Background and Objectives: Bullying and harassment in medical education are common. The aims of this study were (a) to describe how medical trainees respond to harassment or bullying in medical settings, and (b) to determine whether trainees respond differently based on the type of harassment.
Methods: Participants were medical students, residents, and fellows (N=80) recruited from a rural teaching hospital in Pennsylvania. We invited them to complete an electronic survey and react to four standardized situations that included common harassment types in graduate medical education.
Results: On average, 31.6% reported that they would consult with peer colleagues, 50.6% would provide direct support to the victim, 16.3% would approach the perpetrator or intervene directly, and 19.3% would file a formal report with a supervisor or human resources. Findings indicated that respondents as bystanders would intervene significantly more often when harassment was related to inappropriate racial or ethnic comments.
Conclusions: Given that a sizable portion of trainees would speak directly with a victim, training bystanders in strategies to address or mentor others on how to address harassment more effectively could be useful in graduate medical education. Future research might explore trainees’ differential reactions to harassment types toward developing more comprehensive intervention programs in graduate and undergraduate medical education.
Bullying and harassment in medical education are common. Meta-analyses have suggested that nearly 60% of medical trainees have experienced at least one form of harassment or discrimination during training.1 Typical forms of bullying behavior include repeatedly reminding someone of mistakes, shouting, withholding important information, expressing hostility, and/or persistently criticizing.2 Evidence has suggested that bullying behaviors and harassment are more commonly directed toward females, and the most common forms of discrimination and harassment are related to racial and gender identity.1
Hostile work environments have numerous negative consequences. Bullying in residency is associated with a negative impact on the learning environment, reduced patient safety, a reluctance to ask questions, and reduced self-confidence.3 Bullying also negatively impacts health; health care professionals who have experienced hostile work environments have reported increased depression, burnout and psychological distress, sleep disturbance, headaches, and gastrointestinal symptoms.4 This impact is especially concerning among medical trainees, who have reported higher rates of depression and other mental health difficulties.5 Residents who are frequently bullied have reported higher rates of burnout (61.1% vs 37%), increased suicidal ideation (10.4% vs 3.1%), and thoughts of attrition (28.2% vs 7.8%)2 compared to those who have not been bullied.
Medical residents may be reluctant to report bullying, and 86.4% of residents who witness bullying do not report the behavior.6 To date, research has not investigated bystander responses to bullying or harassment in medical education outside of formal reporting mechanisms. The aims of this study were (a) to describe how medical trainees respond to harassment or bullying in medical settings, and (b) to determine whether trainees respond differently based on the type of harassment.
Participants were medical students, residents, and fellows recruited from a rural teaching hospital in Pennsylvania. We invited them to complete an electronic survey via SurveyMonkey in exchange for a coffee voucher. All procedures performed were approved by the Institutional Review Board of the associated medical group.
We asked respondents to provide demographic information and to read four brief vignettes that described situations depicting the most common harassment types in medicine (eg, gossip, exclusion, discrimination/inappropriate comments, excessive criticism).2 The vignettes asked respondents to “imagine you are on one of your usual rotations conducting your usual work.” All scenarios positioned the victim as a peer and the perpetrator as an attending physician. After reading each vignette, respondents were asked to indicate various ways in which they might respond up to 48 hours after the event, including not intervening (eg, would say/do nothing and continue with their day), keeping a record of events in writing, consulting with peers, providing support/empathy/problem-solving to the victim, directly addressing/intervening during the event, and/or filing out a formal report. Respondents were allowed to select more than one response because numerous actions are possible following a negative event. We examined responses categorically to allow for frequency analysis of response patterns, and we also weighted and summed the responses to provide a total intervention score (0=no intervention, 5=filing a report with human resources). Higher scores indicated more active or intense intervention.
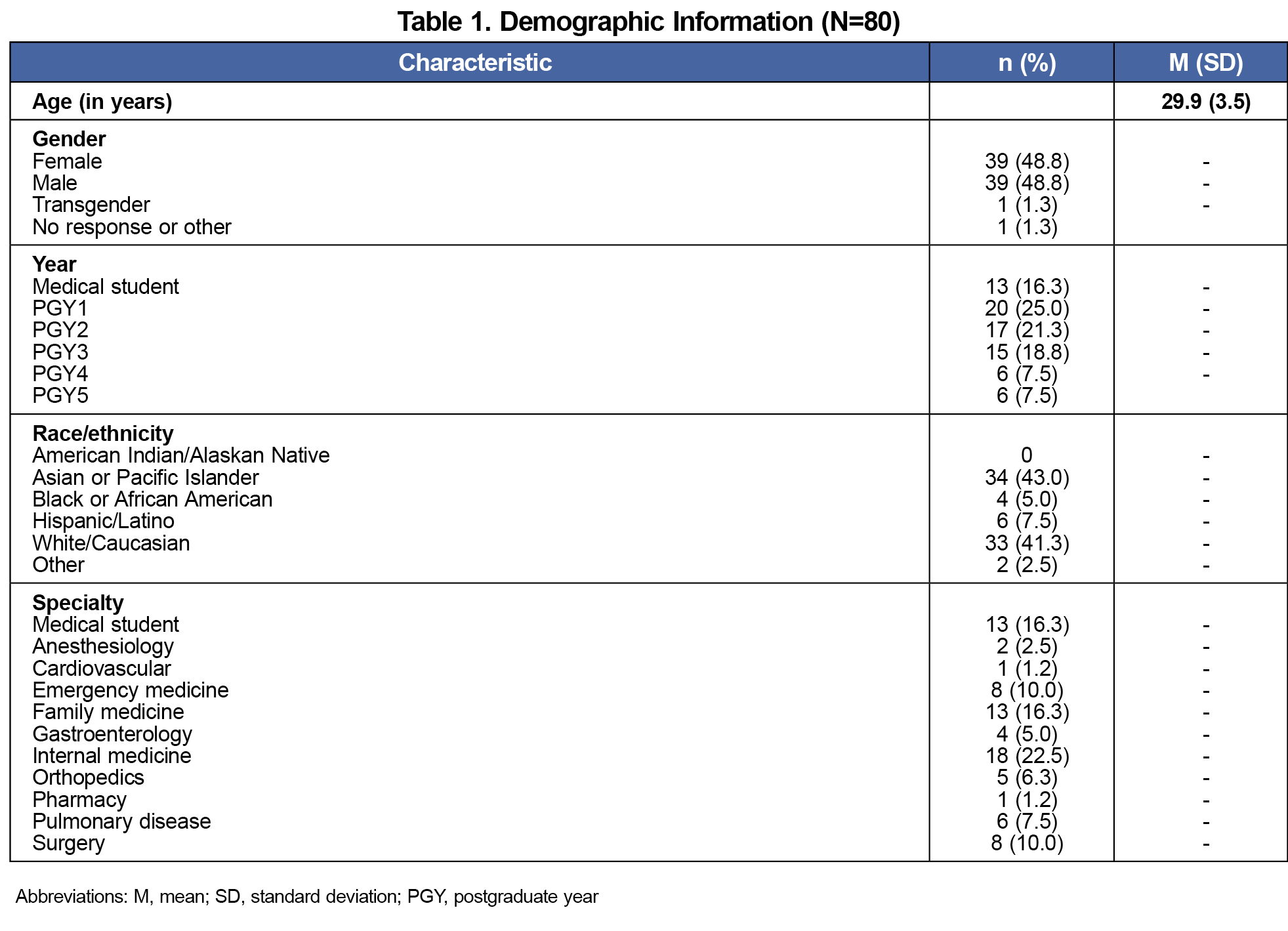
The sample included 80 participants (49.7% response rate). See Table 1 for a list of demographic characteristics by sample.
We calculated percentages of trainees endorsing bystander reactions for the four harassment types. Across all types of harassment or bullying, 14.5% to 26.5% of respondents indicated that they would not do anything if they were bystanders to bullying. Respondents were least likely to report that they would create a record of events (2.4%–12.0%). On average, 31.6% reported that they would consult with peer colleagues, 50.6% would provide direct support to the victim, 16.3% would approach the perpetrator or intervene directly, and 19.3% would file a formal report with a supervisor or human resources.
We performed a repeated-measures analysis of covariance to compare the within-subjects’ variable of harassment/bullying type on bystander intervention intensity, while controlling for gender and race/ethnicity. We found a statistically significant difference in intervention by harassment type (F[3, X]=3.87, P<.01, η2=.05). Specifically, bystanders indicated that they would initiate more intense intervention if the bullying or harassment was related to discrimination/inappropriate comments (M=3.45, SD=2.43) compared to other types of harassment (M=2.78, SD=2.02). We found no independent effect of race/ethnicity or gender on intervention intensity.
Bullying is very common in a medical culture.1 Our study yielded novel findings that add to the literature on bullying in medical education. Consistent with previous research,6 the majority (80.7%) of trainees reported that they would not file a formal report if they witnessed bullying or harassment. However, about half of residents indicated that they would provide direct validation and/or peer support to the victim. Given that a sizable portion of trainees would speak directly with a victim, training bystanders in strategies to address or mentor others to effectively address harassment would be useful in graduate or undergraduate medical education. In other graduate mentorship programs, students who participate in this type of programming benefit academically, socially, psychologically, and professionally.7 Future research might examine the impact of similar programs in medical education that target bystander interventions related to bullying and harassment.
Notably, bystanders were most active when harassment was related to inappropriate racial or ethnic comments. A reason for this finding might be that certain groups have protected rights that can result in legal consequences, and comments related to race/ethnicity may be perceived as more actionable (see https://www.eeoc.gov/discrimination-type). Due to the legal protections and greater cultural sanctions against racism, trainees possibly may feel more empowered to address harassment directly without fear of retaliation. Future research might explore trainees’ differential reactions to harassment types to help to develop more comprehensive intervention programs against all forms of workplace harassment.
This study had several limitations. First, it was limited by its sample size, and generalizability may be limited by the rural location. Future studies across more diverse geographic regions such as urban versus rural settings may reveal different patterns of bullying and bystander responses within medical education. Second, this survey did not include measures of actual behavior, which may have resulted in overestimations of helping behavior, consistent with socially desirable responses. Third, this survey also included a significant proportion of medical students rotating at the site. Further research might delineate differences between graduate and undergraduate patterns of bystander reactions because bullying may manifest differently depending on the level of training. Additional research should include multiple residency sites and may benefit from including attending physician perceptions and intervention strategies. Although this study focused on individuals most directly impacted by bullying, further research also could continue to examine the role that faculty and institutional leadership have in perpetuating and addressing these issues.
Given the high prevalence of harassment and bullying and their damaging effects on medical trainees, understanding patterns of bystander responses and developing strategies for intervention are paramount. These findings add to the literature by examining more subtle ways to influence medical education and suggesting areas for further study.
References
- Fnais N, Soobiah C, Chen MH, et al. Harassment and discrimination in medical training: a systematic review and meta-analysis. Acad Med. 2014;89(5):817-827. https://journals.lww.com/academicmedicine/Fulltext/2014/05000/Harassment_and_Discrimination_in_Medical_Training_.34.aspx
- Zhang LM, Ellis RJ, Ma M, et al. Prevalence, types, and sources of bullying reported by US general surgery residents in 2019. JAMA. 2020;323(20):2,093-2,095. doi:10.1001/jama.2020.2901
- Paice E, Smith D. Bullying of trainee doctors is a patient safety issue. Clin Teach. 2009;6(1):13-17. doi:10.1111/j.1743-498X.2008.00251.x
- Lever I, Dyball D, Greenberg N, Stevelink SAM. Health consequences of bullying in the healthcare workplace: a systematic review. J Adv Nurs. 2019;75(12):3,195-3,209. doi:10.1111/jan.13986
- Pereira-Lima K, Mata DA, Loureiro SR, Crippa JA, Bolsoni LM, Sen S. Association between physician depressive symptoms and medical errors: a systematic review and meta-analysis. JAMA Netw Open. 2019;2(11):e1916097. doi:10.1001/jamanetworkopen.2019.16097
- Wolfman DJ, Parikh JR. Resident bullying in diagnostic radiology. Clin Imaging. 2019;55:47-52. doi:10.1016/j.clinimag.2019.01.024
- Lorenzetti DL, Shipton L, Nowell L, et al. A systematic review of graduate student peer mentorship in academia. Mentor Tutoring. 2019;27(5):549-576. doi:10.1080/13611267.2019.1686694



There are no comments for this article.