA) surveys from April 17, 2021, to May 17, 2021. CERA distributed regularly scheduled surveys to PDs of all US-based, ACGME-accredited FM residency programs, as well as a special survey of American Academy of Family Physicians (AAFP) resident members.15-17 The AAFP Institutional Review Board approved our projects in April 2021.
Measures
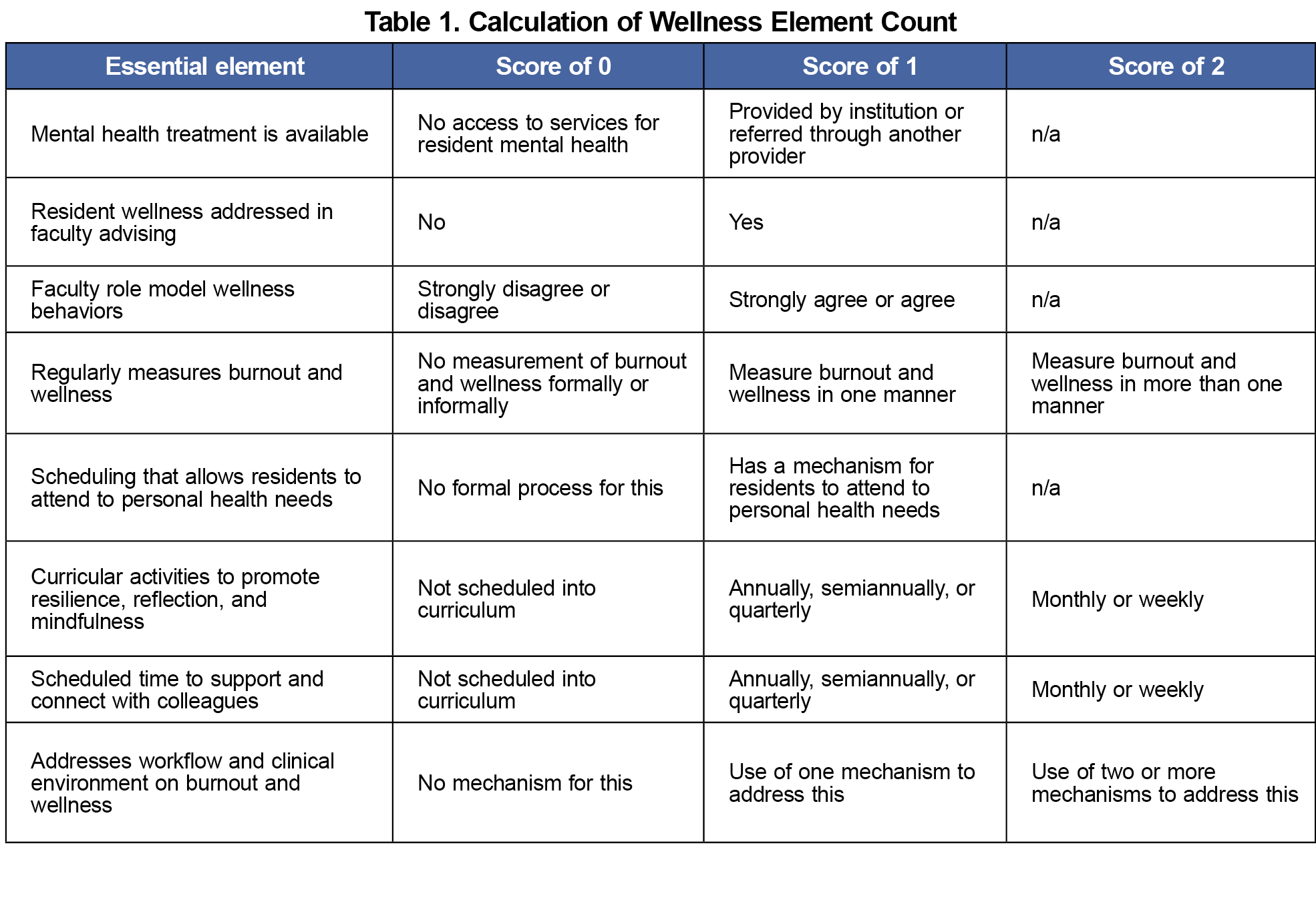
Included with a standard set of demographic questions and approximately 40 questions focused on various special topics, our portion of the surveys was comprised of 10 wellness curriculum-focused questions. Eight items were totaled for the Wellness Element Count (WEC)—a list of essential elements of a wellness curriculum that respondents rate to indicate the availability of each component in their program’s curriculum.11,15,18 Some elements were rated on a continuous frequency scale (weekly, quarterly, or yearly), whereas others were rated dichotomously (present or not); see Table 1 for scoring. Higher WEC scores indicated greater presence of essential wellness elements in a residency program. We also included one question on satisfaction with wellness programming (dichotomized in analyses into satisfied [agree and strongly agree] and unsatisfied [disagree and strongly disagree]). Because respondents completed the survey after the first year of the COVID-19 pandemic, we included a question about whether they perceived an increased or decreased emphasis on well-being or access to wellness resources in the preceding year.
Data Analysis
We assessed bivariate associations using χ2 testing for proportions. Due to the nonnormal distribution of WEC scores, we selected the mode as the measure of central tendency and two-sided Wilcoxon rank-sum testing for comparisons between residents and PDs. We used logistic regression to measure the association between residents’ satisfaction with wellness programming and programmatic changes (ie, increased or decreased resources or emphasis). We conducted analyses using SPSS (IBM) and Stata 17 (StataCorp).
Participants
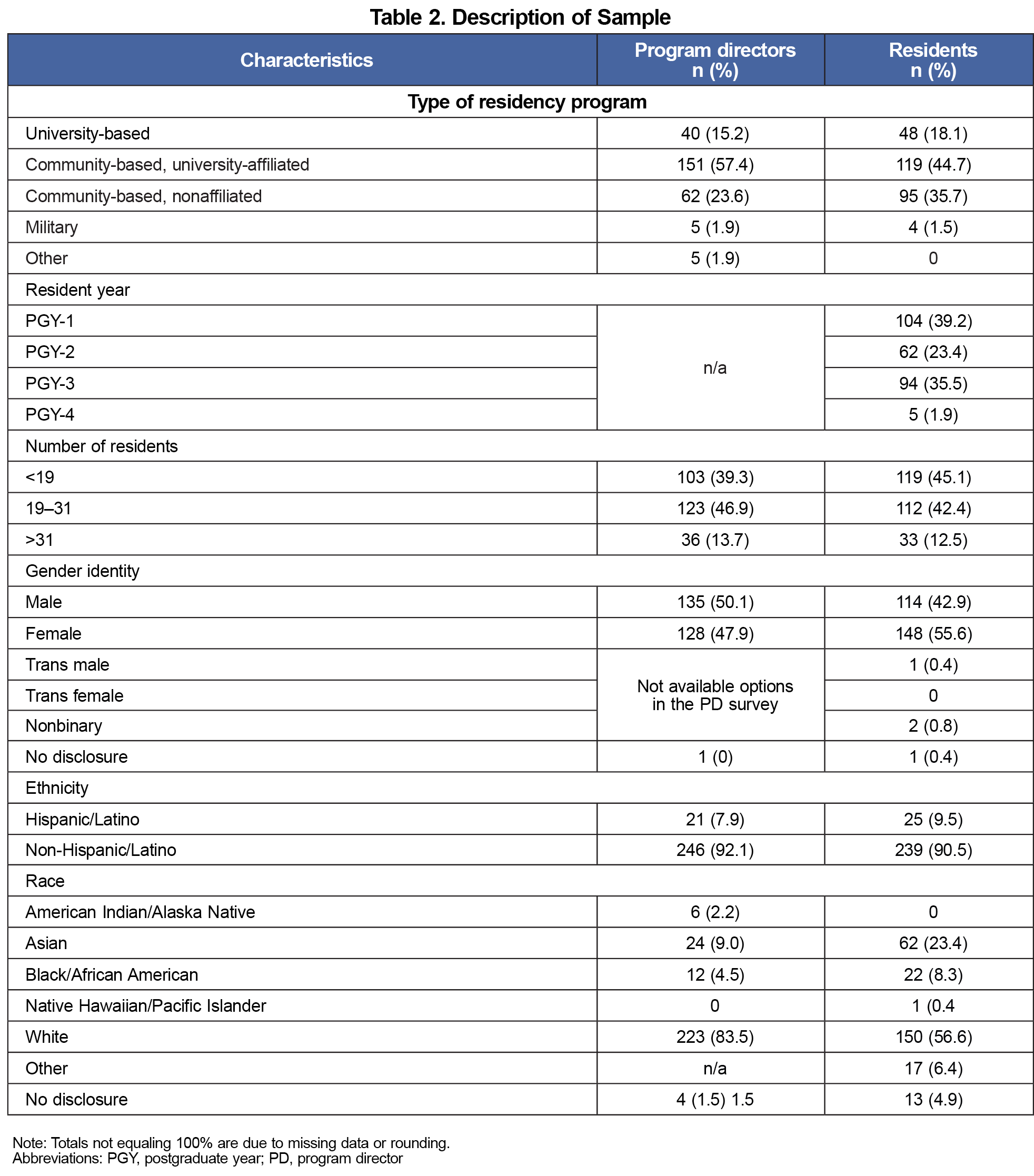
Of the 5,000 AAFP resident members who received the study invitation, 266 responded. Twenty-four residents did not complete wellness curriculum items and were excluded from analyses, leaving a final sample of 242 (4.8% response rate). Two hundred sixty-three PDs completed the PD survey (42.5% response rate). Respondents’ demographics and program information are reported in Table 2.
We analyzed the representativeness of our resident sample for gender, race, and ethnicity from AAFP and ACGME FM resident data using a one-sample χ2 test.19,20 Analyses indicated that the resident sample was representative of FM residents nationally for gender (χ2[df=1]=0.575, P=.448), race (χ2[df=1]=0.014, P=.905), and ethnicity ([df=3]=1.82, P=.611). A χ2 test comparing PD and resident populations indicated similar representation across program type (χ2[df=2]=1.51, P=.47) and size (χ2[df=2]=1.143, P=.565).
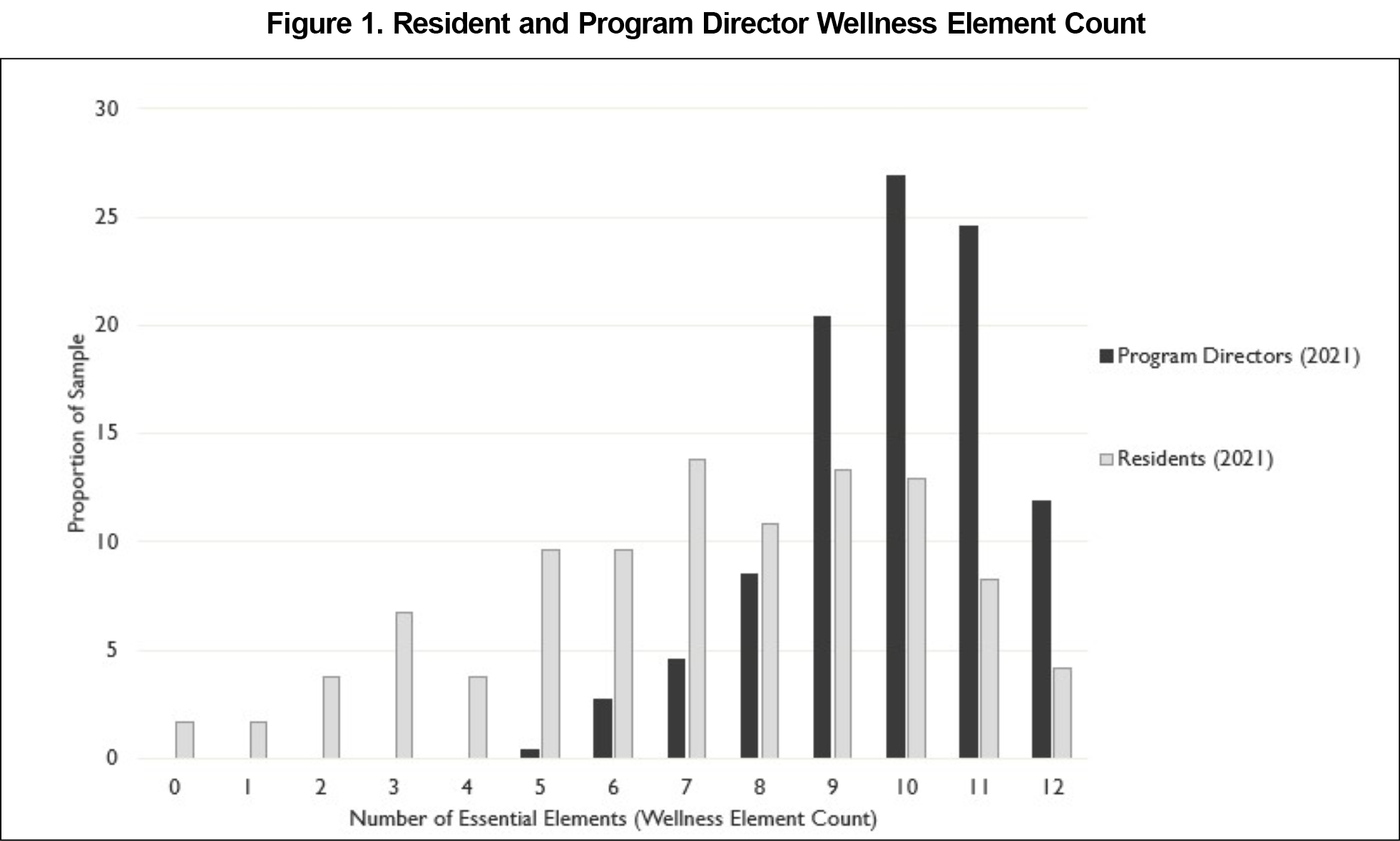
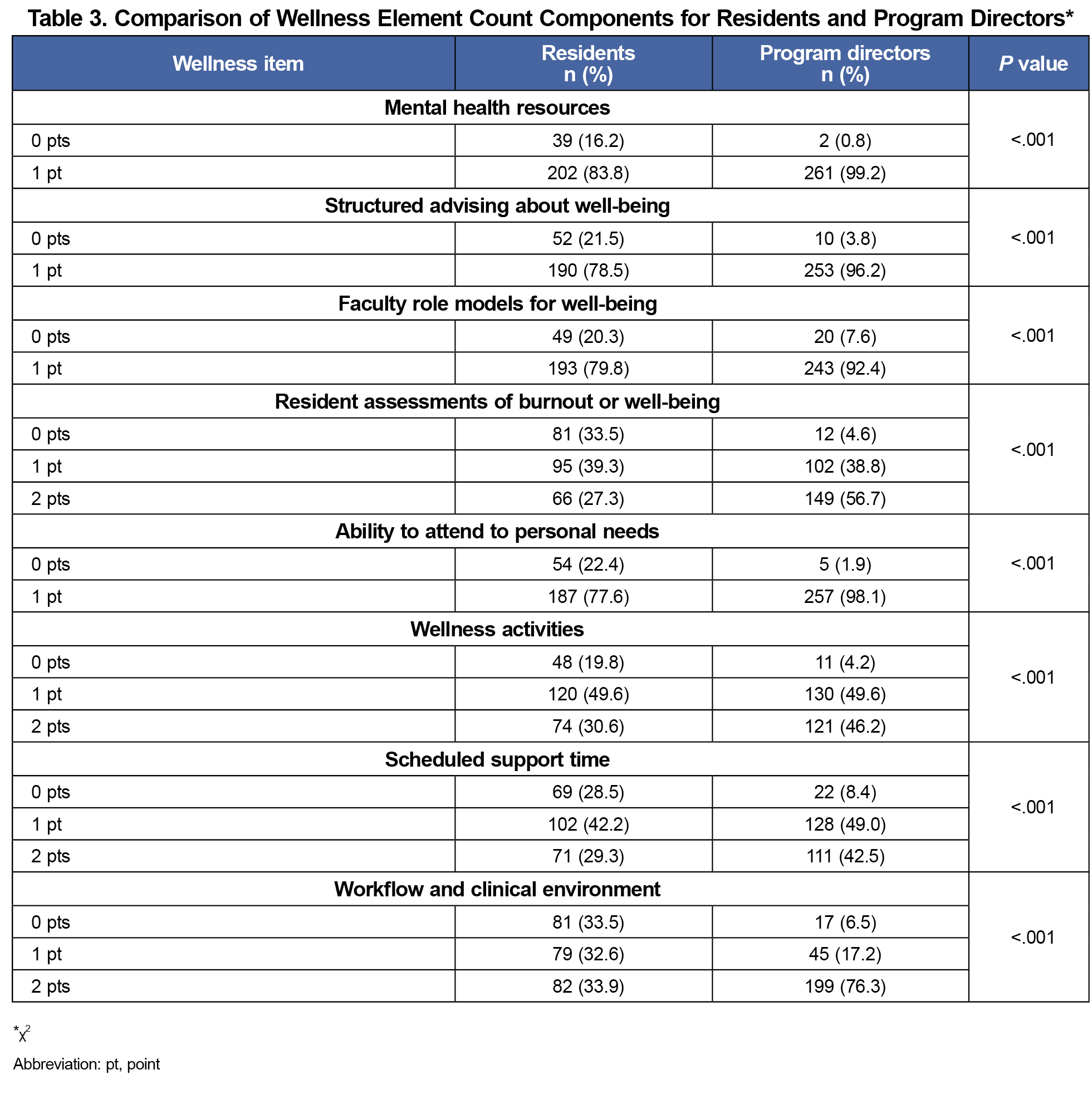
Overall, residents reported lower WEC scores than did PDs, with modes of 7 and 10, respectively (P<.001; Figure 1). Ratings by residents were significantly lower than PDs for each element of the WEC (Table 3).
Resident satisfaction with wellness programming was significantly lower than PD satisfaction. Whereas 67.8% of residents endorsed satisfaction, 89.3% of PDs were satisfied (P<.001). Fewer residents reported greater emphasis on wellness programming (20.7% vs 48.9% PDs) and access to resources (2.9% vs 5.7% PDs) during the preceding academic year. We found a positive association in resident perception of wellness program efforts with increased emphasis (OR=2.75, P<.05). Residents who perceived less emphasis on wellness in their curriculum were less likely to report satisfaction with program wellness efforts (OR=0.15; P<.001). We found no association between perceived access to resources and resident satisfaction. Table 4 presents odd ratios for resident satisfaction and perceived changes in wellness.
Previous studies have indicated misalignment between PDs and residents on what should be included in a residency wellness curriculum. Our study sought to explore PD and resident viewpoints on existing residency wellness curricula and their satisfaction with wellness programming. Approximately one-third of our sample of FM residents were not satisfied with their program’s wellness efforts and felt that less was being done about resident well-being than PDs perceived. These results are similar to studies reporting discordance between PD and resident perspectives on wellness from other specialties.21,22 When compared to PD ratings, residents reported lower presence of each essential element of a wellness curriculum, including things expressly mentioned in the ACGME common program requirements (eg, access to mental health resources, ability to attend personal appointments).3 Because programs must ensure that wellness resources are provided to be consistent with ACGME program requirements, this discrepancy indicates that barriers exist to residents having favorable impressions about implementation of support resources and curricula. Previous research has indicated that these barriers may include residency culture or communication that doesn’t clearly indicate what is available and the support for using it.6,7
Of note, the study occurred during COVID-19, when demands and resources for wellness were in flux. While resource allocation did not influence satisfaction, the degree to which programs emphasized well-being was associated with resident satisfaction. Residents reported higher satisfaction with wellness efforts if they perceived increased emphasis on wellness in their programs during this time and lower satisfaction if they perceived less emphasis on wellness. Again, this finding underscores the need for a culture that clearly supports engagement in available resources and is consistent with prior research that identifies unsupportive or mixed messaging about wellness as a barrier to residents using wellness resources.7 Emphasizing well-being may enhance resident satisfaction with program wellness efforts.23
Future studies may build on current results by asking specific questions about support for well-being and implementation of and satisfaction with wellness curriculum, and linking these results to measures of resident well-being. Knowing that sustained efforts to improve resident well-being are having the desired outcomes will be important.
Limitations
Survey data are cross-sectional, so causal associations cannot be made. Self-selection and social desirability bias are possible with self-report data. Though the resident response rate was low, the sample was representative of geographic region, program size, and AAFP and ACGME resident demographics. PD and resident response rates were markedly different; however, they appeared to represent the same program population based on program characteristics (type and size).
Residency program directors reported offering and emphasizing evidence-based wellness curricula. However, residents identified a lesser amount of implementation and emphasis on wellness programs. Resident satisfaction was associated with emphasis on wellness but not on available resources. Our study suggests the value of regular communication from PDs to residents, encouraging them to access resources to support well-being. Consistent messaging that is supportive of residents engaging in wellness programs has the potential to enhance resident perceptions of wellness. Therefore, future research could explore reductions in differences between resident and PD perspectives on wellness and ultimate improvement in resident wellness measured objectively.
Acknowledgments
Dr Kulshreshtha acknowledges his NIH grant 1K23AG066931-01A1.
The authors acknowledge Jessica Hauser-Harrington, PhD; Mary Talen, PhD; and Valerie Ross, MS, for their contributions to this study.
Presentations:
Results of this study were presented at the 2022 Society of Teachers of Family Medicine Annual Spring Conference in Indianapolis, Indiana.
References
- Thomas NK. Resident burnout. JAMA. 2004;292(23):2,880-2,889. doi:10.1001/jama.292.23.2880
- Mian A, Kim D, Chen D, Ward W. Medical student and resident burnout: a review of causes, effects, and prevention. J Fam Med Dis Prev. 2018;4(4):094. doi.org/10.23937/2469-5793/1510094
- Accreditation Council for Graduate Medical Education. ACGME Common Program Requirements (Residency). Updated March 2022. Accessed July 7, 2023. https://www.acgme.org/globalassets/PFAssets/ProgramRequirements/CPRResidency_2022v2.pdf
- Seehusen DA, Mainous AG III, Chessman AW. Creating a centralized infrastructure to facilitate medical education research. Ann Fam Med. 2018;16(3):257-260. doi:10.1370/afm.2228
- Kolarik RC, O’Neal RL, Ewing JA. Resident preferences for program director role in wellness management. J Gen Intern Med. 2018;33(5):705-709. doi:10.1007/s11606-018-4367-0
- Lawson ND. Wellness and work: mixed messages in residency training. J Gen Intern Med. 2020;35(2):594. doi:10.1007/s11606-019-05018-2
- Ey S, Moffit M, Kinzie JM, Choi D, Girard DE. “If you build it, they will come”: attitudes of medical residents and fellows about seeking services in a resident wellness program. J Grad Med Educ. 2013;5(3):486-492. doi:10.4300/JGME-D-12-00048.1
- Winkel AF, Nguyen AT, Morgan HK, Valantsevich D, Woodland MB. Whose problem is it? the priority of physician wellness in residency training. J Surg Educ. 2017;74(3):378-383. doi:10.1016/j.jsurg.2016.10.009
- Buchholz AL, Henderson F Jr, Lowe S, et al. Perspectives from a residency training program following the implementation of a wellness initiative. World Neurosurg. 2018;119:e947-e955. doi:10.1016/j.wneu.2018.08.009
- Schneiderhan J, Bishop T, Guetterman TC, Dobson M. Faculty and resident oerspectives of the complexity of wellness program implementation: a qualitative exploration. PRiMER. 2023;7:16. doi:10.22454/PRiMER.2023.413534
- Penwell-Waines L, Cronholm PF, Brennan J, et al. Getting it off the ground: key factors associated with implementation of wellness programs. Fam Med. 2020;52(3):182-188. doi:10.22454/FamMed.2020.317857
- Nasirzadeh Y, Chertkow L, Smith S, Ho C, Fefergrad M, Chaukos D. What do residents want from wellness? a needs assessment of psychiatry residents to inform a residency wellness strategy. Acad Psychiatry. 2022;46(2):254-258. doi:10.1007/s40596-021-01578-w
- Chaukos D, Zebrowski JP, Benson NM, et al. “One size does not fit all”—lessons learned from a multiple-methods study of a resident wellness curriculum across sites and specialties. BMC Med Educ. 2021;21(1):576. doi:10.1186/s12909-021-02995-z
- Fortenberry KT, Van Hala S, Frost CJ. Establishing a culture of intentional wellness: lessons from a family medicine resident focus group. PRiMER. 2017;1:12. doi:10.22454/PRiMER.2017.597444
- Grace A, Brennan J, Buck K, et al. Wellness in the time of COVID: a CERA follow-up survey of program directors. Fam Med. 2022;54(9):713-717. doi:10.22454/FamMed.2022.394088
- Shokar N, Bergus G, Bazemore A, et al. Calling all scholars to the Council of Academic Family Medicine Educational Research Alliance (CERA). Ann Fam Med. 2011;9(4):372-373. doi:10.1370/afm.1283
- Holmes EG, Connolly A, Putnam KT, et al. Taking care of our own: a multispecialty study of resident and program director perspectives on contributors to burnout and potential interventions. Acad Psychiatry. 2017;41(2):159-166. doi:10.1007/s40596-016-0590-3
- Penwell-Waines L, Runyan C, Kolobova I, et al. Making sense of family medicine resident wellness curricula: a Delphi study of content experts. Fam Med. 2019;51(8):670-676. doi:10.22454/FamMed.2019.899425
- Association of American Medical Colleges. AAMC Report on Residents. 2021. Accessed July 26, 2023.https://www.aamc.org/data-reports/students-residents/interactive-data/report-residents/2021/table-b5-md-residents-race-ethnicity-and-specialty
- American Academy of Family Physicians. Demographic Characteristics of AAFP Members. December 31, 2020. Accessed July 26, 2023.https://www.aafp.org/about/dive-into-family-medicine/family-medicine-facts/table2.html
- Morgan HK, Winkel AF, Nguyen AT, Carson S, Ogburn T, Woodland MB. Obstetrics and gynecology residents’ perspectives on wellness: findings from a national survey. Obstet Gynecol. 2019;133(3):552-557. doi:10.1097/AOG.0000000000003103
- Daskivich TJ, Jardine DA, Tseng J, et al. Promotion of wellness and mental health awareness among physicians in training: perspective of a national, multispecialty panel of residents and fellows. J Grad Med Educ. 2015;7(1):143-147. doi:10.4300/JGME-07-01-42
- Lefebvre D, Dong KA, Dance E, et al. Resident physician wellness curriculum: a study of efficacy and satisfaction. Cureus. 2019;11(8):e5314. doi:10.7759/cureus.5314



There are no comments for this article.